Editor's note: This text-based course is an edited transcript of the webinar, Documentation in Social Work for Private Practitioners, presented by Gabrielle Juliano-Villani, MSW, LCSW.
Learning Outcomes
After this course, participants will be able to:
- Create clear and concise progress and chart notes that accurately incorporate the contents of the mental health assessment.
- Create effective and efficient treatment plans with clients.
- Develop progress notes and treatment plans that meet insurers' standards.
- Consider the role of ethics in social work documentation.
Introduction
I am excited to be back again doing another presentation on a much-needed topic we do not discuss too often. Documentation is a huge part of social work, especially in private practice. I train folks on how to write progress notes and treatment plans. I have worked in child protection, where documentation was essential because they were court-ordered. I also have had to document very specifically to meet Medicare standards at a previous job. Now, I am in private practice, and we have been audited by Medicaid and other insurers several times. I gathered much of what I am discussing today from that audit and information learned over the years. Thus, I feel like I am well-versed in this topic.
Cultural Competence
For additional information regarding standards and indicators for cultural competence, please review the NASW resource: Standards and Indicators for Cultural Competence in Social Work Practice https://www.socialworkers.org/LinkClick.aspx?fileticket=7dVckZAYUmk=&portalid=0
Why Document?
- How is it used?
- How long does it need to be kept
- Who will read it
- Audit
- Disability
- Workman's comp
- Subpoenas
- DHS
- Clients
- Grievances
- Us
I often hear, "I'm in private practice and don't take insurance or keep notes." It is not just about insurance. Ethically, we are required as social workers, as are all other disciplines, to keep notes. Our documentation can be used for a lot of different things. Especially in private practice, nobody will read your notes unless you get audited, or you get grieved against, but we still need to document as if somebody were going to read it. I think about what I would say if an attorney were reading over my shoulder. I learned from child protection because that does happen. You also want to be vague, but not too vague, and we will cover that today.
Documentation is also critical if an insurance company audits you. They will read it and check it for medical necessity to ensure that no fraud occurs. They also want to ensure you are seeing the client because many issues are seen in Medicare and Medicaid billing, although not usually by social workers. You also give your notes to SSDI if someone is applying for disability. We have been getting many requests throughout the pandemic. I did one yesterday. Disability will want to see all of the notes on the client. Occasionally, they will accept a summary, but usually, they want progress notes and treatment plans. Workman's comp and short-term disability are other areas where they will want to see those notes. Documentation will need to support that an individual is struggling and how that affects their ability to work. If you have a client with an open case with DHS or any court case, your documentation might be subpoenaed for that case. Documentation is also needed for medical necessity to understand your client and their issues better. Clients own the record, and sometimes people forget that. A client may also request your notes. Of course, a grievance or a complaint requires your documentation. Lastly, we also document for us so we can remember week by week what our clients are working on and what they are saying and show the progress that clients have made.
Documentation needs to be kept for usually seven years and can vary state by state and board by board, but in Colorado, it is seven years that we have to keep those records. Even if clients are no longer active on our caseload, we will keep their records. You do that through an electronic health record or paper notes in a filing cabinet.
NASW Code of Ethics
- Section 3.04 Social Workers' Ethical Responsibilities in Practice Settings
- (a) Social workers should take reasonable steps to ensure that documentation in electronic and paper records is accurate and reflects the services provided.
- (b) Social workers should include sufficient and timely documentation in records to facilitate the delivery of services and to ensure continuity of services provided to clients in the future. (NASW, 2021)
- (c) Social workers' documentation should protect clients' privacy to the extent that is possible and appropriate and should include only information that is directly relevant to the delivery of services.
Our code of ethics requires us to document. We need to take reasonable steps to ensure that documentation in electronic and paper records is accurate and reflects the services provided. Again, this does not just protect our clients and their privacy, but it also protects us. If something were to happen, we want to show that we were seeing this person, and this was our intervention. I am not trying to scare everybody with these scenarios, as they rarely happen. But, if we do it on the front end and take thorough and timely notes, we do not have to worry about it later.
Our documentation should be timely and sufficient to facilitate delivery and ensure client service continuity. So we also have an obligation to future providers as well. "Here's where we left off, what we did and didn't do."
We should also protect clients' privacy to the extent possible and include only information directly relevant to the delivery of services. We want to be somewhat vague. For example, we do not need to say that our client told us their best friend Marsha was selling drugs on this corner. We do not need to document all of these specifics. We could say instead that our client is feeling anxious in her relationship with her best friend. We do not need to put every detail in there as the insurance company does not need to know that information. For example, they only need to know that the client is dealing with anxiety and relationships and how we responded.
Another helpful thing that I learned through my Medicaid audit is to use assessments because that backs up the evidence for medical necessity. For example, you can use the GAD7 (General Anxiety Disorder-7), the PHQ9 (Patient Health Questionnaire-9), et cetera to show the work you did up front to identify their diagnosis.
You also want to ensure that your practice policies and form consents are signed. This practice may vary depending upon insurance and state, but Medicaid and Colorado want the treatment plan and the initial mental health assessment intake signed by the client. I would suggest you do that for everybody to cover yourself and make sure clients are informed about the services they are getting and how we got to their diagnosis.
Assessments
- Use GAD7, PHQ9, PCL5, etc.
- Make sure all policies and consents signed
- Medicaid typically wants treatment plans, and the initial assessment signed.
People call an assessment a couple of different things. I usually call it an intake, and Medicaid calls it a mental health assessment. An intake is the first time you meet somebody; it is usually the longest session.
Each insurer, including Medicaid and Medicare, has different assessment timeliness and update guidelines. Medicaid in Colorado wants us to schedule clients within a week of when they contact us, and you need to sign notes within 48 hours. Completion of a treatment plan is 30 days, so that is what I follow. Medicaid guidelines are the most stringent, so we should be fine if we base everything on their rules. I am sure everybody watching this has been behind on their notes before. I try to get my documentation done as soon as possible, so they do not pile up.
Components of Assessment
- Assessment timeliness, updates
- Barriers to tx
- Chief complaint/ problem statement
- Complete MSE
- Dx- meets DSM criteria
- Date/POS/Modality/Clinician Name/Signature
- Complete biopsychosocial (can be gathered from other sources)
I want to go through the assessment components because this is what insurers want. If you check all these boxes from the list above, you should be okay with an audit or any other reason somebody might want to look at your notes. You usually get this information when you first meet with them.
If this client returns, you will want to update your assessment with any new information. First, we start with the question, "Why are you here?" or, "What's going on?" Their answer will be their chief complaint or problem statement.
You will also want to note any barriers to treatment. There may be cognitive deficits or logistics like they do not have a computer or a bus pass. You will want to document those as well.
Each insurer, including Medicaid and Medicare, has different guidelines on assessment timeliness and updates. Medicaid in Colorado wants us to schedule clients within a week of when they contact us, and our notes need signing within 48 hours. A treatment plan needs to be completed within 30 days, so that is what I base my timelines on, as Medicaid guidelines are the most stringent. If we base everything on their rules, we should be fine.
I am sure everybody watching this has been behind on their notes before. I try to get my documentation done as soon as possible, so they do not pile up.
An MSE (Mental State Examination) should always be completed. You also want to talk about their mood, affect, how they were dressed, if everything was within normal limits, and their diagnosis. You can do some of that before you meet with them. I like sending clients the assessments, like the PHQ-9 and the GAD-7, ahead of time. If I think they are coming to me for PTSD, I will also send them the PCL-5 (Posttraumatic Stress Disorder Checklist for DSM-5).
Usually, from their chief complaint, you can start to understand what their diagnosis might be, but you want to make sure it meets the DSM criteria. I copy and paste the symptoms they are telling me from the DSM. That way, it is all right there and using the DSM-specific language.
You will want to have the assessment's date and place of service. You must document if it was telehealth or if you met with somebody in the community, at their home, or in your office. You also want to include any modalities that you used. However, intervention is not typically done in an assessment, so you do not need to say that you did CBT (cognitive behavioral therapy) or anything like that. Make sure that it is signed with your name and credentials.
A biopsychosocial summary should include the clients' work, legal, military, and family histories. You can gather this information from other sources if needed. Medicare puts this in its guidelines. One example would be collecting a child's history from their doctor, referral source, or parents. I document, "Parents are reporting this," or "The referral came from a social worker in home healthcare, and they are saying this."
- Risk assessment - HI/SI ◂ Safety plan
- Medical and psychiatric hx
- Psychiatric/MH hospitalization hx
- Readiness for admission
- Substance abuse
- Duration and start/end time
- Plan for next contact and any follow-up
- Legible!
During a risk assessment, you must determine if there is any homicidal or suicidal ideation and make sure you document that. I am very blunt about this question. Sometimes people ask me about how I assess for that. I usually frame it as me getting to know the client. "I need to know if you have any homicidal or suicidal ideation." They might initially say no, but make some concerning statements during the conversation. I will then need to reassess that. If they report anything, you want to document a safety plan and put it into their chart.
You also want to ensure you are documenting if they have had any psych hospitalizations. I may ask, "Have you been in therapy before? Were you diagnosed with anything at that time? What did that look like?" If you are working with mandated clients and looking at readiness for admission, they might never be ready. However, we should document the stage of change and if they are appropriate or not appropriate for treatment. We then need to note if we are referring them out and why.
If there is any substance abuse, we need to document that. We need to know if we are a good fit for them. In my practice, we do not have many people with substance abuse experience, so we refer cases out.
You must document the start and the end time as all insurances want to know the duration. This is also how we bill and where a lot of fraud happens. We want to bill appropriately for that time. They are very picky in Colorado and want to know the precise times. If you did not start your session until 2:03 PM, you put 2:03 PM and exactly when you ended.
Are you going to be seeing this client weekly? Are you seeing them next week? Are you seeing them on March 14th, 2022? Put those dates and any other follow-up with third parties they may need. If you need to get a release of information signed or if you already have one signed for their case worker, you need to follow up with the caseworker about them.
All documentation needs to be legible. Poor handwriting is not an excuse if you do not use an electronic health record. Your notes need to be able to be read. Again, this not only protects the client, but it also protects you. It shows that you met with them and your interventions so that you can get paid for your time.
- Support with medical necessity
- Medication
- Client's name on pages/record
- Document their ability/willingness to adhere to tx plan
- How and why do they meet criteria for this level of care?
- Impact on functioning
Insurances want to know that everything you are doing is medically necessary or that they will not pay for it. I always ask clients to give me their med list so that we have that, especially for Medicare and Medicaid.
Other tips to help you pass an audit include ensuring the client's name and date of birth are on their record or any pages. If you use an electronic health record, it will do this for you. You also want to document their ability and willingness to adhere to the treatment plan. I will talk about that a little bit more later. We do not want to give clients unrealistic treatment plan goals they will never meet because their treatment will not be covered. You also want to document how they meet this level of care criteria. Are they meeting you for outpatient therapy once a week, or is this somebody in crisis and struggling with suicidal ideation and self-harm? If so, this might be more appropriate for intensive outpatient or even hospitalization, depending on the situation. The impact on functioning is crucial to document. How does depression, anxiety, anger, or whatever impact their functioning? Are they not able to go to work or school?
How do we get to a diagnosis and treatment plan when 800 different things happen in their lives? We want to string all these components nicely together. It is called the golden thread. First, I ask about any previous diagnoses because that can be helpful. For example, they may have five different issues that they are having. I am going to look for themes and patterns. I might also ask the client to give me a problem list. Where are the problems in your life and the precipitants to this current episode?
I will often hear, "It came out of nowhere. I just started feeling this way." We all know that is not always true. I may ask, "What was going on when you started feeling this depression? What was the catalyst for that?" I hear things as my mom died or we moved. I ask about any current behaviors related to that so that I can understand it a little bit better.
How does hopelessness look? Does that mean you are sad or want to die? Or does that mean you are not getting out of bed? Beliefs, thoughts, and behaviors tie all of this together so we have a better understanding of how we can build their treatment plan.
We also want to know their goals. "What do you want to work on together? What will it look like when our work is done?" This can be a tricky question for people to answer. It was a hard question for me to respond to with my therapist. They may want to get on meds or get out of bed in the morning and not feel so sad. Knowing this information is a good starting place.
Case Conceptualization
- Make sure you are asking of any previous dx
- Look for themes and patterns
- Problem list
- Precipitants to current episode or to problem
- Current beliefs/thoughts
- Current behaviors
- What are their goals?
- How will we know when our work is done?
- Look for themes and patterns
This information helps us to conceptualize the case, especially with current events. An issue at work or conflict with their mom or boyfriend may cause anger or anxiety. I write these down because that helps me visualize everything and make a treatment plan. In my experience, that is not how it always works, but whatever their goal is ("get out of bed"), I will write that up in their language.
Treatment Plans
- Client participation
- Timeliness - usually within 30 days of first contact
- Treatment plans are:
- Measurable
- Specific, objective, realistic
- Culturally sensitive
- Individualized
- Strengths-based
Again, the treatment plan should be completed within 30 days of first contact. Goals need to be measurable, specific, objective, and realistic. If someone says, "I'm depressed, and I can't get out of bed and brush my teeth." We will not say, "Okay, your goal is to run a half marathon in the next six months." We need it to be realistic. Again, it might be something minimal, and that is fine.
Goals also need to be culturally sensitive. We can always be better as social workers. We want to examine the client's culture and how it relates to their diagnosis or goals.
They also need to be individualized as every person is unique. We will not have the same treatment plan for every client. Some clients are into meditating and using some mindfulness to manage their anxiety, and other clients do not. They may want to do something else like go for a run.
Goals should be strength-based. This type of treatment is ingrained in us as social workers, but we want to document it in a strength-based way. I learned a good lesson a long time ago working in child protection. I had written some things in a client's treatment plan that were not strength-based, as I was on autopilot and did not think about it. It was court-ordered, read in front of the client, and did not go over well. It was a good learning experience to slow down and make sure I use culturally sensitive and strength-based language.
SMART Goals
- S - Specific
- M - Measurable
- A - Attainable/Achievable
- R - Realistic
- T - Timely
**Wiley
It is vital to make your goals SMART. They must be specific, measurable, attainable, realistic, and timely. This helps us and others know when they have met them. How will they take steps to meet those goals if they are not specific, or how will they know if goals are satisfied if not measurable? If they cannot meet them, they are not achievable. Most will not be in treatment for 20 years, so the goals need to be timely.
I have a little note down here for Wiley. If you are in private practice, community mental health, or working with clients in therapy in some way, I highly recommend that you buy this book. It is $20 on Amazon and has a PDF version that comes on a CD-ROM (if you still have one of those). This is where I start the foundation for my treatment plan. Figure 1 is an example of a treatment plan that is not smart.
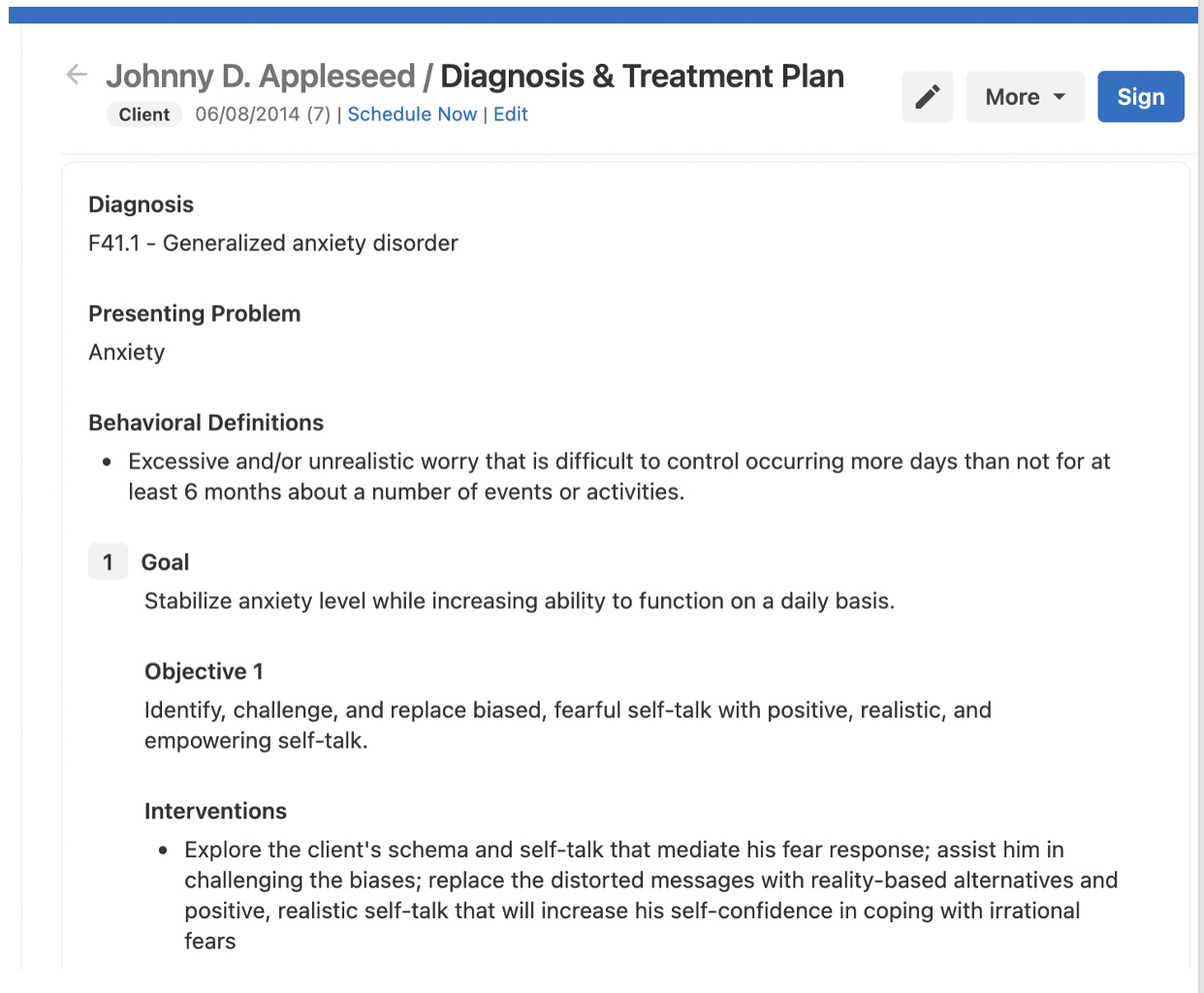
Figure 1. An example of a treatment plan with goals that are not smart.
This is a screenshot from my EHR (electronic medical record); obviously, Johnny Appleseed is a fake client. Every EHR is different; particularly in simple practice, you can easily make treatment plans. They have uploaded "Wiley" in there, which is fantastic. You can go from the diagnosis, and then you can click a bunch of checkboxes. However, they are not smart goals. Figure 2 is the same treatment plan with a smart goal.
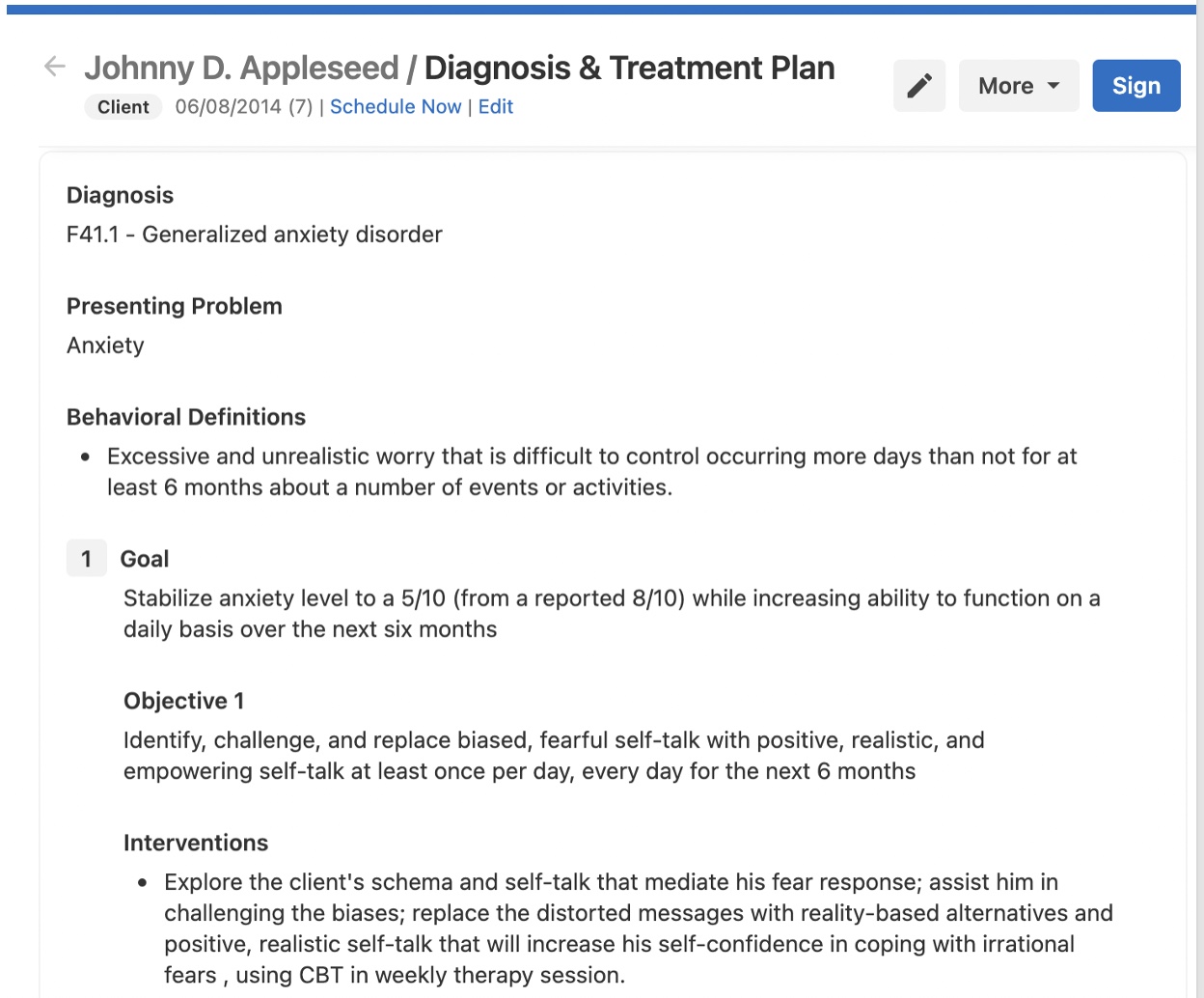
Figure 2. An example of a treatment goal that is smart.
The objectives are always more specific than the goals. The goal is bigger, the objective is smaller, and the interventions are how you will meet those. Let's take the example of Johnny Appleseed. He is seven years old and has a generalized anxiety disorder. The presenting problem is anxiety. He has excessive or unrealistic worry that is difficult to control, occurring more days than not for at least six months about several events or activities. It is written like this as it is part of the criteria for generalized anxiety disorder.
His goal is to stabilize his anxiety level while increasing his ability to function daily. But how, when, where, how often is he going to do that? We want to explore the client's schema and self-talk that mediate his fear response, assist him in challenging the biases, and replace the distorted messages with reality-based alternatives. Positive, realistic self-talk will increase his self-confidence in coping with irrational fears. To improve this, I can put in a scale to either increase or decrease the anxiety level.
Again, we want our treatment plans to be appropriate, individualized, and culturally sensitive for our clients. You do not need to spend hours upon hours writing unique treatment plans for each client. You can easily add in different language to make it individualized and smart. You can see that both EMRs have the same diagnoses, presenting problems, and behavioral definitions. The smart goal in the second one is to stabilize his anxiety level to a five out of 10 from a reported eight out of 10 while increasing his ability to function daily over the next six months. Previously, we did not have any of that in there as we were just going to stabilize his anxiety level. I also added that he reports his anxiety as an eight out of 10 daily. We want to get it down to a five out of 10, and we will do that every day for the next six months while we work together.
In the objective, I used the same language of "identify, challenge, and replace bias, fearful self-talk with positive, realistic, and empowering self-talk, but I added that he would do that at least once a day, every day for the next six months. That might be too much for someone, and I could downgrade it to three times a week, and he is going to report that to you.
I also added more specific language to the intervention. Previously, the client was going to increase his self-confidence when coping with irrational fears without documentation of how to do that. I added that we would do CBT (cognitive behavioral therapy) and weekly therapy sessions. These changes took me about four minutes to change on the EMR. I added different language to make it a smart goal.
As I mentioned earlier, I like to use a scale. For example, ask your client, "How bad is your anxiety on a day to day? What is the average?" They may say it is 20 out of 10. I may say, "Do you think you can get it to an 18 out of 10 when working with me? Use that with your clients, and then add the words increase and decrease.
Medical Necessity
- Healthcare services that a provider, using clinical judgment, would provide to a patient for the purpose of evaluating, diagnosing or treating an illness/disease
- In accordance with the generally accepted standards of medical practice
- Clinically appropriate, in terms of type, frequency, extent, site and duration, and considered effective for the patient's illness, injury, or disease; and,
- Not primarily for the convenience of the patient or physician, and not more costly than an alternative service or sequence of services at least as likely to produce equivalent therapeutic or diagnostic results as to the diagnosis or treatment of that patient's illness, injury, or disease. (Cigna)
I will switch gears to medical necessity, which is the basis for insurance, Medicaid, and Medicare. They need to see that something is medically necessary to cover it. As a social worker, I think medical necessity can be complicated and layered. We can certainly use our clinical judgment to best help our clients and show that services are medically necessary, just like MDs. Physicians will not automatically approve different meds or procedures because it would not be appropriate. The same thing happens to us, unfortunately. Medical necessity are services that a healthcare provider using clinical judgment would provide to a patient to evaluate, diagnose, or treat an illness or disease. In all our assessments, we use our clinical judgment to treat or diagnose our clients' mental concerns.
We also treat following accepted standards of medical practice. We probably would not see somebody coming to us for a moderate depressive episode or see them five times a week. That is, as far as I know, a type of treatment not generally accepted. If it was in an intensive outpatient facility and something deeper going on, then that may be an accepted standard of medical practice, and we would document that. Again, we would need to use our clinical judgment. This is the evidence the client is showing me, which is why it meets that level of care.
We also must ensure our treatment is clinically appropriate in terms of type, frequency, extent, site, duration, and considered effective for the patient's illness, injury, or disease. I had a client who was in crisis, and I had to see them twice a week. I ended up doing three sessions because we also had to do a family session. It was clinically appropriate with what was happening with that client, and we needed the family there. I made sure to document all of that. I do not do that level of treatment with other clients or every week. Still, it was appropriate when that client was specifically in crisis and needed that additional support to prevent a higher level of care.
You may not have your license at first, but you have your judgment. I do not want people to be afraid about everything I just said and feel empowered that you know what you are doing. I have been there many times with an insurance company pushing back on me. However, I am in control as I know what is happening with my client, and they are experts in what they need.
Your services cannot be for the convenience of the patient or the physician, nor can they be more costly than an alternative service. Insurance companies always want to pay for the least invasive level of care. They will ask why somebody has to go to an intensive outpatient or a partial hospitalization program.
- Evidence-based
- Views of healthcare providers practicing in clinical areas
- Specialty Society Recommendations
We must back up medical necessity using evidence-based practice, as we should in all treatments. CBT, DBT (dialectical behavioral therapy), and EMDR (eye movement desensitization and reprocessing) are all evidence-based and can be helpful. You can consult with other social workers, use a consulting group, collaborate with the client's primary care doctor, or see if NASW has some recommendations to back up medical necessity. I talk about medical necessity in every progress note that I write. We have a little check box that we use to deem why it is medically necessary. For example, "We need to see this client for a more extended session because we are doing internal family systems work, or "We're doing EMDR, and it's medically necessary because of new emerging symptoms to stabilize the client.
Expectations of Outpatient Treatment
- The therapist and individual will collaborate to establish clearly defined treatment objectives and to identify ways to measure improvement.
- From time to time, individuals may occasionally have other unresolved problems, but their level of functioning has been restored to baseline. The presence of unresolved issues does not necessarily indicate that continued outpatient therapy is medically necessary.
- The type and degree of functional impairment will be reflected in the treatment plan.
I also put in some expectations of outpatient treatment. I got these from United Healthcare. You and the individual collaborate to establish clearly defined treatment objectives and to identify ways to measure improvements. Hopefully, you can do that in the treatment plan with the client. If not, you are considering what they have told you and putting that into some clinical language.
Individuals might have unresolved problems, but their level of functioning has been restored to baseline. Or their baseline is a lot higher than you or the client would like, but that is their baseline. Unresolved issues do not necessarily indicate that continued outpatient therapy is medically necessary. You may have a lot of things to say about this, but they say something not resolved is not a reason to continue treatment. These scenarios happen all the time. Things might not get fixed, but they may now have better coping skills, so they do not need to see you anymore.
You also want to document the type, and degree of functional impairment as this will impact the client, so you want to put that in your treatment plan. We are hopefully reducing or alleviating the individual symptoms. For example, we may see their anxiety going from an eight to 10 to a five to 10, or we are getting them to their baseline or improving their level of functioning. You always want to get them to a higher level of care. "We need to meet with this client twice weekly to prevent them from a more intensive level of care."
I want to mention family therapy as I see this a lot. People ask, "How do you bill?" or "How do you work with a family if you are doing couples therapy?" If you want to bill insurance, that family unit is seen as the patient, but to play the game, you need to have an identified patient if you are doing family therapy.
Purpose of Outpatient
- Reduce or alleviate the individual's symptoms,
- Return individual to baseline or improve the level of functioning; and/or
- Prevent imminent deterioration that would lead to a need for admission to a more intensive level of care.
- Family- need identified patient
We are hopefully reducing or alleviating the individual symptoms. We may see their anxiety is going from an eight to 10 to a five to 10, or we are getting them to their baseline or improving their level of functioning. You always want to get them to a higher level of care. "We need to meet with this client twice weekly to prevent them from a more intensive level of care."
I want to mention family therapy as I see this a lot. People ask, "How do you bill?" or "How do you work with a family if you are doing couples therapy?" If you want to bill insurance, that family unit is seen as the patient, but to play the game, you need to have an identified patient with a diagnosis if you are doing family therapy. The work you are doing together needs to alleviate the client's issues.
Components of Progress Notes
- Nature and Frequency of services correspond to those ordered on the tx plan (document if a change is needed)
- DOS
- Place
- Time
- Duration
- Who is present
- CPT
- Signed with credentials
Progress notes have specific components to cover yourself and meet insurance standards for medical necessity. First, you need to have the nature and the frequency of services. These services need to correspond to what is on the treatment plan. This was a big one with my Medicaid audit. If we say that we are going to meet the client weekly in that treatment plan, and then we decide we will meet them every other week, we need to document that.
The date of service (DOS) is crucial. When did you see them and where? You also want to document the time and the duration. Again, if you started at 2:03 PM, put that on there. If you have an EHR, this does all that stuff for you. But if you are writing paper notes, you want to ensure that you are writing those timestamps down. Who was there? Was it just your client? Or did they have their mom or caregiver there? Who else is involved? The CPT code is the billing code. The EHR will do this for you as well. If you do not have one, you will have to write it on there. CPT billing could be a whole other training. Finally, it needs to be signed with your credentials, which is a specific requirement of Medicaid. If you get audited, they can easily see what you are working on, when, and how.
Each note refers to the goals and objectives from the current treatment plan being addressed in that session. When I type my note, we have check boxes and a narrative section where I say what we worked on and how the client responded. I also assign it to a particular goal like, "Per goal one, objective two of the treatment plan." I say that in every single note, and then I just leave it every week, or if we are working on something else, I change it.
Clinical interventions and techniques also need to be in your progress note. I also have check boxes for these and a note template I made. I include psychoeducation EMDR, CBT thought record, DBT distress tolerance skills, IFS work, ACT, and Gottman on those boxes. You can add whatever you do to the record along with the client's response to that. They may be into it and want to add some meditation, or they may resist and say, "I don't want to do that." I document all of that.
If you need an interpreter, you also want to document that. I mentioned earlier that you must always document suicidal or homicidal ideation ethically and for liability. If somebody talks about suicidal ideation the prior week, and then you do not document the next week, that will be a problem. You want to ensure you are addressing that issue until it resolves. If they are feeling better this week, you need to document that and note if this is resolved or if you are still working on it.
A referral is needed if they discuss medical, dental, or substance abuse issues. We do not want to cross the line by giving medical advice. However, we need to document and refer or empower the client to do that independently.
If somebody does not show up or drops out of services, you want to document that you reached out to them because there is a liability if something happens. "This client no-showed last Tuesday. I called them on Tuesday and left a message but didn't hear back. I called them again on Wednesday and sent them a text, but I didn't hear back. Thursday, the client texted and apologized and said that they were in the hospital." It is essential to cover yourself.
Summary
You want to make sure that you have all of that stuff documented. And that is it. Thanks for attending.
Questions and Answers
What typically prompts an audit?
It can be a lot of different things. Some people never get audited, and some people get audited more often. Usually, they just randomly select people like every quarter. I know Anthem does this. Some things can be a red flag. If you are billing a lot and seeing a client two or three times a week for months, this might initiate an audit. Another reason could be the types of billing codes that you use. There are normal billing codes, and then there are a bunch of add-ons that you can do to get some extra money if there is a crisis or you need a longer assessment. Using those add-on codes may also trigger an audit.
What are some common mistakes you see in the documentation that social workers can avoid?
A common mistake is not putting the exact duration. This is the number one issue in fraud cases, specifically with Medicare billing. I cannot emphasize enough to document the start and end times. Social workers also need to ensure that the codes match. Each note also needs to refer to the goal and objectives of the current treatment plan. Many do not do that every single time, but it will cover you if an issue arises.
Should there be a two-factor authentication if we use an electronic medical system? And do paper records need to be behind a lock?
If you are keeping paper records in Colorado, it needs to be behind two locks. My documentation is in a locked filing cabinet and a locked office. Electronic documentation should be encrypted. I also back up data in case something ever happens.
You spoke about case conceptualization. What is the best practice for conceptualizing a case or articulating that in writing? We want to ensure we are not giving too much but clearly articulating what is happening with our client.
I do not document every detail, but I will write down what they report to me. I always think about the impact on functioning and focus on behaviors, patterns, symptomology, and how that impacts their functioning.
References
Boylan, M. Teays, W. (eds.) (2022). Ethics in the AI, technology, and information age. Rowman & Littlefield Publishers.
Cigna Standards and Guidelines for Medical Necessity. (2020, April). Cigna for Health Care Providers. https://www.cigna.com/static/www-cigna-com/docs/health-care-providers/medicalnecessitycriteria.pdf
Kivistö, M. & Hautala, S. (2020). Structuration processes of client-oriented and system-oriented social work practice: The viewpoint of client documentation. Nordic Social Work Research. DOI:10.1080/2156857X.2020.1848907
Merrill, C. A., Maheu, M. M., Drude, K. P., Groshong, L. W., Coleman, M., & Hilty, D. M. (2022). CTiBS and clinical social work: Telebehavioral health competencies for LCSWs in the age of COVID-19. Clin Soc Work Journal. https://doi.org/10.1007/s10615-021-00827-7
Miller, C. A. (2021). Social work documentation: A guide to strengthening your case recording, 2nd edition. Nancy L. Sidell. Social Work, 66(1), 84. https://doi.org/10.1093/sw/swaa044
Nadler, L. E., Ogden, S. N., Scheffey, K. L., Cronholm, P. F., & Dichter, M. E. (2021). Provider practices and perspectives regarding collection and documentation of gender identity. Journal of Homosexuality, 68(6), 901–913. https://doi.org/10.1080/00918369.2019.1667162
National Association of Social Workers (NASW). (2021). NASW - National Association of Social Workers. https://www.socialworkers.org/About/Ethics/Code-of-Ethics/Code-of-Ethics-English
Reamer, F. G. (2005). Documentation in social work: Evolving ethical and risk-management standards. Social Work, 50(4), 325–334. https://doi.org/10.1093/sw/50.4.325
Savaya, R. (2010). Enhancing student awareness of the importance of full and accurate documentation in social work practice. Social Work Education, 29(6), 660-669. DOI: 10.1080/02615470903552006
Schwartz, A. L., Chen, Y., Jagmin, C. L., Verbrugge, D. J., Brennan, T. A., Groeneveld, P. W., & Newhouse, J. R. (2022). Coverage denials: Government and private insurer policies for medical necessity In Medicare. Health Affairs, 41(1), 120–128. https://doi.org/10.1377/hlthaff.2021.01054
Singh, S., Kolinski, J., Alme, C., & Sinson, G. (2022). The growing epidemic of insurance denials: A frontline perspective. Journal of Hospital Medicine, https://doi.org/10.1002/jhm.2775
Zerden, L. de S., Lombardi, B. M., Richman, E. L., Fraher, E. P., & Shoenbill, K. A. (2021). Harnessing the electronic health record to advance integrated care. Families, Systems & Health: The Journal of Collaborative Family HealthCare, 39(1), 77–88. https://doi.org/10.1037/fsh0000584
Citation
Juliano-Villani, G. (2022). Documentation in social work for private practitioners. Continued Social Work, Article 160. Available from www.continued.com/social-work
