Editor’s note: This text-based course is an edited transcript of the webinar, Preparing Complex Medical Patients for Successful Community Integration, presented by Diane Ulmer, OTR/L and Melissa Gulizia, BS, RRT.
Learning Outcomes
After this course, participants will be able to:
- Define the role of the RT within the interdisciplinary team in alleviating barriers to community integration.
- Describe 3 key aspects of emergency preparedness in order to sustain long-term community living.
- Describe 3 strategies that can be utilized for communication with multiple providers post-discharge.
Introduction
Melissa Gulizia: We live in Lincoln, Nebraska, and work in a rehab facility with two different campuses, one in Lincoln and one in Omaha. Our patients come from all 50 states. We have experience with discharging very complex medical patients, not only to urban areas but to very rural areas where the closest hospital might be 100 miles away. Today, We will discuss how the respiratory therapist is integral to making this transition successful.
We use the term complex needs to describe these patients who have a lot of complex needs. They are sicker, have numerous interventions, multiple providers, and multiple systems involved. Many of the patients that we see on a daily basis as respiratory therapists had an incident such as a fall at home, a car accident, or a routine surgical procedure and a snowball effect has taken hold where numerous other things occurred. They may be on dialysis or may have cancer. Many different types of patients can fall into the category of complex medical patients. With the pandemic, our COVID-19 patients with severe lung disease fall into that category as well.
In 2021, we have a lot more technology and different treatments that increase patients' survival rates, as compared to what was available in the past. Because we are keeping these patients alive longer, these patients are much sicker and have numerous providers such as nephrologists and pulmonologists. Many of their organs or other body systems may be compromised.
Case Study
We will use this case study as our example for today's presentation. We will discuss ways to make Marvin's home discharge successful so that he can remain in his home for quite some time.
Marvin had a family member pass away. He was out mowing the lawn in preparation for family to come for services and he had a cardiac event. He rolled over a retaining wall on the riding lawn mower and sustained a C2 spinal cord injury. He spent some time in the acute care hospital and then eventually came to our long-term acute care hospital. He was 68 years old at the time of this accident. He came to us ventilator-dependent and with the C2 spinal cord injury, knowing he was going to be ventilator-dependent for the rest of his life. He had been working at a lumber yard in a rural town in Iowa prior to the incident. Previously he was healthy and did not have a lot going on besides some home access things and family support that we had to take into account.
Teamwork
I think It is important for everybody to understand that teamwork makes the dream work. This list may not be the same team members as your team at your hospital, but there are numerous people involved in each patient's care. Some might have little involvement and some might have more involvement than others. This is a list of who is on our team where we work and that we feel is necessary in order to really get patients back into the community.
- Patient
- Family
- Respiratory therapy
- Vendors
- Community partners
- Occupational therapy/Physical therapy
- Speech therapy
- Recreational therapy
- Psychology
- Physicians and nurses
- Social work/Case management/pt financials
- Maintenance
Notice, we put the patient and family first because they are the center of what we are doing. It is important for them to be part of that team. Everybody brings different views, different aspects, and another pair of eyes. As a respiratory or physical therapist, if I see something of note, I will bring it back to the team and really focus on that patient. Sometimes you have to get creative because patients with complex medical needs have a lot going on and some of that might not change by the time they go home. We will talk a little bit about some of those barriers and how to overcome some of those barriers.
It is very important not to have silos in your team. You want a cohesive collaborative team. For example, if a patient has a physical therapist, occupational therapist, and respiratory therapist working with them, we want them to work as a team and not come in and just worry about therapy in their discipline. Again, family and caregivers are an important piece of this team because they are going to be all of these listed when It is time to get back into the home. They are going to be playing the respiratory therapist, the speech therapist, nurse, and social worker. It is important to have that well-rounded team to help the family and patient be successful towards discharge.
Barriers
Here are some of the more common barriers that we tend to run into because of these complex patients needing a variety of different things and services.
- Access to services
- Language barriers
- Accessibility of home and transportation
- Caregiver burden
- Financial limitations
- Caregiver availability
- Difficulty with social participation, adjustment
- Insurance barriers
If we are thinking about discharging a patient to rural Nebraska or rural Iowa and the closest hospital is 100 miles away, what does that look like? What support and what EMS services are around there? Think about where they live and what access to services they have. It is rare, but it has happened that patients have had to move closer to those services in order to get back into the community to be successful.
I am sure many of us have encountered language barriers. We see lots of different cultures here at Madonna and patients and caregivers speak a multitude of different languages. This can sometimes can make it hard to communicate. Make sure that you utilize an interpreter service. Even if we have a family member that is fluent in English, they may not be more fluent in healthcare terms. It is important to pull somebody in that is used to healthcare interpretation and can be an advocate for that patient. Language barriers can also be hard when patients are working with vendors to make sure that their needs are met once they discharge.
Accessibility of home and transportation can be other barriers. Not all places have accessible transportation yet and patients may not have the ability to buy a new vehicle or car versus having a truck. Accessibility issues have to be taken into account. The caregiver burden is something many of us are familiar with. Being respiratory therapists over the past year and a half or so, there has been a lot going on with the pandemic so we should have a good understanding of what caregiver burden means. Be aware of what it is like for the caregivers to take on taking their loved ones home and care for them. Provide them information about respite services and other services that might be helpful.
There are financial limitations along with caregiver availability. Home care nursing is really hard to find right now. How can we piece things together so we can still get these patients home? Our patients belong at home. Other barriers include difficulty with social participation and adjustment issues, especially after a long complex injury or illness. It is important for psychology or counseling to be part of that team to help with the reintegration back into the community. Of course, there are also insurance barriers regarding what they will pay for, what they will not, and when patients are mandated to leave versus how long can we keep them. Insurance can keep us on our toes.
What is our role as respiratory therapists in overcoming these barriers? Our goal is not just to discharge them to home or the next level of care, but we want our patients to be able to sustain that plan. We want them to have long-term success in the community. We want them to be active members of their churches and schools. We really need to think outside the box and be creative in how to make that happen. I do not think anybody wants to see patients go in and out of the acute care system. We want to be able to get them home and sustain that plan. We play a very important role in that as respiratory therapists.
Role of Respiratory Therapy (RT)
There are many roles of the RT. Sometimes we get stuck on going in and doing our breathing treatments and managing the ventilator. But when we start talking about reintegrating these patients back into their community, It is important that we start thinking about other topics too. Think back to Marvin from our case study. Marvin loved being out on his back patio and enjoying the weather and his yard. When we think about Marvin and getting him out there, we have to think about mobility and portability.
We had to ensure he had a portable ventilator and we worked with physical therapy to ensure that we had the pieces of equipment on the back of his wheelchair to accommodate the ventilator, including his respiratory supplies, suction machine, and Ambu bag. If he wanted to go down to the coffee shop, we need to think about that too, such as does he have enough batteries. It is important to think about the portability factor in reintegrating someone into the community. Think about transfers, including ventilator circuits in regards to transferring from the bed to the chair and then going from the chair to out and about. Make sure the vent circuits are all strapped up and tightened.
These complex medical patients will continue having doctor's appointments and events they want to go to such as a basketball game, football game, or a birthday party. We have to think about transportation for them. Remember, we are trying to integrate these patients back into their communities and we want them to be doing those things. Think about evacuations and how that will be managed for your patient. We need to look at evacuations closely and the education that we provide our patients. When evacuations start, It is got to be pretty quick. Figure out a process and provide education to the family on how to make that happen.
We want to ensure that they remain stable at home so they still might be on a ventilator or may need breathing treatments throughout the day. They may get pneumonia so it is important that we are providing education on how to identify those early declines, when to call the doctor, and what different lung expansion or secretion mobilization techniques they can do. They are going to be at home and are not going to have access to you as a respiratory therapist. Let them know what they can do at home to try to prevent them from going back to the hospital or from getting sick.
Another role of the RT is to think about patients as a whole person and not just the situation, especially when it comes to their tolerance for positioning in side-lying, sitting, and standing. Some patients may not tolerate laying on their left side or right side. Work with the therapy staff to ensure we've got good skin health. It is good for the lungs to be up and moving. Co-treat with other therapy staff and ensure that the patient remains stable and can get into a position they can tolerate in the wheelchair or the bed.
Transition Planning
Transition planning involves planning for the patient right before discharge and making sure there are ready to be discharged. We provide patients with what we call a transitional living experience. This can be done in the hospital room, but we are fortunate enough to have rooms like an apartment at our facility. After training has been completed with the patient and their family or caregivers, the patient is placed in a transitional living experience for them to better understand their role and what that looks like at home. We always say, It is not a pass or fail experience. It is an opportunity to see what barriers still exist. Maybe we did not think about the wheelchair needing to be on the left side of the bed versus the right. Maybe we did not think about the ventilator needing to be on one side or the other or where to set the suction machine and oxygen equipment.
It is helpful to provide the education and get everything together for them to have an opportunity to practice while they are still in the hospital. It allows other healthcare providers to peek in and check on them or be available for help. They are not going to have that at home. We really need to see how things are going to go and make sure that caregiver expectations are set. What does that look like? They are going to need to be with this person for 24 hours a day, or somebody is going to need to be there. You may need to backup train a couple of people.
Identify the DME providers, vendors, and who is providing suction catheters. Take into account environmental supports and transportation plans, whether they are temporary or permanent. How are you going to get to the doctor's office? Most of us have social workers or discharge planners helping with all of this, but the role of the RT is to help them to understand what it looks like to live with a ventilator, a trach, and/or oxygen. Social work can help support transportation and get things lined up from that perspective but our role is to help them see what it looks like from a respiratory perspective. It is important to pull in every support possible. It is really amazing to see who steps up when an injury or illness happens. That could be church friends, members of the church, or the neighbor. Think outside the box to ensure that this is going to be successful.
Follow-up with the healthcare team and specialists is very important. Patients need to get to their therapy if they are still doing outpatient therapy. They need to get to their doctors for follow-up. When planning transition and patients are in that transitional living experience, you want to start pulling back on some of those supports that you're offering and allow caregivers to work through those things that they are going to have to do at home.
Tools
We have identified several tools that tend to work well for us. To begin with, identify the caregivers as early as possible. They are going to have to be the respiratory therapist, physical therapist, and nurse so they need to understand early on what that looks like and what they are going to need to learn. We do not want to leave education closer to discharge because they are going to be very overwhelmed and it may increase the length of stay in the hospital or require having to find other means of getting them out of the hospital. It should be a very organized team effort as you work together to benefit the patient.
We make follow-up calls within 72 hours of discharge to make sure that all of their equipment arrived, what it looks like, and see if they have any questions about it. We also ask if they got all of their meds and if they need us to talk to any of their therapists about anything. We have clinics and comprehensive assessments at our facility. All of these things provide good follow-up with these patients in the continued support to help them be successful at home.
Checklists
Figure 1 is our pediatric pulmonary education checklist. It could be used for adults too, but It is important to remember that you hit every detail when you are educating people. It is important to remember that caregivers may have never even touched the equipment patients are using. Going through every little piece and nook and cranny of their care is imperative. This checklist helps identify those things to cover.
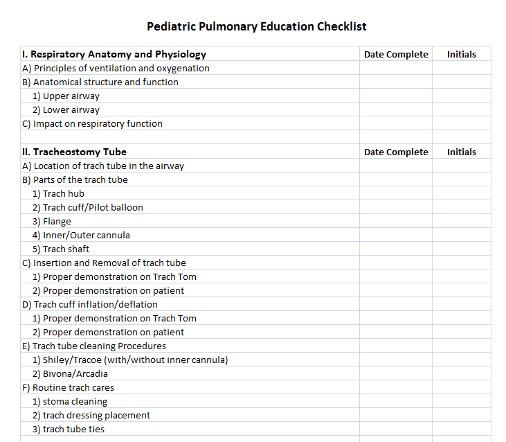
Figure 1. Pediatric pulmonary education checklist.
Figure 2 is another checklist that we have utilized in the past. Checklists are a great way to keep track of what patients need to be educated on. They are also a good visual for the family and staff to make sure that it all gets completed.
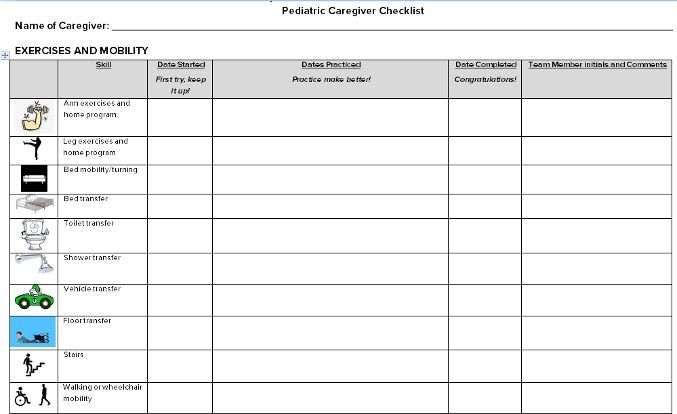
Figure 2. Pediatric caregiver checklist.
Figure 3 shows part of another checklist about bowel and bladder care, respiratory care, wound care, and nutrition. Again, when creating a checklist include everything that is important to make things successful for the patient at home.
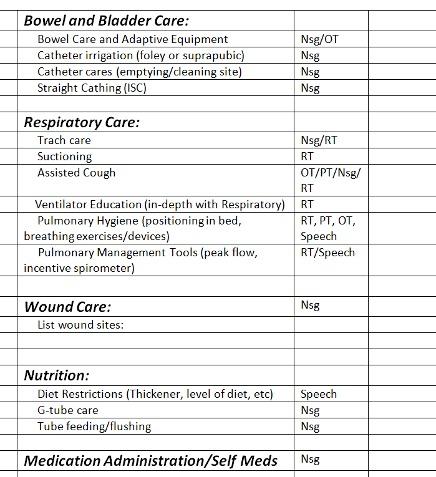
Figure 3. Sample checklist.
Caregiver Manual
A caregiver manual is a tool that helps provide consistent care. Once a patient gets home, their caregiver, whether It is someone in their family or a paid caregiver, is going to want to pull in additional help and support. Having a caregiver manual made by the hospital staff who helped that patient helps ease into that transition home. It also helps with training the caregiver. It is a good reference in case they have to go to a different hospital so they can identify what is needed for the patient's care. Examples include how they transfer and what ventilator are they on. You can also include information for early identification of any declines, flow sheets for respiratory exercises, skin logs, wounds logs, and bowel care records. It takes an interdisciplinary team and interdisciplinary approach to put that together and make it a good resource and reference. One of our manuals was written in Spanish to ensure that those patients who are non-English speaking have the education and materials in their caregiver manual.
Figure 4 is an example of something I made in the past for patients. Grouping cares is important here. When we are taking care of patients there are several people helping to take care of them, which could include the nurse, respiratory therapist, physical therapist, and occupational therapist. When the patient goes home there is one person playing all those roles. It is very important that they get on a routine and schedule and learn to group cares together. We can provide education on how to do that. For example, you're going to complete your breathing treatment, then suction, and use cough assist. Then we will place your Passy Muir Valve on and transfer. This gives a step-by-step process of what they will do. They are going to find their own groove at home, but we can provide the education for them to better understand what that might look like. For example, while my breathing treatment is going, maybe I am putting my wife's sweat pants on, or maybe while I am sitting on the commode and doing my cares, we are also brushing teeth or something else. Grouping those cares together can help decrease that burden for going home.
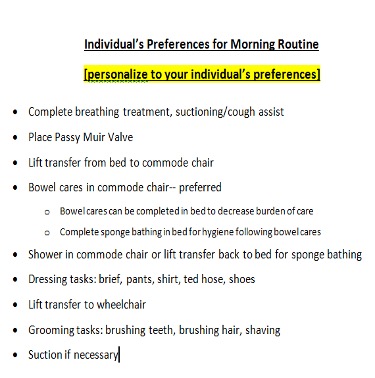
Figure 4. Sample of preferences for morning routine.
Personal Health Profile
Diane Ulmer: Melissa gave us a lot of great tools, and I will add a few others that I have in my toolbox. It is important to individualize what things can help make a family successful long-term at home. An additional tool that we encourage our patients and families to use is a personal health profile, also known as a portable health profile. There are a lot of different names and they come in a lot of different versions. There are apps, you can place them in an envelope with multiple sheets of paper that someone can just stick in a binder or in their purse, or you can load all those documents onto a flash drive to have with you. There are quick references in the form of an emergency card in case of an ER visit or evacuation.
Basically, we want them to have a really quick place to access all of their information and to find a way that fits them. My mom likes to pull out a piece of paper with all her specialists' phone numbers and names on a piece of paper. Lots of people just like to have it on their phones. Our patients are always being asked, "Who's your pulmonologist? Who's your urologist? Who saw you for that? Who did your biopsy? Who provides your trach supplies?"
A lot of individuals have supplies auto shipped to their house every month and when you ask them, "Where do you get this from?" many won't know. If they are in an emergency evacuation shelter and do not have it documented and with them, they won't be able to get their medications or supplies. When it comes down to it, I have to look in my phone to find my kids' pediatrician's phone number. The personal health profile also helps so that EMS has quick access to a medication list and all of those other important things. It also makes it easier if you have to go to the ER so you do not have to remember all of these details. It is such an important tool.
Our local children's hospitals started Project Austin with the goal of providing continuity of care from the hospital to home and increasing community awareness and education to EMS and other providers. You can search Project Austin, Nebraska, and even use some of their tools. They have resources such as documents with places to add emergency information, forms for kids with special healthcare needs, and other tools for families to have at their fingertips when they need it.
Self-Advocacy Training
I think self-advocacy training is a tool that is overlooked and maybe not thought of as a tool sometimes, because we take it for granted. However, this is training that we should be doing with our patients. Depending on the generation that your patient comes from, they may not speak up. I am helping my aging parents navigate through healthcare and have noticed they do not always speak up. They just take what the healthcare professional says as gospel truth and do not ask questions. When something does not seem right, they do not speak up. This is a skill that is important for our patients. They are the most consistent person in their care and they need to be able to advocate for themselves and to be able to direct their care. If their caregiver is ill or unable to get to the patient, the patient may need to tell their neighbor exactly how to suction them, how to do their trach care, and how to care for them until someone who is better trained can get there.
This is a skill that can also teach them how to be assertive, but in a kind way, so they can be direct with detail that does not send the caregiver running away. This is not something that comes naturally to a lot of people so we practice that a lot with our patients to help them understand they are the center of the healthcare team. We as healthcare professionals need to allow them to be that way when they are practicing. As we are directing their care, we also need to listen to them.
If they say, "Well, I really like it done in this sequence, or no, I prefer that you tie it this way or that way" we need to listen to them. If we have a better way, we can offer that, but still, respect that the way that they have been taught to do things. We can respond to them and show them that they do have a voice. Help them be involved in choosing their equipment and understanding what equipment they have. We often have patients who have previously done rehab at places that do not specialize in spinal cord injury, brain injury, or pulmonary complications. When they come to us, we realize that they do not really know what was ordered for them. We may ask them, "Is this the equipment your therapist prescribed?" and they respond with, "I am not sure what they prescribed. I just trusted I would get what I was supposed to get." It is important to help them practice that and know they have a voice to talk to their insurance company, oxygen provider, or other provider and ask those questions too. Empowering them is really important.
Emergency Preparedness
We are going to switch gears into emergency prep. At the beginning of my career, I felt like as I was preparing my patients who had experienced a catastrophic injury for home, that emergency preparedness was only something extra I would do if I had the time. But in the last five to ten years, it has felt more essential. Everywhere in our country has experienced disasters. Thinking about 9/11 as well as current issues, nobody anticipated being isolated in your home because of a pandemic or being unable to access parts of your community because of a riot, a hurricane, wildfires, flooding, tornadoes, or blizzards. Everybody's been impacted in these last several years by something.
We just recently had a storm blow through our local area, which no one was prepared for. We had people in the biggest city in Nebraska out of power for up to five days. People were in a panic and were calling the fire department saying, "I need more oxygen. I do not know what I am going to do." Melissa and I were talking about it saying, "Oh my goodness, why do not they have enough oxygen to get them through two or three days of emergency?" The providers were so inundated with calls that they were not able to return their calls. We were helping people find backup things. You cannot prepare enough. I think regardless of what level of care you work in, whether it is the ER, home health, or long-term care, all of us need to address emergency preparedness.
Can Your Patient Answer These Questions?
One way to open that conversation with your patients, regardless of what level of care you are working in, is to ask them, can you direct your care? For example, do you know what your C-PAP settings are? If you cannot remember that, let's just tape them right to the machine or put that in your caregiver manual. Can you tell your caregivers? I have trouble remembering all the details of my care, but my caregiver manual is in the backpack on the back of my wheelchair, can you pull it out? It will talk you through exactly what to do with pictures. That's a good way to start that conversation.
Do you have an updated portable health profile or do you have an emergency health card? They will probably say no and you can say, well, let's start one for you today. Educate them about how they can transfer the information to an app later, but this at least gets it started before they leave acute care or if you are a home health practitioner before you leave. A good place to start is to ask what they would need to take with them if they had to leave their home today. Do you have a go-bag or emergency bag you could just grab? What if your power went out, do you have a backup plan? If not, offer some resources and help develop a backup plan.
Melissa and I are working with our local community partners and have learned that the fire department is more than happy to come out and look at an evacuation plan with you. The electric company would love to troubleshoot generators and things like that with you. That's much better than you calling in the middle of the blizzard in a panic when they cannot help you because they are trying to reestablish power everywhere.
Ask the patient, do you know who your equipment vendors are? Is all of your equipment labeled? As we interact with different providers all over the country, they always say, no, their equipment is not labeled. This is what happened when there was flooding in Houston. I talked to an occupational therapist who was part of that recovery. EMS went around and evacuated so many people from their homes and then went back to their homes and got their medical equipment. Unfortunately, it all ended up in a gymnasium and they had no method to match people in the shelter with their medical equipment.
They had a gymnasium full of oxygen concentrators, portable suction machines, wheelchairs, and other equipment, but no way to know whose was what. That was a disaster in and of itself. So much could have been prevented if the equipment was labeled. Another way to prepare is for patients to keep bungee cords in their go-bags. When they are in a shelter, they can get use the bungee cords to gather their equipment together so that somebody does not walk by and scoot it over and becomes the next person's equipment. These are stories that are documented from natural disasters.
Three Key Aspects
We will cover three key aspects of emergency preparedness:
- Knowledge of community resources
- Effective planning
- Developing a circle of support and network providers
There are many other aspects we could cover, but we chose to narrow it down to three. We feel that these are three that have a big impact on patients being successful in the community long-term and things that they struggle with.
Knowledge of Community Resources
Working with community agencies and identifying what medical facilities can be backup shelters is vital for respiratory therapists, social workers, and families. We recently had some unprecedented flooding in Nebraska. During this flooding, we ended up housing a couple of people who were ventilator-dependent. We hadn't planned that ahead of time, we just responded. The community called us because we have experience with caring and providing that sort of equipment and caring for people. It is important to know what is available and to know what accessibility needs there are at the shelters in your community, as many of them are not accessible. Think about what could make them accessible or where else could they go that might be accessible. Explore those agencies and resources. For our spinal cord patients at Madonna, we have an educational course where we teach them about a lot of different topics. We talk about how to find those shelters and how to tackle those environmental barriers, either with a portable ramp or other backup equipment that they could request.
Contacting EMS and utility providers prior to an emergency is really important, but It is also important to help your patients not to have a false sense of security that, "Yes, my local electrical provider knows that I live on a ventilator and I have life-sustaining equipment." In the case of an outage, they assume that they are going to come to their home first because they have life-sustaining equipment. At one point in my career, I thought that too, because we know that they were registered with those companies and they were aware of them. But as we developed our relationship with our local electrical companies and did some education for their staff and had them do some for us, we realized, that is a false sense of security.
They do not respond to folks whose power is out. They do not know who has life-sustaining equipment in their home. They have it on file and look at that when someone does not pay their bill. They pull their file and see that they have life-sustaining equipment so they are not going to just shut their power off as they may in a different situation. In the case of a power outage, they are going to go where the masses are out of power. They go to help the most people first and they do not know who lives in that area. That was an aha moment for our team and how we train our patients to communicate with them as well as local EMS providers as we discharge patients to rural communities. A lot of those EMS providers are volunteers and many do not have any experience with the sort of equipment our patients have. But those men and women are ready to respond and are so helpful and ready to learn. We have had patients give short in-service training to their EMS providers on what is autonomic dysreflexia, how to move their head array or power wheelchair, and other specific issues related to them. That can be so valuable when those providers are coming to help them in an emergency.
Look at alternative transportation options. Lots of our patients use public transportation because accessible transportation of your own can be so expensive. In the case of an emergency when public transportation may not be an option, identify who else can they call that has a vehicle they may be able to fit their chair in. This could be a caregiver or a neighbor, or if they have their own vehicle, someone who knows how to drive their accessible van and manage the lift? Does that person have an extra set of keys?
Another community resource to look for is respite organizations. They are often difficult to find and have difficulties with staffing, but It is worth looking into for assistance. Do not just think about your patients, but consider the caregiver's needs as well when looking at community resources. If there is a tragedy the primary caregiver will be affected as well and could benefit from backup assistance.
Effective Planning
Effective planning is our second aspect of emergency preparedness. We cannot reiterate enough that we have to help people plan, prepare, and develop a plan for evacuation, as well as a plan for staying in your home in the midst of a blizzard, or if you are unable to evacuate. Those plans look very different. Make sure there are options for both situations and that information is quickly accessible to EMS if they do come to help. Make sure caregivers are aware of the emergency plan as well and know where to access things and how to get into the home. Consider an alternative power source or generator as well. Marvin, our case study from the beginning, went without power for nine days. They had a natural gas generator that ran all his respiratory equipment, his ventilator, as well as their entire house, including the furnace, microwave, and stove. They got through the emergency at home and did not have to evacuate. This was best because It is very difficult to evacuate someone with all of his needs and equipment. They planned ahead and were very prepared. do not forget about service animals and their needs. Sometimes when people do not have a plan for their service animal, they refuse to leave their house because they are afraid they will be not accepted at a shelter. That can put them in increased danger.
The other thing I want to mention is not only to help our patients plan for evacuation at home but think to yourself, do I know how to help the facility that I work at evacuate in the case of a tornado, fire, or another emergency? Do you know where your evacuation equipment is? Do you know where the Paris sleds are? Do you know how to use the evacuation chairs? Have you carried a human being down a flight of stairs on a Paris sled? In the case of 9/11, there were lots of stories about people with disabilities working in the Twin Towers who perished because they could not get down the stairwell. There were also testimonies of their coworkers that there was evacuation equipment available, but they did not know how to use it. The coworkers were trying to figure out how to use the equipment and were headed down the stairwell of 60 flights of stairs with someone on one of those sleds while the fire department was coming up the stairs with tons of equipment. The stairwells were too narrow to pass each other which made it a crazy situation. We cannot prepare for every scenario, but we can ask ourselves, are we ready to help our facility evacuate? Think about that and challenge each other and your team to take the lunch hour one day to practice this. Make sure all shifts know how to do this as well.
Another piece of effective planning that I think that we fail to use is our equipment vendors. We are not always able to travel as far as we want to help to look at a patient's home and talk about how they would get out and what do the different entrances look like? We do lots of things through telehealth now to look at the patient's home environment, but sometimes you just need to be in the home. Some equipment vendors will complete home visits and assist with emergency planning. They may try to determine if the equipment is sustainable or if they have the electrical capacity to even manage this equipment in their home? The wheelchair vendor may go to the home and make sure that the power wheelchair is really going to be able to get up that ramp because from the view on telehealth it does not look like It is quite to ADA specifications. Use them as an extension. Embrace the whole community and the whole team and say, "If this person is going to be successful at home and this equipment is going to be sustainable at home, can you help us actually get inside the home and make sure the family's comfortable and It is going to work."
As I've said before, keep medical information, DME providers, and other phone numbers in one place in an organized fashion so it is readily available when you need it. We provide our patients with a list of reminders for being prepared for emergencies including all of the things we have been discussing. We also provide them with a form to list their emergency contact, physicians, DME provider, and pharmacy along with their contact numbers. Again, regardless of what level of care you work in, ask them if they have this on their refrigerator so that the firefighter or other emergency worker can quickly grab it and have everything that they need. There are dozens of emergency preparedness checklists on the internet, but sometimes families are overwhelmed with the options. Giving them a blank form can be very helpful. I recently went through a healthcare crisis in my family too and it was another aha moment. They taught us all this stuff and then I got in the elevator and I thought, "Wait, what are we supposed to do? What do we do first?" If you have a patient in the ER and they seem to be a frequent flyer or you're discharging them to a different level of care, just say, "Do you have all of this information in one place?" If they do not, then offer to write it down for them. Hand it to a family member and say, "Put this on your fridge when you get home." At least It is a start in case they have to leave the house quickly so they'll have the important information available.
Circle of Support
The third key aspect in emergency preparedness is identifying and expanding someone's circle of support. As Melissa mentioned, I think the circle of support is another thing we may take for granted. We've all been in a team meeting or discharging patients and the patient says, "I do not really have any help. My brother lives an hour away. He cannot really help." We need to help them dig down and think about who else could help them. It is also important for us to give the patients permission to ask for help because they often feel like a burden. I have found here in the wonderful Midwest and I know across the country, people are almost always more than happy to help, but they have to be asked. It may make them feel good to be able to check in on you every Wednesday, pick up your groceries, or help get that online delivery going. Sharing all of those duties amongst many people takes some organization, but can really make them successful. Help them think through the community partners, independent living centers, healthcare agencies, friends, and family who might be able to help as their circle of support.
I had a patient the other day who has had MS for 20 years and she had never heard about the independent living center in our community. They could have been helping her for years with so many things. She said, "We use the internet and we order a lot of stuff on Amazon." I told her there are people out there that have resources and can help her, such as Aging Partners and Easter Seals. There are agencies that patients may not even know about that can really help.
Do not forget to look at the circle of support outside of their area because a lot of times in a huge community emergency everybody's dealing with the same disasters. The people that you would normally call on are also dealing with their own families and the disasters. Help them identify who outside of their area they could call to help and know when to go to the hospitals and when not to. They need to know what facilities can help in the time of evacuation or power outage. It is important for patients not to panic and inundate the ER if It is not needed. Instead, they need to know how to ask for help prior to getting to the point of an emergency.
Marvin's family was great about networking in his small community and they had multiple house calls from various providers. Their primary care provider actually came to their home instead of Marvin going to him. Is that rare? Yes, probably. But would it have happened if they hadn't advocated and asked? No. You may be surprised how sometimes It is incredibly frustrating to find resources and sometimes you just cannot believe how people step up.
We have also found that local churches and local colleges that have programs for healthcare careers are great resources. Nursing students often want the experience and OT students are often willing to help. Partnering with those programs to give students opportunities to learn while being supports is a great extension of what you do.
What Can You Do?
So what is next? We have all these tools ready to help our patients transition back, but big picture, what can we do? We give our families all these things to do to be prepared, but what can we do to help? Remember that we have the best knowledge and information about what our patients need.
Get involved in your local emergency planning committee to advocate for your patients and other individuals with complex medical needs. I am on one of these committees in our community and there are brilliant community planners on our committee including emergency medical providers and EMS. There are lots of people in the room, but they do not have the same perspective. For example, they have never helped someone with a power wheelchair whose battery has died get up a ramp. They are not thinking in that way. They are not thinking about how many people in the community actually live on a ventilator. Do you know that about your community? When I found out how many people in our local community lived on a ventilator I was blown away. I thought, what is our plan if we have to set up tents, where are those people going to stay? We do not have enough accessible shelters with electricity for their life-sustaining equipment. Then we broke off into a subgroup to address those needs. There are no answers to all of those questions, but we have to keep asking them. We need to, and we are the best people to help them. We might not have the answers, but we are the best people to be asking those hard questions about what are we going to do about John and Betty and their child? These people have real needs and you know what they need.
You can also collaborate with your electric companies and other utility companies in your area. Get to know your policymakers and those with the legislature who are passing laws that restrict access. Many times they do not even realize they have negative effects. I've recently gotten involved with our Nebraska OT Association. To be honest with you, I was scared of talking to a Senator and our mayor until they started making some less than optimal choices for the people we serve. I realized they are people too and they just do not know, but they want to know. do not be afraid to empower yourself and empower your patients to be good self-advocates.
Case Study - Now
Marvin was at home for 10 years with very high physical and respiratory needs. He was only rehospitalized three times and none of those were for pulmonary reasons because he had incredible support, an incredible plan, a backup plan, a plan B, and a plan C. This allowed him to be able to stay at home in his community with his family.
Resources
Here are some resources to utilize as you support patients and their families. do not take for granted the things that are at your fingertips and the organizations and associations that have tons of resources on their websites.
- American Red Cross
- www.redcross.org or www.prepare.org
- Federal Emergency Management Agency
- www.fema.gov
- National Spinal Cord Injury Association
- www.spinalcord.org
- National Organization on Disability
- www.nod.org
- Ventusers.org
- Easter Seals
- https://www.easterseals.com/
- Family Caregiver Alliance
- https://www.caregiver.org/
- State Specific Assistive Tech Programs
- https://www.christopherreeve.org/
- http://www.agrability.org/
- Smiths Medical adult home care trach guide-Spanish
- Smiths Medical adult home care trach guide-English
- VTA Application on mobile phone
- Med Wish Low-cost supplies and equipment
- https://www.medwish.org/
- https://www.medicaid.gov/medicaid/long-term-services-supports/pace/programs-all-inclusive-care-elderly-benefits/index.html
- https://www.ready.gov/
- Official website of the Department of Homeland Security
- Plan ahead for disasters
- https://www.ready.gov/individuals-access-functional-needs
- Individuals with disabilities
- Building a kit – special considerations for individuals with low vision, mobility impairments, communication difficulties
- www.phe.gov/
- U.S. Department of Health & Human Services
- Sheltering in place and evacuation checklist
- www.disabled-world.com/disability/emergency/
- Disability, Disaster and Climate Change Emergency Planning
- www.flash.org/peril_inside.php?id=42
- Federal Alliance For Safe Homes
- Floods and people with disabilities
- http://www.portlight.org/
- Inclusive disaster strategies
I think Easter Seals is something that is underutilized. They have low-interest loans for vehicles and other DME equipment that are not covered by insurance, such as evacuation equipment. Those may seem non-essential and the costs may seem prohibitive, so they are the last things people get, or they never get but are really important. More people would get them if they had a resource to help them. The Christopher Reeves Foundation is great. They have people that can interpret education materials into many languages. If you serve areas that are rural, Agra Ability provides amazing rural solutions that can help overcome a lot of physical barriers and getting people back into that rural community.
Med Wish is another resource we found recently that provides very low-cost supplies and equipment for those who are uninsured. Patients also need a way to sustain replenishment of supplies. If they are uninsured, that is a great resource for them as well. There is a home care trach guide in both English and Spanish listed here for you as well. Since disaster preparedness is such a hot topic now, a lot of people have stepped up their websites in helping people build an emergency preparedness kit to have, regardless of their impairments. These can assist patients like we have been talking about, but also those with low vision, communication difficulties, or other challenges and disabilities. Another great resource is www.phe.gov where one of the things they cover is sheltering in place. Many of us feel like we've done that over the last year.
If you do nothing else today, put a sticker on somebody's equipment with their name and phone number on it. Start small and help the patients get prepared. Thanks for all you do as respiratory therapists!
References
Agtarap, S., Carl, E., Reynolds, M. C., Roden-Foreman, K., Bennett, M., Rainey, E., Powers, M. B., Driver, S., Warren, A. M. (2020). Caregiver expectations of recovery among persons with spinal cord injury at three and six months post-injury: A brief report. The journal of spinal cord medicine, 43(1), 122–125.
Peterson, B. (2019). Preparing to Transition Home. Christopher & Dana Reeve Foundation.
Ronca, E., Scheel-Sailer, A., Koch, H.G., Essig, S., Brach, M., Münzel, N., Gemperli, A.; SwiSCI Study Group. (2020). Satisfaction with access and quality of healthcare services for people with spinal cord injury living in the community. J Spinal Cord Med, 43(1),111-121.
Rennke. S., Ranji, S.R. (2015). Transitional care strategies from hospital to home: a review for the neurohospitalist. Neurohospitalist, 5(1), 35-42.
Kansagara, D., Chiovaro, J. C., Kagen, D., Jencks, S., Rhyne, K., O'Neil, M., Kondo, K., Relevo, R., Motu'apuaka, M., Freeman, M., Englander, H. (2015). Transitions of Care from Hospital to Home: An Overview of Systematic Reviews and Recommendations for Improving Transitional Care in the Veterans Health Administration. Department of Veterans Affairs (US).
Citation
Ulmer, D., Gulizia, M. (2021). Preparing complex medical patients for successful community integration. Continued - Respiratory Therapy, Article 91. Available at www.continued.com/respiratory-therapy

