Editor's note: This text-based course is an edited transcript of the webinar, Administration of Medication in ECE Settings, in partnership with Region 9 Head Start Association, presented by Charlotte Hendricks, PhD.
Learning Outcomes
At the conclusion of this course, participants will be able to:
- Identify circumstances that may require administration of medication on site.
- List six "rights" of assisting with medication.
- Describe safety measures in handling, storing, and disposing of medication.
There are two handouts for this course. One is a sample authorization form and the other one is information on the six rights. If you haven't downloaded those, you may wish to do that, as we will be discussing those later.
What Is a Medication?
Medication is a substance taken into or placed on the body used to:
- Cure a disease or condition (e.g., antibiotic)
- Treat a condition (e.g., insulin)
- Relieve symptoms (e.g, acetaminophen)
- Prevent disease (e.g., vaccine)What is a medication? It's any substance that is taken into or placed on the body to cure a disease or condition, to relieve symptoms, or to prevent disease. One example of a medication to treat a condition is an antibiotic. Another example is insulin, which would treat the condition of diabetes. An example of a medication to relieve symptoms is acetaminophen which many people commonly know as Tylenol. This medication would be used for pain or fever. An example of a medication to prevent disease is a vaccine. Medications can be either prescription, which is the Rx symbol, or what we call Over-the-Counter, or OTC drugs. Those are drugs that do not require a physician's prescription and you can just go into a drugstore or grocery store and purchase those.
Policy on Giving Medication
Must have written instructions from health care provider and written parent permission:
- Prescribed medication (Rx or OTC) with scheduled dosages required during program hours
- One-time or short-term medications
- Long-term medication for chronic or special health care needs
- Emergency medications
In early childhood settings, Head Start programs, family child care homes, and any other kind of early child care setting, there may be times that you will be getting medication. The goal is to not give medication because there are always problems that can occur and there are certain risks with it but there are times when you will need to give medication for children's well-being. First of all, you need to think about when you would give those medications. We'll go over some of the possible scenarios of when you would.
Before you do anything around giving medication, think about what's in your written policy. First, you must have written instructions from the healthcare provider, that is the child's doctor or a nurse practitioner or health clinic, and you must have written parent permission. If it's a prescribed medication, whether it's a prescription one or an over-the-counter one that has scheduled dosages required during the program hours, then you have to give the medication while the child is in your care. Now notice the difference there. I say it's a prescribed medication either prescription or over-the-counter. Even if it's an over-the-counter medication such as acetaminophen, if the doctor has prescribed it for that child, then it's considered a prescribed medication. If it is something that is to be given twice a day, then the parent can give it at home before the child comes to child care and then give it when the child is at home that evening. You may have one-time or short-term medications such as for a particular condition that's going on or there may be long-term medication for children with chronic or special health care needs. There are emergency medications such as an EpiPen Jr. or an asthma inhaler that you may be required to give to the child during the child's time with you.
Do not give these medications:
- New medications being given for the first time to a child
- OTC cough and cold medications
- Folk or homemade remedies or treatment
- First aid cream, hydrogen peroxide, etc.
- Teething gel
- Expired medication
There are times that you will not give medications and it's just as important to know when not to give medication as it is to know when to give medication. If it is a brand new medication, one that is being given to the child for the first time, then the parents should have given that medication at home at least once before that child comes to child care. For example, if a child has a heart condition or some other special needs condition and the physician has prescribed a new medication for that, the child should receive the medicine at least one time before coming to your program. A child should not be brought into child care with a medication he or she has never had before. There's no way to know exactly how that child will react to the medication. It's very important that the child has been given the medication before and you know how the child will react to it.
Never give over-the-counter cough and cold medications. The American Academy of Pediatrics does not recommend cough medicines for children. It's better for them to be able to cough and cough up the mucus or whatever the cough is producing. You do not give cough and cold medications in child care. Do not give folk remedies or homemade remedies or treatments. It may be harmless for the child but if it is not something that is prescribed by the physician, you do not give it in child care.
You cannot have any medications in your first-aid kits. This includes first-aid creams, hydrogen peroxide, and rubbing alcohol. These are not allowed in your first-aid kits. Soap and water are the best way to clean cuts and scrapes.
Teething gel is not given because it may or may not help with the child's discomfort. There are too many dangers with it where if too much is given, it can actually cause numbness of the throat and interfere with breathing and swallowing. It is not something that is going to be prescribed.
Finally, if a parent brings in a medication, always check the expiration date. If it's expired, you cannot give it. Even if it's the last one the parent has, you cannot give expired medication.
Must have written parent permission:
- Sunscreen
- Insect repellent
- Non-medicated diaper creams
There are a few exceptions and it's very important to know these. There are three medications that you can give without a doctor or a healthcare provider's prescription, but they do require parent permission. The first one is sunscreen because we do want to protect our children from overexposure to the sun. Second is insect repellent and third is the non-medicated diaper creams. If a parent has those or your program may have the policy that you put on sunscreen before children go out, you must have written parent permission that you do not need a health care provider's prescription.
Who Can Administer Medications?
Any adult in your program who is administering medication should complete a standardized training course that includes skill and competency assessment. This course is designed as an overview. It's giving you the basics, but it is not sufficient for an adult who is administering medication, especially specialized medications such as injections. You should have one or more people who are designated in your program to give medications and they must be trained. The trainer should be a licensed health care professional. It may be a child care health consultant, the child's physician, a registered nurse, or a licensed practical nurse, but it should be a licensed health care professional.
The skill and competency should be monitored at least annually or if an error occurs. For example, if someone is giving medications to a child and something happens such as the child vomits after it and the person is not sure what to do, that would require that the medication administrator be retrained. Another example is if the wrong medication is given, then be sure that that person is retrained and their skill and competency are frequently checked.
If you have programs where several children require daily medication or even weekly medication, the best practice is to hire a licensed health care professional to give those medications. That's not always possible especially in family child care or small child care programs as you may not be able to have someone there on-site. It is admissible to have a trained teacher, administrator, or someone who is a responsible adult who can be trained to give medication.
However, all staff should be trained and that's the purpose of this webinar. Think about why people need to be trained? Teachers are the ones who greet parents and children every day. They can look for any kind of illness or side effects that might occur from medication. If you know that a particular medication sometimes causes a side effect, then you look for that when they come in. Also, as a teacher or caregiver, you may be the first one to ask, "Has the child had their medication today? What time was it given? Did everything go okay? How's the child feeling?"
Home visitors need to be trained because they may be discussing medication with families. For example, you never know what is going to come up just in conversation. I was walking out on the playground with a parent who mentioned that her child wasn't feeling well and she was giving her medication. Being the nosy person that I am sometimes, I said, "What's wrong and what are you giving her?" Then, for some reason, I said, "How much are you giving her?" It was a liquid medication and she said, "Well, I'm giving one tablespoon three times a day." I immediately knew there was a problem because a tablespoon is not a typical dosage. It turned out that the pharmacy had made a mistake on the label. The parent was doing what was written but it was not correct. In your conversations with parents, ask what's going on. If something strikes you that it might not be right, then go ahead and check further into it.
Vehicle drivers and attendants must administer first-aid, transport medication, and talk with parents. They might be dealing with emergency medications. Your food service staff may be avoiding ingredients that interact with medication. For example, some medications cannot be taken with dairy products. Also, a child may have an allergic reaction to food, so food service staff would need to know about emergency medications.
Six Rights of Medication Administration
The first handout that you have is the Six Rights of Medication Administration and we're going to go over that now.
- The Right Documentation
- The Right Child
- The Right Medication
- The Right Dosage
- The Right Time
- The Right Route
The Right Documentation
Accurate documentation is essential before, during, and after giving medication. Document everything!
- Written consent from parent/guardian
- Written prescription from doctor
- Administration of medication during day
- Disposal or return of medication to parent
It seems like everything we do requires a ton of paperwork but it is essential that you have correct documentation when giving medications. It must be accurate documentation and it's essential that you do that documentation before, during, and after giving medication. Document everything. If you're not sure if you need to document it, write it down. Use ink when you are documenting anything on medication. If you make a mistake and have to change something, draw a single line through it and then write the correct information. Do not document in pencil. It must be in ink. You need to have written consent from the parent or the guardian, a written prescription from the doctor, documentation of the administration of medication during the day, and documentation of disposal or return of medication to the parent.
Health Professional's Authorization
- Child’s name
- Health professional’s name & signature
- Date of authorization
- Name of medication
- Expiration date of medication
- Why medication is needed and for how long
- Time, date, dosage, and how medication is given
- Possible side effects or adverse reactions
- Special instructions
- How long consent form is valid (up to one year)
The health professional's authorization is the doctor's prescription. This is not the prescription that's given to the pharmacist, this is a prescription for you in the child care or early childhood or Head Start program. It could be a form that you have for your own program or the physician may have their own form. It should have this information though: the child's name, the health professionals name, and signature, their date of authorization, name of the medication, and expiration date of medication. By that, we mean how long do you give it. The form should also include why the medication is needed and for how long and at what point will that medication definitely be stopped. Be sure it includes the time, date, dosage, and how the medication is given, possible side effects or adverse reactions, and special instructions. The special instructions might include injections a child is getting or it could be special instructions such as give this with food or without food. The final piece of information that should be included on the form is how long the consent form is valid. If it's up to one year, you cannot have a consent form and then keep giving that medication for more than 12 months.
Parent/Guardian Written Consent
- Child’s name
- Parent/guardian’s name & signature
- Date of authorization
- Name of medication
- Time, date, dosage, and how medication is given
- Possible side effects or adverse reactions
- Special instructions
- How long consent form is valid
You need the parent or guardian's written consent. Just like the health professional's authorization, the parent/guardian's written consent should include the child's name, the parent/ guardian's name and signature, the date of authorization, the name of the medication, the time, date, dosage, and side-effects, instructions for the medication, and how long the consent form is valid. I know this is a repeat of information but these are two separate forms and you must have both.
Accepting Medication from Parents
- Verify the consent form on file.
- Complete daily authorization form.
- Check name of medicine. Must be in original labeled container. Verify expiration date.
- Verify special storage requirements.
- Verify any precautions for child (e.g., not go in direct sunlight; avoid dairy products).
Let's talk about accepting medication from parents. Let's say the parent comes in and says their child has a cold. It's minor and is not affecting the child, the child feels well enough to participate in all the activities and it's not contagious, so there is no reason to exclude the child. However, the child is on medication for some reason.
The first thing you should do is verify that the consent form is on file and that you have the authorization from the child's health care professional and the consent form from the parents. The parent signs this form saying they're bringing it in and you've got this medicine that was brought in today. Check the name of the medicine. It must be in the original labeled container. If they're bringing in a bottle, it must have the child's name on it, the dosage, and the expiration date on it. Verify any special storage requirements such as if it is a liquid that requires refrigeration or insulin that requires refrigeration. Verify any precautions for the child. For example, when taking some antibiotics the child cannot go into direct sunlight or must avoid dairy products.
Medications Must Be Properly Labeled and In Original Container
- Child’s name
- Name of medication
- Dosage
- Directions for giving medication
- Expiration date of medication
- List of warnings and possible side effects
Medications must always be properly labeled and in the original container. It is not acceptable for a parent to bring it to you in a seven-day pillbox or the things that we sometimes use as adults at home. They must be in the original labeled container with the child's name, name of the medication, dosage, directions, expiration date of the medication, and list of warnings. If it is a prescription medication, sometimes you have to look on the label to find the expiration date. Later, we'll go over where to find expiration dates on other medications.
Authorization Form
- Check for correct name and spelling.
- Print correct time; use AM/PM.
- Get parent signature.
- Get emergency contact number.
- Complete documentation in ink. If change required, draw single line through and initial.
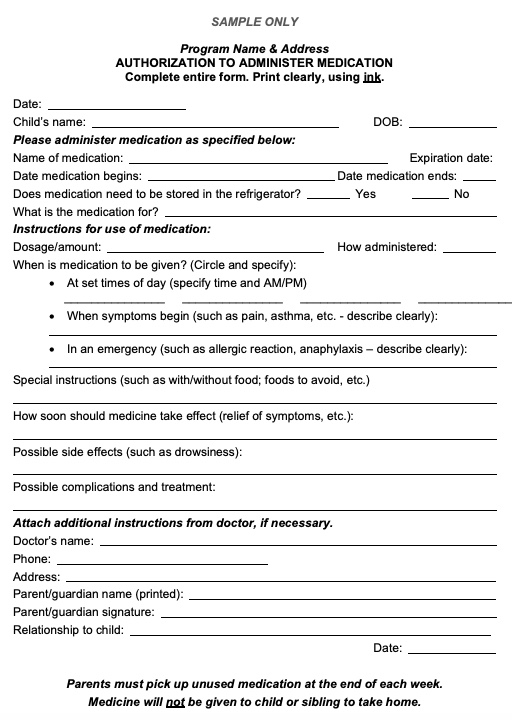
Figure 1. Sample Authorization Form.
Figure 1 is a sample authorization form that is one of your handouts. While this is a sample only, you can download some from different resources online or your program may already have an authorization form they use. You do need an authorization form that's a standard form for your program. That way everybody knows what to look for on the form and where to look for it. Always check for the correct name and spelling and get the signature. When you're writing the correct time be sure and write AM or PM. If they say the medication is supposed to be given at 11 o'clock, it should be written as 11:00 AM, while the child is in your care. Always get an emergency contact number. Remember that sometimes contact numbers change frequently so make sure to get one each time. Again complete the documentation in ink.
Daily Medication Form
- Date
- Child’s name
- Name of medication
- Time given
- Dosage
- Any observed side effects, reactions, comments
- Name and signature of who gave the medication
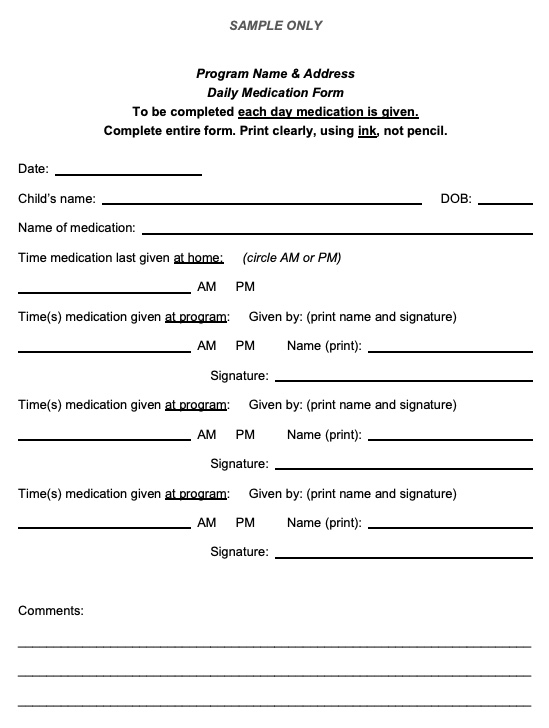
Figure 2. Sample Daily Medication Form.
Figure 2 shows a sample daily medication form. This one includes the date, the child's name, the name of the medication, the time that you gave the medication, and the dosage that was given. This form is filled out every day when you give the child their medicine. It should be filled out when the parent brings the medicine in and then any time it's given. The person who gave the medication has to sign this form. It should always be the person that has been trained to give the medication.
Administering Medication
Now let's get into administering the medication and the actual how to's. The first thing you should do is the same thing that we hear all the time in early childhood, wash your hands. You should wash your hands before giving medication and you should wear gloves when handling the medication. Some programs may not require this but it is recommended. You should wash your hands after giving medication. This would be especially true if you were using a topical medication, such as a cream that is applied to the skin. You wear the gloves as you're giving the medication because it keeps it off of your skin. Always wash your hands after so you're not then getting that on another child. Let's get into the other rights.
The Right Child
- Give medication to only one child at a time.
- Recognize the child. Ask the child their name.
- Watch out for twins or children with same name!
- Check the name on the authorization form.
- Check the name on the bottle – twice!
The next one is the right child. It's important to think about whether you really know the children in your care and if you recognize them when you see them. If you have a lot of staff turnover then that can be a problem. Most of our caregivers and teachers know the children and can pick out even the difference between twins. Remember that children do change how they look, especially young children as they're growing. Be sure that you recognize the child. Some programs, such as public school preschool programs and Head Start programs in a public school, have a particular person in the facility who gives medication. If that's the case, then that teacher who knows the child by name and by face goes with the child to the nurse to be sure that the wrong child isn't there to receive the medicine.
The first thing to remember is to give medicine to only one child at a time. If you have three children that are on the same medication, only have one child come up at a time. You should make sure you recognize the child and ask their name if they are old enough to speak and know their name. Watch out for children with the same name. Sometimes you have two Johnnys or two Marys or two Claudias. Check the name on the daily authorization form you received when the medicine came in and check the name on the bottle twice. Always check the name on the bottle twice, especially if you have two children with the same first name or the same last name. Check that bottle carefully.
The Right Medicine
- Get out one medication at a time.
- Check the child’s name on the medication container – twice!
- Check the name of the medication against the authorization form.
- Do not leave medication unattended.
- Store medication properly.
Make sure that you're giving the right medication. You have one child at a time and now you're going to get out one medication at a time. A child may be on two, three, or even four different medications during a day. Sometimes you may give two at a time. It may be that you give medication A in the morning and medication B in the afternoon. Only get out one medication at a time and make sure what you're giving is the correct one. Again, check the child's name on the medication container twice, check the name of the medication against the authorization form, and never leave the medication unattended. Don't open the bottle and then turn around to go wash your hands. Wash your hands before you get the medication. Once you open the container get out the proper amount of medication but never leave it unattended. As soon as you're finished, close the container with the child-resistant cap and store it properly.
The Right Dosage
- Use a calibrated medicine spoon, dropper, dose cup, or syringe to measure liquid medication.
- Shake liquid medication (suspension) 15 seconds before measuring.
- Do not cut or crush tablets, empty capsules into food, or add to bottle unless prescribed by doctor.
- Be sure the child takes all the medication.
- Be sure all the medicine comes out of the spoon or dropper.
- 5 ML = 1 teaspoon
- 1 ML = less than ¼ teaspoon
With any dosage, you need to use a calibrated medicine spoon, a dropper, a dose cup, or a medication syringe. There are different sizes of syringes, so you have to look at the calibration on them to see how much is supposed to be given. There are also medication dose cups that you can use that have the measurements on the side. Never use a spoon.
I have a fun activity on how to help train people, including parents, on how to give the right dosage. I start by gathering several different spoons, usually from my kitchen. I'll get what we think of as a tea spoon, a soup spoon, what I call a tablespoon or a serving spoon, and a plastic spoon.
For the activity, set out several different spoons and a bottle of water with food coloring added so you can see it. Ask the people you're training, whether it's parents or teachers, to pick up a spoon and measure a teaspoon of liquid. Once they've measured into the spoon, then pour it into a dose cup and see if it really is a teaspoon. I've done this at a lot of trainings and it's always interesting to see how much they measure. Depending on the spoon they pick up, it can range from half a teaspoon to as much as three teaspoons in that dose cup and they think they've measured a teaspoon.
A suspension is a liquid medication that's thick and not clear. If you have a suspension medication then it must be shaken for at least 15 seconds. Just count, sing a song, or do whatever you need to do make sure you shake it for 15 seconds before you measure it into the medicine cup or the calibrated spoon that you're using.
Do not cut or crush tablets and do not empty capsules into food. Do not ever put medication into an infant's bottle unless it has been prescribed by the doctor or the health care professional. I don't care what the parent tells you to do, if the doctor or the health care professional did not say it, you do not do that. Some medications will be affected by the food and some medications are not supposed to be taken with food. In addition, you have no way of knowing how much the child is getting once it's mixed with food. That goes back to those special instructions on your first authorization form.
Be sure the child takes all the medication. It may take a while if they don't like it or they're busy looking around but try to make sure they take all of the medication. Be sure all the medicine comes out of the spoon or the dropper.
Now let's look at some dosages. The prescription may say five milliliters (5 ML) which is equivalent to a teaspoon. The medicine dropper or cup will have the measurements on it. If the prescription says one milliliter (1 ML) that is less than a quarter teaspoon. It's a very small amount, so you probably be using a little syringe. Often when a parent picks up the medication from the pharmacist, liquid medications will have a dose syringe, dose spoon, or something with them. If not they should ask the pharmacist for one.
I went to my local pharmacist and asked if he could give me some dose cups and things that I could use for this webinar. He gave me five or six different syringes, dose cups and all kinds of things. They get these from the pharmaceutical reps and from the companies, so they do have those and feel free to ask for that. You can use them for training purposes and to have extras on hand to give medication.
Watch for and question any unusual dosages such as the one tablespoon. Another thing to remember is after you use that dose spoon or that medicine dropper, wash it, rinse it out with water, squirt a little dishwashing detergent in it and wash it out. Make sure to rinse it thoroughly, let it dry, then store it properly.
The Right Time
- Write specific time(s) on the daily administration form. Include AM or PM.
- Check the time written against the clock. Make sure your clock is correct!
- Check the time of the last dose given. Calculate the hours between dosages.
- Schedule before/after meals if instructed.
- ASK if the time between dosages is critical. Up to 30 minutes before/after may be necessary when scheduling around food service or other activities.
Right now I'm looking at a digital clock and it says 9:10. If I were to look at one of my battery-operated clocks if I haven't changed the battery it might not say the right time. Always make sure that your clock or watch is correct. I really prefer an atomic clock that has the correct time. Be sure you're looking at the correct time zone, whether it's Eastern Time, Central Time, or Pacific Time. That normally wouldn't be a problem but I do know of one city in Alabama where the city, Phoenix city is on Central Time Zone but many of their people work in Georgia which is Eastern Time Zone. In their school systems, the elementary school is in the Central Time Zone and the high school is in the Eastern Time Zone. It is possible to have two time zones in one area. Be sure that you have the correct time.
You have written the specific time on the administration form and it should have included AM and PM. Check the time the last dose was given. The first time you give a dose you check it against when the parent says that it was given at home. If you're giving an afternoon dose, check to see if there was a morning dose given and at what time it was given. If it's supposed to be given every four hours, you'll need to calculate the hours between dosages. Also, look at the schedule and special instructions. Should this medication be given before or after meals? It does make a difference with some medications.
Some medications can only be given without food and with no other medications because it makes a difference in how the body absorbs it. When the parent brings in the medication, ask if the time between dosages is critical. Feel free to call the pharmacist if the parent is not sure. Usually up to 30 minutes before or after may be necessary as we're dealing with the daily schedule for children. If that time between dosages is critical then you must follow that.
If the instructions say to give one-half a teaspoon three times a day when would you give that medication? With 24 hours in a day, three times a day sounds like it's every eight hours. Again is the time between dosages critical? If it's not then I'm not going to wake a sleeping baby to give medicine. When babies or toddlers are sleeping, let them. If it is critical that it's every eight hours, then ask what time is the parent giving it at home. What time do you give it during the program day and what time do they give it at night?
If you have a medication that says to give one teaspoon twice daily, then it's only given two times a day. The parent can give it before the child comes to the program and they can give it to the child when they get home. You should not be giving this medication in the child care program. The parent is responsible for that. That's one of the things that you should put in your policy.
Some medication instructions say to give five milliliters every six hours. Thinking about when to give that during child care, is that a critical time period or not? Is it specifically every six hours? There certainly is a difference in time if they gave it at home and then you're giving it at lunch, then they give it at supper and before going to bed. With that, there could be four hours in between or eight hours in between. Find out how critical the timing is.
The Right Route
- Oral medication:
- Tablets or capsules
- Liquids – clear syrups and elixirs
- Liquids – suspensions (shake before measuring)
- Sub-lingual drops (under tongue)
The next right for giving medication is the right route. This means how the medication is entering the child's body. If it's an oral medication it could be tablets, capsules, or a liquid. Liquids can be clear syrups and elixirs, which are the ones that are obviously clear, or suspensions. A liquid suspension is one that you must shake for 15 seconds before you measure it. Another one is sublingual drops which means it's under the tongue. If you see the word sublingual that means it's simply under the tongue, not on top of the tongue. If the medication is sub-lingual drops you have to have the child hold the tongue up while you put the drops under it.
- Topical medication:
- Eye drops and ointments
- Ear drops
- Skin ointments and creams
- Sunscreen
- Insect repellent
Other routes would be topical medications. Topical means that it's put onto the body in some way. It could be an eye drop or an eye ointment going into the eye. This is one that is more specialized, so you need to be trained on how to do that properly. Ear drops could be another topical medication or most common would be skin ointments and creams. Even those may have specific dosages that you are putting on. Sunscreen and insect repellent would be topical medications. Again, your sunscreen and insect repellent do not require a physician or a healthcare provider's authorization, but they do require parent or guardian permission.
- Inhaled medication:
- Nasal sprays
- Metered-dose inhaler
- Nebulizer
Inhaled medications include nasal sprays, metered-dose inhalers, and nebulizers. A lot of children with asthma and breathing difficulties may have these. If a child has a sinus infection or something similar, a doctor might prescribe a nasal spray. Most likely the nasal spray is going to be given once or twice a day and would not be given by the child care provider. However, if you have a child with asthma and that child has an asthma inhaler, then you need to be trained on how to administer it, perhaps as an emergency medication.
- Specialized medication:
- Suppositories
- Injections
There are also specialized medications such as suppositories, which are medications that are inserted into the anus (rectum). Another specialized medication you might see is injections. This would likely be if the child has a port and the medication is inserted into the port. It also might be an insulin injection for a child who has diabetes.
Unintentional Errors
- Forget to give a dose
- Give medication to the wrong child
- Give the wrong medication
- Give the wrong dosage
- Give medication at the wrong time
- Give medication by the wrong route
- Forget to document administration of medication
We've gone through the six rights, the documentation, the right child, the right time, right medication, right dosage, and right route. Now we're going to look at why you really have to be so careful when you are administering medication. Things can happen and there are unintentional errors that we want to prevent. All of your documentation, including those six routes, will make a difference in whether you do this correctly and avoid errors.
A very common unintentional error would be if you forget to give a dose. I set my alarm on my cell phone for everything because I will forget something. You get busy doing something else and you simply forget that you're supposed to do something. It's perfectly okay to set a reminder to yourself to say, I'm supposed to give medication to this child or these two children at this time.
Another unintentional error is you might give medication to the wrong child. You could give the wrong medication to a child or it could be someone else's medication given to the wrong child. It could be that the morning medication was accidentally given in the afternoon. That's why we only get out medications one at a time.
You could give the wrong dosage, either too much or too little or give it at the wrong time. You could give medication by the wrong route. There have been cases where it was sublingual, which is under the tongue, and the person mistook it for an eye drop or an ear drop. You don't want to give it by the wrong route.
You may forget to document the administration of the medication. In that case, think about what could happen. If you forgot to document that you gave the morning medicine and then perhaps another staff member came in and looked at the authorization form and saw that the child wasn't given the medication so that person gave the child the medication again. In that case, you have given the wrong dosage because you have given the medication twice. This is one example of why it's so important to document the administration of medication.
- Unintentional Errors: What to Do
- Immediately contact Poison Center at 1-800-222-1222 or a physician.
- Follow recommended treatment.
- Document exactly what happened.
- Inform the parent.
- www.poison.org
If these or any other errors occur, it's very important that you immediately contact the poison center at 1-800-222-1222 or contact a physician. That is the National Poison Center and that number automatically puts you in contact with the poison center in your geographic area. You might also contact a pharmacist. Physicians know a lot about medications, different chemicals, and drugs. Pharmacists probably know even more about individual medications than a physician would.
Follow their recommended treatment. Immediately ask, "What do I do?" Ask somebody, "What do I do in this case? We've made a mistake, what do I do?" Follow their recommended treatment, whatever it is. If they say call 9-1-1, you do that. If they say don't worry about it, it's fine, then you follow their recommendation.
You must document exactly what happened on that daily authorization form and inform the parents. Do not wait until the parents come in that afternoon to pick up their child. Call the parents and let them know what happened. Tell them you have contacted the child's physician (or the Poison Center) and they said this is what we should do. Make sure they are informed of everything. Poison.org is the national poison center. That's an interesting resource to visit because there's a lot of information on medications there.
Additional Things to Consider
There are a few other things that can happen but are not errors. Sometimes a child simply won't take the medicine, either by keeping their mouth closed, refusing it, spitting it out or vomiting after taking the medication. In this case, they haven't had their medication properly. What do you do? Document what happened on the daily authorization form. You can contact a physician or pharmacist for instructions especially if they spit it out or they vomited afterward. Ask the pharmacist, "What do you think should happen with this?" Again, inform the parent. If the child simply is refusing the medication you can call the parent and say, "I'm sorry I've been trying for 15 minutes and your child simply will not open his mouth to take this." The parent may decide it's really important and may come to give their child the medication or they may have suggestions on ways that they give it at home. It could be that there's a little song they sing that the child loves and is accustomed to hearing when taking the medication. There are a lot of ways to work with children.
Side Effects
Every medication has some type of side effects. A side effect is an adverse or undesired reaction to a medication by one's body. That doesn't necessarily mean it's dangerous. For example, an antibiotic is designed to kill the bacteria that is causing the symptoms or the disease. A side effect of many antibiotics is nausea, stomach cramps, or diarrhea. It's not what you want but it's simply a side effect.
You need to be familiar with the possible side effects of each medication. Any suspected side effects are something to include on the authorization form. If you get medicine from a pharmacy, even over-the-counter ones, there's always a piece of paper in the box or with it that tells you all the possible side effects. When you read all of those, it makes you think, do I really want to take this? They are required by law to document and to inform you of everything. It doesn't mean you will have those side effects, it just means they're possible.
If you notice the child does have a side effect then document it and inform the parents. Immediately report any unusual or unexpected reactions, including behavior changes. Sometimes the side effect of a medicine is that it's causing pain, a cough, diarrhea, or drowsiness. However, if there's something that's not expected such as a child suddenly seems to be lethargic, you need to call the parent and a healthcare professional. If a child is lethargic, meaning they're simply going limp, call 9-1-1 and get emergency care. It is possible for those things to happen. Usually, if there is an unexpected behavior change and definitely the lethargy or anything like that, that's more than a side effect which we will talk about.
Remember that every child can react differently to the same drug. If you have two children that are both on the same medication, for example, augmentin which is an antibiotic, then one child may have diarrhea and the other may not. Antihistamines cause drowsiness for a lot of children but some children actually seem to rev up and have a lot of extra energy when they're on an antihistamine.
Allergic Reactions
An allergic reaction is much more serious than a side effect. They're not common but they can be very serious. Before accepting any medication from the parent, ask if the child has had a reaction to a medication in the past, either that medication or any medication. If they say that the child has had a reaction to it, then you should not be giving that medication in the program because the next reaction could be more severe. For example, penicillin was given as the most common medication for years and it's still given but there are times that children or adults can develop an allergic reaction to the penicillin. A person may have had 99 injections of penicillin and never had a reaction, but on that hundredth one, they have an allergic reaction. You don't know when an allergic reaction will hit.
I saw a case where a teenager was on a sulfa antibiotic. He'd had that medication before and never had a problem with it but he woke up that morning and was itching everywhere from the top of his head to the bottom of his feet. He had little welts appearing, swelling, bumpiness, and itching. He immediately went to the physician who prescribed it, who was also an allergist, and they watched him very carefully for the next hour, giving him Benadryl, Claritin, and some other antihistamines. He no longer can take any kind of medication that includes sulfa in it. You must be very careful about allergic reactions.
Anaphylaxis
- Breathing problems
- Swelling of the face, lips, tongue, or throat
- Difficulty swallowing or speaking
- Rash or hives on the body
- Itching, including in the mouth
- Dizziness, confusion, fainting
- Abdominal pain, nausea, vomiting, or other sudden illness
With allergic reactions there's something called anaphylaxis. This is life-threatening. Anaphylaxis is an allergic reaction to a substance, whether it's food, medication, or something else. If you give a child a medication and they start to have any of these symptoms, call 9-1-1. If you see any breathing problems, no matter how slight they are, call 9-1-1. If you notice the child is not breathing as they normally do, that's a breathing problem.
Another symptom to call 9-1-1 for is any swelling of the face, the lips, the tongue, or the throat. Young children are not going to be able to tell you if they're swelling, but they might be reaching for their throat, you might notice breathing problems, or they might be moving their lips funny. You might notice that they are having a difficult time swallowing or speaking. Make sure to observe them and if you notice something that is not normal or typical for that child, then follow through and see what it could possibly be.
The allergic reaction might occur within 30 seconds, 30 minutes, or even two hours later of taking the medication. In the case of the teenager I told you about, it was six hours later when he woke up that symptoms were seen. There's no timeline on this. If it's an infant you might not notice the difficulty swallowing until you're giving them their bottle or with a toddler when they're eating their food. If you see anything like that, call 9-1-1.
Another symptom you might see is a rash or hives on the body. This may appear as redness on the skin, bumps on the skin, or feeling itchy. It could also cause itching in the mouth. Itching could be a side effect and might not be an allergic reaction but you are not the one to determine that. Any itching, especially if it's itching around and in the mouth, is considered an allergic reaction and you need to get a professional and their emergency help.
If they have dizziness or confusion or if they faint that could also be a symptom of anaphylaxis. Other symptoms include if they suddenly have abdominal pain, nausea, vomiting, or any other sudden illness. This also includes lethargy as I mentioned previously where they simply go limp. That is an allergic reaction. The abdominal pain, nausea, and vomiting may be a side effect of the medication which is why you need to know the side effects of the medication. However, if they are suddenly having severe abdominal pain or they're throwing up and having additional problems that are not typical and have never happened with this medication before, consider it an allergic reaction and call 911. Do not wait because it can become very serious very quickly.
Ask Questions!
It's important that you ask questions. You should be familiar with different types of medication that are commonly given to children and the typical dosages for children such as a teaspoon versus a tablespoon. Know the medications that are prescribed for children enrolled in your program who have special healthcare needs. If you have any questions, call a pharmacist. They're always glad to help and they're knowledgeable. If you don't have a regular pharmacist that you use or you don't know the pharmacist that the child's family uses, just go to your local drugstore and go to the consultation area. Let them know you have some questions about certain medications and most likely they'll help you. Learn more, because the more you know the better you'll be able to take care of children.
Storage of Medication
The storage of medication is very important. If you go to the Caring for Our Children Health and Safety Standards for out of home child care, they have information on medications including storage. It is very specific about how medication must be stored. It must always be in the original labeled container and it must be in a locked cabinet inaccessible to children. When I say a locked cabinet if it's in the classroom and it's in an area that is accessible to children, it must be in a locked cabinet. If the school nurse has a room where she works and gives medications, the door may be locked when she is not there.
If the medication requires refrigeration then you have to store it in a locked box that is away from food or in a separate refrigerator. A family childcare provider may have a refrigerator where all the children's food is stored. If parents bring in a medication that must be refrigerated, then get a locked box to store it inside the refrigerator. You can use a combination lock or one with a key. It does have to be a locked box, it cannot simply be latched.
Controlled substances must be accounted for. If parents bring in certain medications that are considered controlled, then count the pills when they come in. You need to know how many you start with and how many are given to the child. The number of pills must always be accounted for. If pills are suddenly missing then parents might say, "Hey, what happened to these pills?" You should know exactly how much of a substance has been brought in by the parent, exactly how much you give the child, and what you give back to the parents.
Again, remember to get out only one child's medication at a time and immediately return that medication to the locked cabinet after you've administered it.
Emergency Medication
There is an exception to this. Emergency medications such as an asthma inhaler or an EpiPen Jr. must be stored out of reach of children and in a clearly latched cabinet. You don't want them in a locked cabinet because you have to be able to access them immediately. If you're on a field trip, you might store those emergency medications in your fanny pack or backpack that is in your possession at all times but is easily accessible. It must always be accessible to the supervising teacher or the person who is trained to administer the medication. In this case, you may have teachers who are trained to administer emergency medication even though those teachers may not give other medications. The emergency medication must be available at all times including outdoor play, mealtime, and transportation. For example, some children are severely allergic to fire ants or bee stings so if you're out on the playground you have to have that emergency medication with you.
Check Expiration Dates
- Outdated medications can change chemical structure. Some become ineffective; others become stronger or toxic!
- Most prescription medications should be disposed of after one year. Read the label.
- Liquids, such as antibiotics, have a shelf life of about 14 days.
- Expiration dates are found on package labels. Make sure date is on the container, as well as on the original box when purchased.
- Tubes have the expiration date stamped on the crimp at the bottom of the tube.
Check the expiration dates. Sometimes those are tricky to find. If you have a tube look at the very end of the tube and the expiration date should be stamped into the crimp. Sometimes it's pretty easy to read the labels and it lists the expiration date. The label will have the date that the prescription was filled, the date that the prescription is no longer valid, and the expiration date. I've noticed my own pharmacy has changed their labeling about every six months or more frequently and the bottle and the label look different. I don't know why they do that because it's very confusing. On some labels, the expiration date is at the top and it's very clearly written. On others, it was down at the bottom and I had to search to find the expiration date of that medication. Find out what it is and make sure you include the expiration date on your authorization form.
Outdated medications can change chemical structure. Sometimes they become ineffective and sometimes they actually become stronger or toxic. Do not use expired medications. Most of your prescription medications should be disposed of after one year. Liquid suspensions, such as antibiotics, usually have a shelf life of about 14 days. If you're giving it as prescribed you should have given all of it anyway. Expiration dates are found on packaged labels. I've often found that the expiration date on over-the-counter drugs is on the box but it's not on the actual container. For example, if you get eye drops that come in a box, the date is on the box, so if you throw that box away you don't know what the expiration date is on the eye drops. Make sure before you throw a box away that you do have the expiration date.
Return Medication to Parents
- Return medications at the end of each day, end of the week, or when medication is no longer being administered.
- Give accurate account of controlled substances being administered and amount returned to family.
- Keep medications securely stored in locked cabinet until returned to the parent.
You should return medications to parents at the end of each day or the end of the week whenever it's no longer being administered. Remember to give an accurate account of any controlled substances and keep them securely locked in the cabinet until you give them back to the parent.
Disposal of Medication
- Follow disposal instructions on medication container, if listed.
- Participate in community drug take-back programs.
- Ask a local pharmacist about proper disposal methods.
- Properly dispose of sharps and other equipment.
You can go online and find out exactly how to dispose of medication. The container may have disposal instructions, there are community drug take-back programs, or you can ask a local pharmacist about it. If you are using injections or any other equipment, always properly dispose of sharps and other equipment. This is important for home visitors to tell parents how to dispose of expired medications. Don't throw it in a trash can because people go through trash looking for medications, and of course, children may go through trash. Also, pets get into garbage cans and you don't want anyone or anything to get the medication.
- Pour medication into sealable plastic bag. Add water to dissolve pills and capsules.
- Add kitty litter, sawdust, coffee grounds, soil, or other non-food material. Mix with the medication.
- Seal the bag and put it in the trash.
- Remove and destroy all identifying personal information from medication containers before recycling or throwing away.
- Document all medication disposed.
As I mentioned, you can find various ways to dispose of medication online. One way to dispose of medication is to pour the medication into a sealable plastic bag and add water if you're dissolving pills or capsules. Then add something like kitty litter, sawdust, coffee grounds, dirt or anything that's non-food and mix it with the medication. This is making it where nothing is going to want to eat it. Seal the bag and put it in the trash. You should always remove and destroy all identifying personal information from containers before you recycle or throw them away.
If you are disposing of the medication, then document exactly how you did this. You should only dispose of the medication if you are not returning the medication to the parents. It's recommended to return it to the parents, but if you are disposing of medication or if you're working with families on how they can dispose of medication that they have, this is how you can do that.
Questions and Answers
You talked about using your cell phone as a reminder, but I know that a lot of programs have no cell phone policies in the classrooms. Do you have a recommendation if somebody works in a facility where they are not allowed to have their phones out or even where they can hear it that they could use as an alternative for a reminder for giving medication?
All programs have a daily schedule that's posted in the classroom and you might put a sticky note beside the time that a child needs to be given medication. Do not put the child's name on it, but you could put a code or Rx for medication. You could also put a sticky note right beside the clock on the wall to remind you that at this particular time a child needs medication.
References
Caring for Our Children: National Health and Safety Performance Standards; Guidelines for Early Care and Education Programs, 4th ed. Itasca, IL: American Academy of Pediatrics; 2019.
U.S. Department of Health and Human Services. (2016) Head Start Program Performance Standards. (45 CFS Chapter XIII) Subchapter D, Part 1302.47. Accessed at: https://eclkc.ohs.acf.hhs.gov/policy/45-cfr-chap-xiii/1302-47-safety-practices
Hendricks, C. (2016). Medical emergencies in early childhood and school-age settings. St. Paul, MN: Redleaf Press.
Citation
Hendricks, C. (2019). Administration of Medication in ECE Settings, in partnership with Region 9 Head Start Association. continued.com - Early Childhood Education, Article 23377. Retrieved from www.continued.com/early-childhood-education
