Learning Outcomes
After this course, participants will be able to:
- Explain effects of hearing loss on families and the support that parents need when a child has hearing loss.
- Explain key components of support groups for parents of children with hearing loss, and of support groups for children with hearing loss.
- Describe ways professionals can help children with hearing loss and their families to advocate for themselves about issues related to hearing loss.
Effects of Hearing Loss on Families
Jane Madell: When I started my career many years ago, newborn hearing screening was not in effect, as it is today. Hearing loss was not identified in children until their parents noticed that they were not developing speech and language. Parents already had a relationship with their baby when the diagnosis of a disability was made, but that's not the case anymore. Now with the advent of newborn hearing screening, babies are identified with hearing loss at birth, so families do not develop a bond with their baby before they get the information. They don't have time to recognize that something might be wrong. Ninety-five percent of children born with hearing loss are born to families with no family history of hearing loss, so parents are stunned when they get this information. They do not know anything about hearing loss. If they know anything about hearing loss, it is usually some like a grandparent has age-related hearing loss and wears a hearing aid that they dislike. They really do not know what to expect or how to proceed. Parents need help accepting that there is in fact a hearing loss. They need help understanding that hearing loss is a manageable disorder, that if we do what we need to do this child will have a positive outcome. We can only help them understand that if we absolutely believe that ourselves.
We also need to discuss what needs to be done in terms of medical evaluations. Additionally, technology is an important area to discuss with parents. We need to help them accept the fact that the child will need hearing aids or other amplification, and talk about the value of an auditory-based therapy program. We also need to tell parents what all the options are, and to be honest about those options. Parents need to know what kind of language a child will develop if they have one kind of therapy, if their parents choose one communication mode versus what happens if they choose a different one.
When Do Families Need Support?
I think every family of a child with a disability, and that includes hearing loss, needs support groups to help them feel that they are not alone in this situation. They need support groups in the beginning when the child is first diagnosed, as parents are so overwhelmed. A support group can help them meet other families who have recently been through it and are a little further ahead, so they can feel like they are not alone in this world. Parents may also need support groups when a child's technology is changed. If a child wears hearing aids and needs to move to cochlear implants, that can be traumatic and parents may need help. They need help when a child needs cochlear implant (CI) surgery. Parents may need support when the child is starting school or changing schools; those are times that are stressful for most families and especially for those with a child who has hearing loss. When there are major life events like Confirmation, or Bar or Bat Mitzvahs, families want to know if their child with hearing loss will be able to do those things. At those times families may need a little more support either from professionals or from other families.
How Do We Provide Support to Parents?
Most hearing loss is identified at birth, and there are significant advantages to that. Children can be fit with hearing aids a few weeks after birth and start therapy early, so that language delays can be minimized or eliminated. The child's listening age will be the same as their chronological age, or very close. When I started in this field, we didn't know the kids had hearing losses until they were between 18 months and two years of age, so their listening age was two years behind their chronological age. That makes a big difference in the way they develop language and it makes a big difference in the way that families feel about their children. The disadvantage of early identification of hearing loss is that the parent didn't know and love the child before getting the information that the child had hearing loss.
Support Groups
Scheduling parent and family support groups can be challenging. If children go to a center where a lot of children have therapy, then we can schedule parent support groups during therapy times. There are several families at once who are together at the same time and having therapy. If we schedule support groups in the evening, parents who work can be involved. In some cases afternoons may be better or weekends may be better. It may be a group that meets weekly, monthly, or occasionally at whatever intervals are best for the group so that families are able to attend and participate.
The advantages of a support group for parents of children with hearing loss or other disabilities is that it enables parents to communicate with others who have been through the same experience. The audiologist, physician, speech language pathologist, and auditory verbal therapist may know a lot about hearing loss but most of us have not been through the experience of having a child with a hearing loss. We know some things, but we don't know other things that a parent who is living it can know.
There are different ways to compose support groups. Topic-based groups are centered around a specific topic. For parents who are very busy, they're more likely to take time out to go to a meeting that is focused on a specific topic than one that is focused on themselves. They may want to learn about how to improve speech and language, how to get their child to do something, how to transition or pick a school, etc. When planning a group, you need to consider what is going on with the families and what kind of group would be most beneficial to them. There are groups for parents whose children were newly diagnosed, and groups specific for mothers or fathers. Even today, mothers and fathers often have different concerns about their children. Mothers may have more social concerns, and fathers may worry about what will happen to this child as an adult and will they need long term care (which is not usually the case). There are also grandparent groups. Grandparents have a particular interest in how children are doing and how they are developing. Support groups for grandparents help us talk to grandparents about their role. Sometimes grandparents can be a benefit and sometimes they can be a difficulty. I have had grandparents who told the parents that when they were babysitting for a child with hearing loss, the grandparents didn't want the child to wear their hearing aids. That is obviously a problem for speech and language development, as hearing aids should be worn during all waking hours. There are other grandparents who just assure parents that everything will be OK but do not make any effort to support the family's goals for that child. If they are people who are caring for children on a regular basis, that's something we need to work on. It is also important to have sibling groups. Siblings of children with disabilities really struggle. The child with the disability gets an enormous amount of attention from the parents, and sometimes other children feel overlooked. They may not really be overlooked, but siblings need a little support. And for the child with hearing loss, support from other siblings is sometimes very helpful.
Informational support groups may focus on technology, school, or dealing with other family members. And then there are support groups that deal with emotional issues. The groups for mothers or fathers, mixed groups, siblings groups, and grandparents groups can all deal with emotions.
Basic Information about Technology
It is critical to have basic information about hearing technology when working with families of children with hearing loss. Here are some important things to know:
- Hearing aids work well for children with mild to moderate hearing loss.
- Cochlear implants work well for children with severe and profound hearing loss. Before children are considered for a cochlear implant they will have had a trial period with hearing aids.
- Some children with moderately-severe hearing loss will do well with hearing aids, but others will need cochlear implants.
- All children with hearing loss will need a frequency modulation (FM) system in school and in other listening situations where there is background noise. An FM system is a wireless system that transmits sound directly from a sound source (such as a teacher's microphone) to a receiver (attached to the child's hearing aids or cochlear implant). As children get older they may not want to use an FM system, but if they do not they will have difficulty hearing people in school who are more than three feet away. More information on FM systems can be found here.
Supporting the Child with Hearing Loss
Figure 1 shows the child in the center of the figure, and all the people who are critical in supporting the child to be successful. These include the family and extended family, the educational audiologist, the clinical audiologist, the physicians, and the speech-language pathologist. Social workers, psychologists, and educators are critical people in this child's world. We need to be sure they are all communicating with each other if this child is going to succeed.
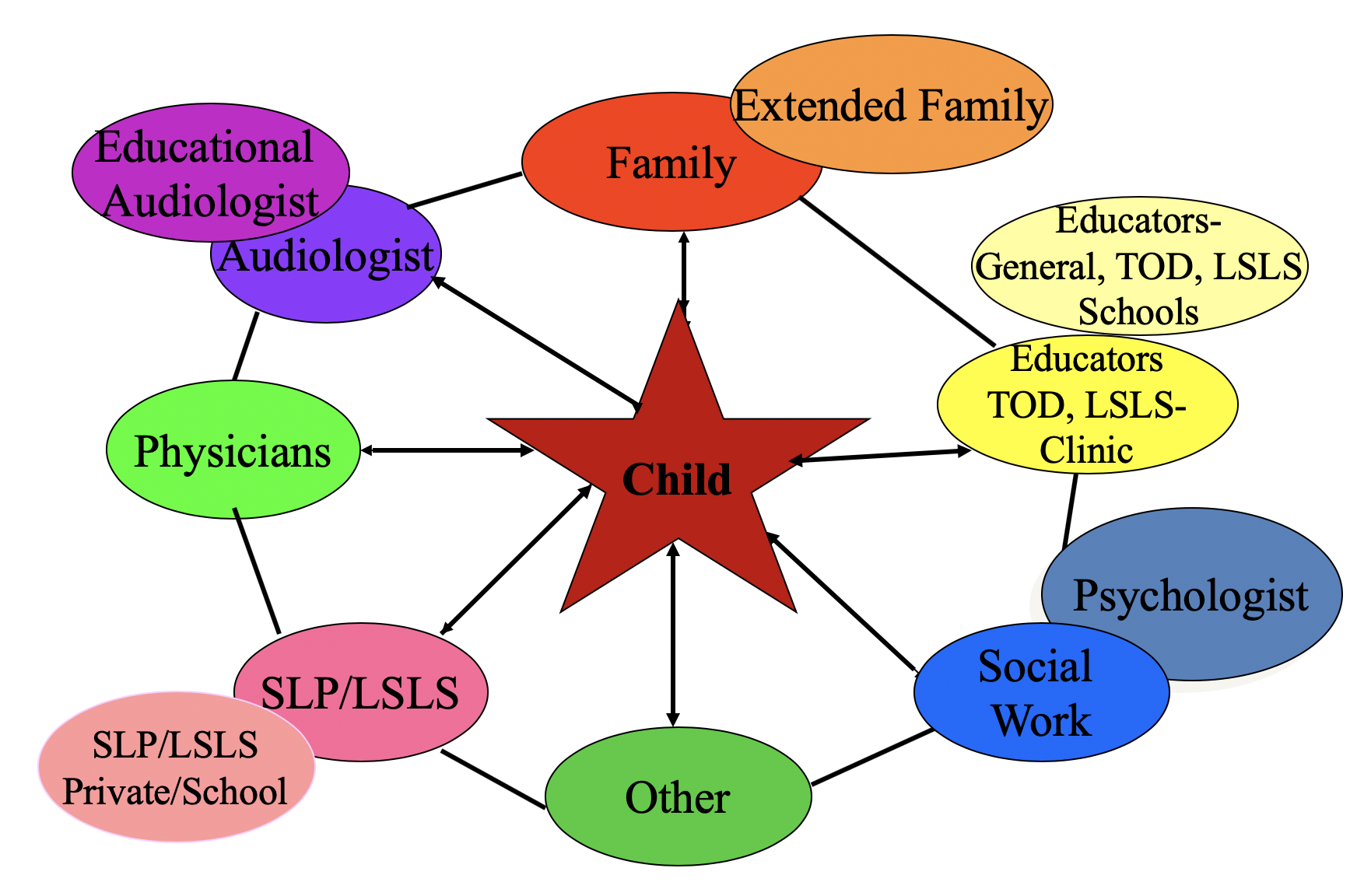
Figure 1. The support network for children with hearing loss, with the child at the center. Copyright 2019 Jane Madell, www.janemadell.com.
Roles of Different Practitioners
Here is a short summary of the roles of the different practitioners in the support network for children with hearing loss:
- Audiologists: Diagnosis of hearing loss, evaluation and management of technology, counsel parents and children about the effect of hearing loss, help school staff understand how to manage a child with hearing loss.
- Speech-Language-Auditory Pathologists/Listening and Spoken Language Therapists: Evaluate speech-language-auditory skills, develop treatment plan for building skills, provide therapy, monitor progress
- Physicians: Medical evaluation and treatment
- Educational Psychologists: Psycho-educational evaluations to identify learning issues
- Social Workers: Counseling and support for families and children
Client-Centered Counseling
Client-centered counseling puts the client in the middle of the procedure. Counseling that tells the family what we think we should do is not always in the family’s best interest. This does not always work well because it does not empower families to build their own skills to move forward.
Client-centered counseling in the diagnostic process begins when we first have contact with the family. If a hearing loss with the child is identified at birth, parents do not have a lot of information about the baby to share. But if a child is diagnosed later, then there is information that the parents can tell us about what they see at home and what a child is hearing. At this stage, it is important to let parents share their feelings about what they have seen and what they are observing about their child. They need to be allowed to tell their story to determine what they have seen and what they suspect.
Parents as Co-diagnosticians
It is important to involve parents in the diagnostic process. In audiology, we can sit the parent in the test booth with the child so they can see everything that is happening. That helps diminishes the denial mechanism of, "I'm sorry, I just don't believe he has a hearing loss" because they are in the room with the child. It also builds confidence between the parent and the clinician because the parent can see how the clinician is making a clinical judgment about whether the child has a hearing loss.
It is also important to include parents in speech and language evaluations that determine whether the child has a speech and language delay. Research shows that parental satisfaction with testing children who fail newborn hearing was a function of how empowered the parents felt in participating in the process. Parents have such a vital role because clinicians do not spend all that much time with children. What we do is important, but parents make the decisions about acting on our recommendations and how they are going to follow up.
In order to involve parents actively in audiology test procedures, we engage them as much as possible in seeing responses. When I am testing children in the sound booth, I involve the parents in watching the child’s responses. If we are doing an auditory brainstem response (ABR) testing, we can position the parents to see the equipment screen, so that they can see when there is a change in response.
When parents participate in the diagnosis, they are more likely to accept the diagnosis. They can see responses in behavioral testing, the ABR testing, and otoacoustic emissions testing (OAEs). We can let them observe what the child responds to with and without technology, and that helps them accept what the child is hearing. With corroborative testing in the sound booth, we can have one parent sit with the child and have them point out responses. If there are two parents, we can have the other parent sit with the audiologist and have them describe what they see and what they think. In speech-language evaluations, let the parent observe testing and comment on performance. Parents are often surprised when their children show language deficits because they do not see the child the same way we see them. The parent is working with the child alone, but they may not delving into difficult language situations, such as complex wording. When a speech-language pathologist does an evaluation and the child is making errors, it helps if the parent can see the errors because that helps them understand what they have to do at home.
Listening Bubble by Karen Anderson
It is important that families understand the Listening Bubble concept that Karen Anderson developed some years ago.
The Listening Bubble refers to the range of hearing within which speech can be fully heard. The Listening Bubble can be used to describe hearing loss in terms of how far away a child can be to fully understand someone speaking. A person with hearing loss has a smaller listening bubble than someone without hearing loss. For example, a child with normal hearing will hear you speaking at an average volume level from 10 or 15 feet away, but a child with a hearing loss may not hear or understand from that distance. When we describe to parents and families what a child can hear, it is very helpful to talk about a listening bubble. It explains why a child with hearing loss may hear loud sounds but not soft sounds, or may hear when you are close to them, but not when you are far away. The listening bubble gets even smaller when there is competing noise in the environment. When there is noise in the environment, it will be more difficult for a child with hearing loss to hear and understand.
Different voices can be easier for a child to detect. A father with a low-pitched voice may be easier to understand than a mother whose pitch may be higher as hearing loss is often greater for higher pitch sounds. In this case, we can explain that the child’s listening bubble is bigger when her father is speaking and smaller when her mother is speaking. The concept of the listening bubble is also very useful for children to help them understand their own hearing loss.
Another concept that is important when working with children with hearing loss is speech understanding. Speech perception testing is usually described in percentage, but not all people understand it. An audiologist may explain that a child has 88% word recognition ability, but what does this mean to parents? Some people have found it is easier to describe it in terms of pieces missing from a puzzle. Imagine looking at a jigsaw puzzle that is put together but has several pieces missing. For example, if you have a 100-piece puzzle and you are missing 12 pieces, you don’t see the entire picture. This analogy may be helpful for families in understanding speech perception testing scores.
The Counseling Role Following Diagnosis
Regarding counseling after diagnosis, all decisions made for a child are based on parent choice. They will decide whether the child will wear technology and what kind of communication mode a child will participate in. Therefore, we need to provide parents with information that will help them make educated decisions. We need to help parents become empowered because they need to feel that they can make a decision for their child and follow up on it.
I ask families about the goals for their child. Where do you want them to be when they are five, and 10, and 15, and 20? Almost every parent says that they want their child to be able to go to school and play with other kids. I ask them about what they think it will take to get them there because if they want their child to go to school, they need to be able to develop good listening and spoken language. We need to be honest when describing all the options because we have different expectations for children who are in an auditory program versus children who are in a signing program, and we need to talk to families about what those expectations are. We are not saying that one is better than the other, we are just being clear about what you will expect in terms of one program versus the other.
This question always comes up: how much should we answer for a family? This is common with cochlear implants and when parents are trying to decide about a communication mode. Parents may sometimes ask us, If this was your child, what would you do? This is a trap we need to avoid. For example, if I say if I were deciding for my own child, I could choose a cochlear implant, then parents want me to decide which cochlear implant. We cannot do that because that sends a message to the parent that they are not competent enough to make decisions for their child. We see successful outcomes by making sure that the family is making the decisions. Families do not learn to become responsible for their decisions if they do not make them for themselves.
Here are some questions that are useful counseling tools:
- I can see that you're having a hard time with this decision, can you tell me why this decision is difficult for you?
- Do you have questions I can answer to help you make this decision?
Let the parents talk through the answers to these questions. This can be difficult for them, but it is important to have the parent make the decision in their own good time. We also need to routinely and actively engage parents in dialogue about the goals for their child and what they have to do to carry over those goals. What do they have to do at home? We need effective dialogue to help them become knowledgeable about what it takes to succeed. What is the parent's role if they choose? For example, what is the parent's role if they choose sign language? We need to help them be familiar with normal speech, language, auditory, and cognitive development. It is essential that we listen to the parents. This is a stressful time for them and we need to arrange for parent support. Parent-to-parent support is effective because those who are a year or two ahead of a newly diagnosed family are in a different place. The initial panic is over and they have a child who they see is progressing, and can help newly identified families be optimistic. Validating parents’ feelings is also critical when working with families.
Support When Considering Cochlear Implants
When a child is not doing well enough with hearing aids, professionals may have to make the decision to move on to cochlear implants. Moving towards cochlear implants can be traumatic. That is difficult for families of newborns, too. If we know the baby has a profound hearing loss, we know we are going to have to move onto cochlear implants right away. But for a child with a moderately-severe hearing loss who starts out making progress but then progress slows, talking about cochlear implants can be very hard for families. It is always stressful for parents when they have to think about surgery for their baby. We need to help parents understand what kind of benefit the child will get if they choose an implant. You may need to explain that hearing aids are not working well enough and show them what we expect from children with cochlear implants.
Having parents meet children with cochlear implants is very helpful. Speech-language pathologists can demonstrate why the speech and language skills are not progressing at a sufficient rate and social work services can help families develop realistic expectations and provide emotional support. We cannot expect a child without speech and language to be speaking in three-word sentences two days after surgery.
Even when we have explained about realistic expectations with parents or older children, they may not believe us and think everything will be perfect from the beginning with cochlear implants. Sometimes that is a problem. Families and children need to understand that it takes time to build skills and that a CI alone doesn't provide magic benefits. Children still need auditory-based therapy and mapping of their cochlear implants on a regular basis.
Support for Children
Children with hearing loss are, for the most part, educated in mainstream school settings: 85% of children with hearing loss are educated in the mainstream. The advantages of mainstream education are that the kids have normal language models and the school has normal developmental, academic, and social expectations, so the kids have a better opportunity as adults because of their language skills. The disadvantage is that they are often the only child with a hearing loss in the school and have no contact with other children with hearing loss. That is a problem because they have difficulty hearing in school and may have questions about management of their hearing loss or technology. If their language skills are not at typical hearing levels, children with hearing loss will have limited social opportunities.
Support Groups for Children with Hearing Loss
Children who are a part of mainstream activities are in a situation where they have better academic and language models but feel isolated, and their friends often don’t understand the issues of hearing loss. If they go to someone's house and have a sleepover, they take off their technology to go to sleep and they cannot hear anything that is happening. As they get older, social issues become more significant. Children in special education classes may feel less isolated but have lower expectations. They may need assistance dealing with people outside of school because they don't have language skills that enable them to do that.
Counseling Children with Hearing Loss
Children need both informational counseling and support counseling. We do not always think that we need to provide the same kinds of counseling to children but we need to do that as soon as the children are ready. Social skills are dependent on language age. Children socialize well with other children as long as they have the language to communicate. They may do really well in preschool through first grade. By the middle of second grade, if their language skills are not equal to their peers, they are going to start having socialization problems because they cannot follow games being played or participate as much in discussions.
By the age of eight or nine, children begin to recognize that they are different. As children get older and are more aware of their hearing loss, they begin to resist things that can help, such as wearing an FM system or other hearing technology. Some resist going to therapy or decide they are not going to wear their technology. Children with disabilities are also more likely to experience bullying, and it is the responsibility of all of us who work with these children to check in and see if they are having these problems. When a child comes in and says they want to take off their FM system, the first thing I wonder about is whether they are being bullied. We need to think about ways we can help children deal with being bullied, so we counsel children as they are ready for it.
In terms of topics to cover in counseling, children need to understand the degree of hearing loss and it means. They need to understand hearing technology and why they have a hearing aid or a cochlear implant. We need to give them an opportunity to talk about their feelings towards having a hearing loss. It is not fair and I am sorry this is happening to you, but it is happening and we have to do some things to fix it. We need to help them talk about the social issues that are related to hearing loss. What kind of problems do you have and what can we do to fix it? We also need to help them build self-advocacy skills so they can ask for help. If they do not understand something one of their friends is saying, they need to be able to say, “I didn't hear that, can you say that again?” They also need to be able to say that to teachers at school. But we also need to give them permission to feel bad about the fact that they have a hearing loss and are in a situation they do not want to be in.
Counseling Older Children with Hearing Loss
When we test a child who is old enough to understand, we need to describe to them what they are hearing with and without technology. It is important to discuss how this affects everyday listening. If you have an audiogram that has all the phonemes on it, you can help them understand which phonemes they are missing without their technology. We also need to talk about the difficult listening situations they have and how technology can help.
We need to be careful about how much information we provide. We need to determine what the child wants to know and what they are ready for at that time. We say, “Tell me what you want to know about your hearing loss.”
These are questions that children may ask:
- When will I be old enough not to need hearing aids?
- Will my hearing loss go away?
- Will my hearing get worse?
- What will happen if I don’t wear hearing aids?
I once had a six-year-old boy want to know when he would be old enough to no longer need hearing aids. His mom and I looked at each other and realized that we had not made it clear that this was going to be a lifelong situation. We also need to talk with them about their language, as well as their future. I had a middle school student who said he did not want to wear hearing aids anymore and asked what would happen if he did this. I said to him, “Do you want to go to college?” He said yes. “Where do you want to go to college?” He said Harvard, Princeton and Yale, which are good goals. “Okay, let's think about what your grades will be if you're missing half of the phonemes.” So we need to just talk things out. If they ask a question, answer it. Offer the information on a regular basis so they know what we are trying to tell them. We need to talk about why they need speech-language therapy, as well as discuss skills and what they need. They need to know about what can be done to build skills and that hearing helps them learn a language.
Running Support Groups
With today's technology, most children are educated in the mainstream, but they may not be able to contact other children with hearing loss. It is important for them to have someone else who understands the situation that they are in and give them an opportunity to talk about how they feel. In those situations, there needs to be a moderator that can help them understand, either somebody to type it on a screen or write on a blackboard what the concerns are. Then we can go around in a circle and all make suggestions for how to handle those concerns. I had a situation where a child with a hearing loss was giving up their technology. I could not make a change, but the other kids in the group helped her understand what she was doing if she gave up using technology. They can provide support for each other.
When I run a group, I set it up by age and communication mode. I do not worry about the degree of hearing loss because with whatever technology they are wearing, they should be hearing well and able to communicate. To start the group I ask, "Tell me something funny about having a hearing loss.” It is often mentioned that a teacher forgot to turn off the FM microphone and the child heard things they were not supposed to hear. Then I suggest that they name five or 10 things that their family and friends know about them. It is very interesting how many of them will say in that list that they have a hearing loss, while others will say that is not something that matters. I ask, “Is there anything good about having a hearing loss?” Some of them say they get more attention from parents.
Most importantly, I ask about the problems with having a hearing loss. We list all the problems on the board, then have everyone make suggestions. We talk about social issues, including bullying and teasing. I bring those topics up myself if the children do not. Most kids do not want to leave at the end of the hour. It is something that they crave and we need to work on it for them.
Counseling Issues with Children
A typical issue is fear of parent anger. Children have been yelled at in the past for not hearing or for losing a hearing aid. Parents are concerned about how much hearing aids cost, so the children do not want to tell them if their hearing aid is not working well. There is also ridicule from siblings or other children. The refusal to wear hearing aids happens often, especially with those who have relatively mild hearing loss, and sometimes kids with profound hearing losses who are not doing well. With younger children, rejection of hearing aids is usually the result of parent attitudes, since they can see that their parents are upset about it. With older children, it is usually related to the attitudes of peers. We need to talk to parents about their concerns for the child having a hearing aid and provide them with support, but we also need to help them understand the effects of their child not wearing a hearing aid.
Helping Children Talk About Problems Listening
In order to help children talk about their problems we can ask questions, such as, “Do you only hear part of it when someone talks to you?” Encourage parents to share their concerns and behaviors they have observed under what conditions, and have the child there as well so they can hear that parents also recognize the situation. Mention that we all have problems hearing sometimes, even people with perfect hearing, but then discuss the situations where the child has a problem and see what we can do to fix it. Sometimes that helps families understand that it may be necessary to change technology.
With older children, if we test their speech perception using the loudspeaker in the soundbooth both with and without their hearing aids and/or cochlear implants, technology, we can demonstrate to them what they are missing. For example, we may find that at a normal conversational level they understand 86% of the words presented and at a soft conversational level, they understand 48%. We may also explain to parents or children that they will not hear unless the person speaking is standing no farther than three feet away, which means they will miss what is happening in a classroom. Audiologists should perform testing in noise as well. When hearing testing is only performed in quiet, scores are not representative of real world situations. Results of speech perception testing in noise can help to demonstrate how much the child is missing. Remind them that you understand this testing is difficult because we need to let parents and kids express their frustration and anger.
With teenagers, talk about the problem of the pieces missing from the puzzle. Talk about how they are getting new information in school and if they are only hearing part of it, they are not going to learn well. We also need to talk about the fact that hearing loss is fatiguing. Children with hearing loss have to listen much harder to fill in the blanks that they are missing due to hearing loss, so they are constantly doing extra work. But we also need to make children understand that other students will recognize that something is wrong if they decide not to wear their technology. The effects of hearing loss can be subtle but will be noticed by other students, and it would be better to deal with the hearing loss so that they can hear and communicate. We should also talk to teenagers about the lifelong impact of having a hearing loss. Adults who have hearing loss and wear hearing aids earn 50 percent more during their lifetime than those with hearing loss who do not wear hearing aids and instead try to get by without them. About 30 percent of people in prison have a hearing loss, which may lead to poor choices due to not hearing what was happening around them or not effectively navigating social situations and communication.
Self-Concept
We need to help children deal with self-concept. They may internalize the reactions of others, so when people look at them with annoyance due to their difficulty hearing, it makes the children feel bad. They are not ready to tune out the reactions of people who treat them badly. Children with hearing loss often have a relatively poor self-concept if they do not have the language to compete with their peers. Also, they may have fewer opportunities to interact with peers if their language is not as good. They have less opportunities to practice social rules and may misinterpret interactions. If they do not understand sarcasm or certain idioms, they will not be able to keep up in social situations. It is the job of everyone who is working with the children to make sure that they have the language they need. Hearing aids alone may cause a self-concept problem, since wearing the device may amplify the difference between the child and their peers. Children with hearing loss may have fewer options to socialize especially if their language skills are not at age level. We need to make sure that children with hearing loss have the vocabulary to express their emotions and help them learn to recognize emotions in others.
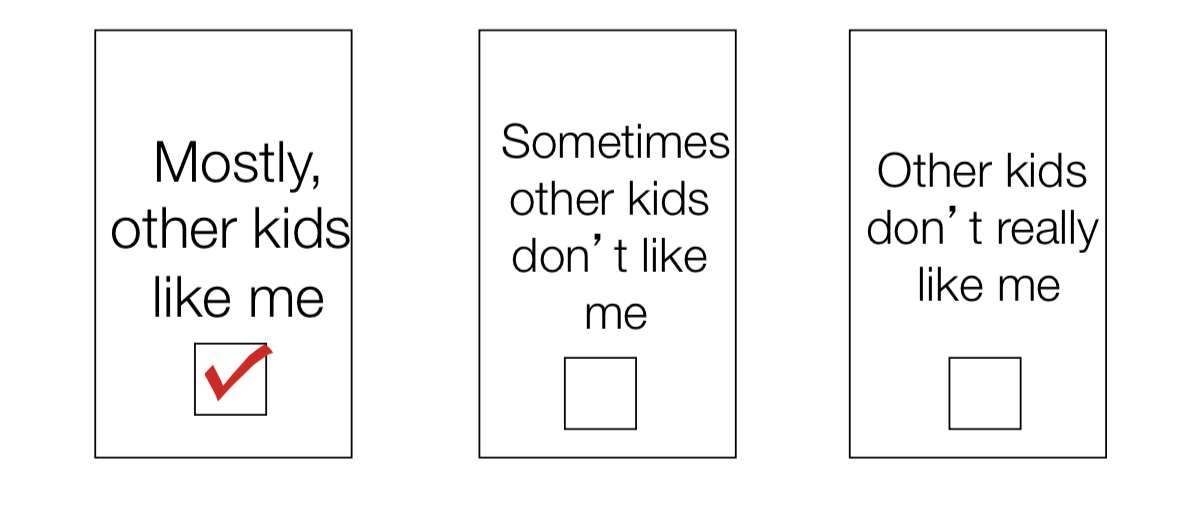
Figure 4. The Child Peer Relationship Scale.
Figure 4 is the child peer relationship scale. With this, there are eight discussion points we ask kids to fill out and then they can check the points. These statements can be about relationships with other kids or their feelings about school. If we get them to just check which best relates to them, we can get a better picture of where they are and what kind of assistance they need. It could be specific therapy assistance, technology assistance, a support group or counseling, and we can get that by looking at these responses.
We can use the Cappelli "I Start/You Finish" tool as a way of checking in with kids:
- I am happy when____
- I am sad when___
- The thing I like most in the world is____
- The thing I would change in the world is_____
- Because I have a hearing loss_____
Using this activity, we can get an understanding of where a child is and possibly refer them to a counselor to help them work through these issues.
There are some self-assessment tests for teenagers that are available on the Internet, including the Self-Assessment of Communication - Adolescents (SAC-A) and the Significant Other Assessment of Communication - Adolescents (SOAC-A). These also provide good information to help us figure out where a child is and what kind of help they need.
Using Scenarios
We can also do an exercise where we discuss different scenarios. For example, we can show children a picture of a student sitting at a desk and a teacher speaking at the front of the room. We can then ask, “Does your teacher do that? Is it hard to hear your teacher when your teacher is standing in the front of the room? How much of what the teacher is saying do you miss?” It is an opportunity to get kids to talk about these daily situations. Additionally, the Ida Institute has a game where you can set up situations and help children talk about their experiences relative to those situations.
When we are talking with children, we need to be sure that we are keeping the door open. We need to make sure that the children understand that we hear them and understand that they are struggling. We need to give them encouragement and show that we are listening. For example, if a child is struggling to describe a difficulty, we can say, “I think what you're saying is that you're having a hard time talking to kids in places like the lunch room where it's very noisy. Let's think about what we could do about that.” Acknowledge their feelings, then try to help them solve the problem. Any indication that you are struggling to understand the emotional content of what a child is saying makes it hard for them to go on and say more. It is difficult for people to change if they do not feel like they are understood, so we need to be sure we are making it very clear that we understand where a child is.
Counseling Missteps
My colleague and mentor David Luterman talks about counseling missteps. When we counsel families, we need to be sure that we do not give the impression that we have all the answers and they do not. This is a quote of how we do not want to come across:
“I have all this information and training. You do not. I will help you see it my way.”
It is possible to make this misstep without using these exact words. Presenting yourself this way is not the message we want to give to families. We may know more about some things, but they know more about the child. It is important to have counseling remind families that we are listening to them and that they are capable of coming up with the answers.
Case Example
In this example, a 10-year-old boy tells the school he left his hearing aids at home, and then tells his family he left the hearing aids at school.
What can we do to manage this? We have to think about why the child is doing this and what we can do to change the behavior. We cannot get upset with the boy that he is not wearing the hearing aids. We have to talk to him about what's going on and understand that he is most likely upset about the hearing aids if he is refusing to wear them. We can say, “Tell me about this. Is that what the problem is? Is it hard in school? Are kids teasing you? Does it make you feel bad that you have to wear hearing aids and other kids don't? Do the hearing aids help you? What do they help you hear?” We ask questions to allow the child to talk through the situation, as well as how they feel and how they want to move forward.
Summary
Here is a summary of key points I have discussed today:
● At all stages, it is essential that professionals empower parents and kids and help them process the emotions associated with hearing loss.
● Involve parents as co-diagnosticians for children of all ages.
● Simulations and descriptions using decibel levels and the “listening bubble” are more useful to help families understand hearing loss than labels and audiogram interpretation.
● Encourage parents to identify their goals for their child and present them with unbiased information about all options.
● Counseling is important for kids with hearing loss.
● Hearing testing in noise is critical for older children and teenagers.
● Provide fact-based information about the life-long impact of hearing loss with older children and teens.
● Give everyone the chance to express feelings.
● There are both positive and negative help-giver responses. Resist the urge to rescue!
Questions and Answers
Will a child with a cochlear implant have difficulty hearing in school without an FM system?
Yes, the child with a cochlear implant will still have difficulty hearing in school without an FM system. Every child with a hearing loss needs an FM system no matter what kind of technology they are using. When they get to be teenagers, they often reject them, but if we can help them understand how much better they hear with the technology, we are making a big difference.
At what age do children start to grieve?
It is about age eight or nine when they first start recognizing they are different that they start to grieve.
Do you recommend hearing loss simulators to help parents, family, and other people understand hearing loss?
I do not like the hearing loss simulators and only use them when I think parents are really resisting understanding the effects of hearing loss. The reason I feel this way is that I think it makes it sound so much worse than it is. If you listen to a simulator for a moderate hearing loss, parents may start to wonder whether there is any possibility that a child with a hearing loss can learn anything. However, if parents decide that the child will manage without hearing aids, then I will use a simulator to help families understand what it is like to have a hearing loss. But for the most part, I am not crazy about simulators because I do not like the effect they give. But if we can use a simulator, we also need to be able to show what it will sound like with the technology on.
How can social workers learn hearing loss basics and technology basics?
Social workers who work in programs for children with hearing loss should develop those skills by meeting with clinic staff, including audiologists and speech-language pathologists. I think it is easier than trying to read a basic audiology textbook.
You mentioned support groups for children with hearing loss in school, are there sometimes not enough kids in a school with hearing loss?
It is usually done by district. School support can be provided if there are several kids in one school, but that is usually not the case. School districts can arrange to have all the kids with hearing loss meet for lunch in one particular school, or have kids with hearing loss meet at the end of the day and have a support group that way. You can also get support groups outside of school. AG Bell, the Alexander Graham Bell Association for Deaf and Hard of Hearing, has a wonderful program in the summertime called Leadership Opportunities for Teens (LOFT). It is a group of teenagers that can meet other kids with hearing loss, and the people who run the group are young adults with hearing loss who have already been through the LOFT program. The kids who have been through it find that they get wonderful opportunities to share their thoughts with other people who have hearing loss.
What are some movie recommendations for kids with hearing loss?
I made a documentary called The Listening Project, with Emmy award-winning filmmaker Irene Taylor Brodsky. We interviewed 15 people whose hearing loss I had identified when they were babies and are now young adults. We talked about what it was like to grow up with a hearing loss. It is available in full on DVD, as well as a short version for schools. Schools have found it very helpful in giving kids in the school an understanding of what it is like for the kids with a hearing loss, as well as for teaching empathy. The kids with the hearing loss who have seen it said it allowed them to realize that there is somebody out there who feels what they feel. Thank you for participating in today's course.
References
References are included in the course handout.
Citation
Madell, J. (2020). Providing support to families of children with hearing loss. continued.com/social-work, Article 1. Available from www.continued.com/social-work
