Editor’s note: This text-based course is an edited transcript of the webinar, If You Cannot Breathe, You Cannot Swallow...Breathing and Swallow Coordination in Respiratory Disease, presented by Angela Mansolillo, MA/CCC-SLP, BCS-S.
Learning Outcomes
After this course, participants will be able to:
- Recognize three components of respiratory and swallow coordination in healthy individuals
- Describe the impact of disordered respiratory and swallow coordination in individuals with respiratory disease
- Explain two interventions to improve respiratory and swallow coordination
Respiration and Swallowing
- During swallowing, airway closes to prevent aspiration:
- Vocal fold adduction
- Laryngeal valve closure
- Laryngeal excursion
- Epiglottic-arytenoid closure
- Epiglottic retroversion
- And...
- Breathing cessation
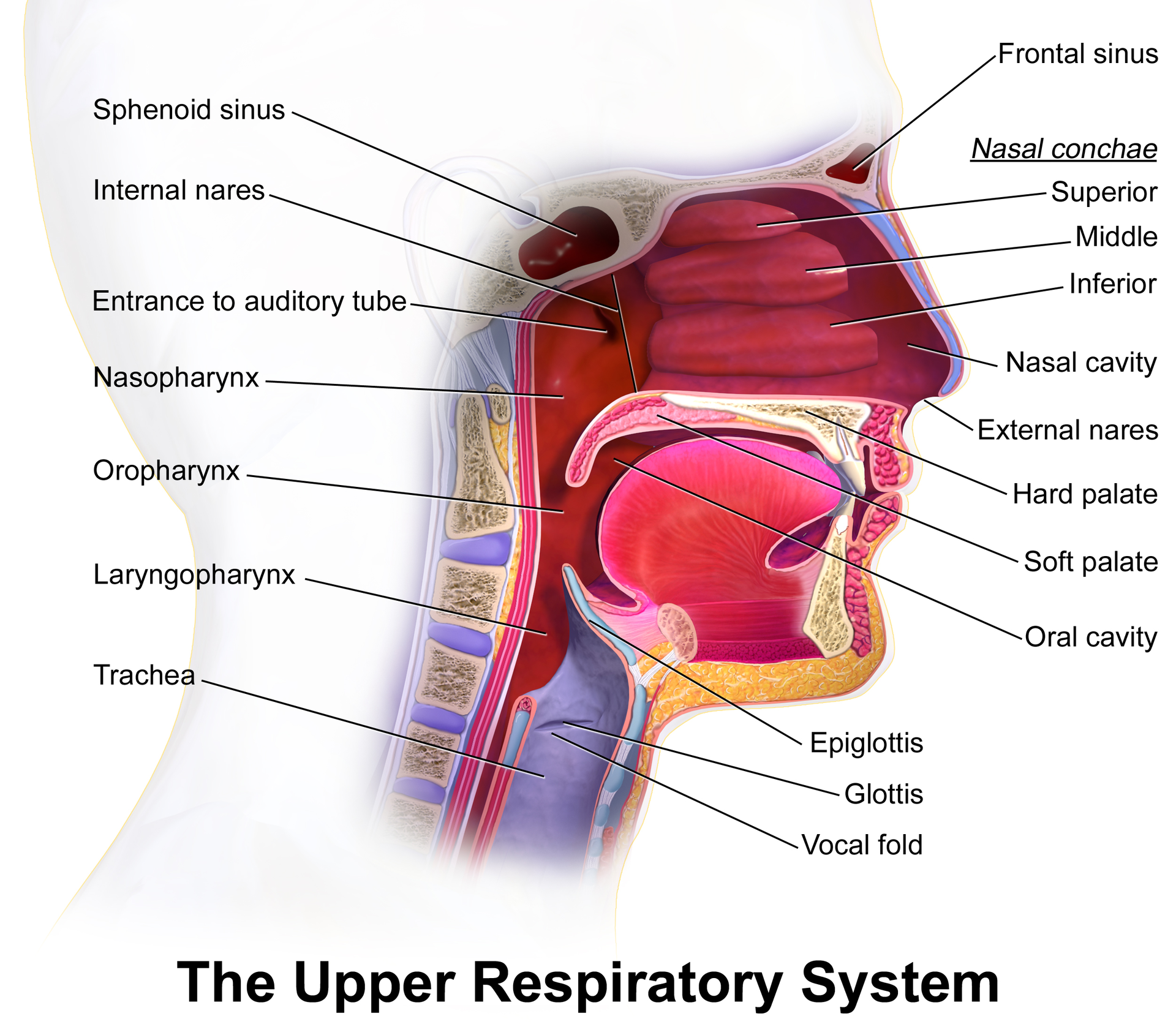
Figure 1. Upper Respiratory System (CC by 3.0 Blausen 0872 UpperRespiratorySystem).
Let's start by discussing respiration and swallowing and how the two work together (Figure 1). During the swallow response, we know that the airway closes. That is an important mechanism to prevent aspiration, but what is happening? The vocal folds are adducting, and the laryngeal valve is closing due to that adduction and movement of the false vocal folds. The laryngeal excursion is initiated, which is the upward and forward movement of the larynx guided by hyoid movement. The muscles that are attached to the hyoid provide that laryngeal lift. There is epiglottic-arytenoid closure. As the larynx is elevating, the epiglottis is retroverting, and we want that contact between the underside of the epiglottis and the arytenoid to help seal off the airway further as the epiglottis is going into retroversion during the swallow responses.
Swallow Apnea
Most importantly of all, breathing stops. We do not breathe and swallow simultaneously, so that period of breathing cessation, swallow apnea, or respiratory pause, whatever term you prefer, is critical to airway protection during swallowing. It is also variable; every aspect of the swallow response has some normal variability, which is valid for the period of respiratory pause. We know changes occur depending on the bolus, the type, and particularly the size of the bolus. Not surprisingly, as boluses increase in size, whenever you take a larger bite, you take a larger sip, the duration of the respiratory pause increases, and the onset is a little bit earlier.
We also see changes in respiratory pauses associated with different patient populations. As we age, we are not talking about patient populations here but a healthy aging population. We see these normal changes in respiratory pause, no change in onset, but longer durations across bolus sizes. So even with smaller boluses, we see a little lag in our healthy elderly as they get back to breathing after the swallow has completed itself. More importantly, from our perspective as clinicians, we see much difference in respiratory pauses associated with various disabilities. When the underlying cause of the dysphagia is neurological, or in patients with neuromuscular diseases like ALS, Cerebral Palsy, or premature babies, we tend to see longer than typical periods of respiratory pause.
When the underlying cause of the dysphasia is respiratory, our patients with COPD, for example, might see shorter periods of respiratory pause. Breathing is difficult, and breath-holding is critical to airway protection during the swallow is challenging to maintain when you cannot breathe very well. We see shorter than typical periods of respiratory pause because these folks have to return to breathing as quickly as possible. The typical pattern for breathing swallow coordination is exhaling a little, swallowing, and exhaling some more. The swallow typically interrupts the exhalation fairly early in the exhalatory part of the process.
Respiration and Swallowing
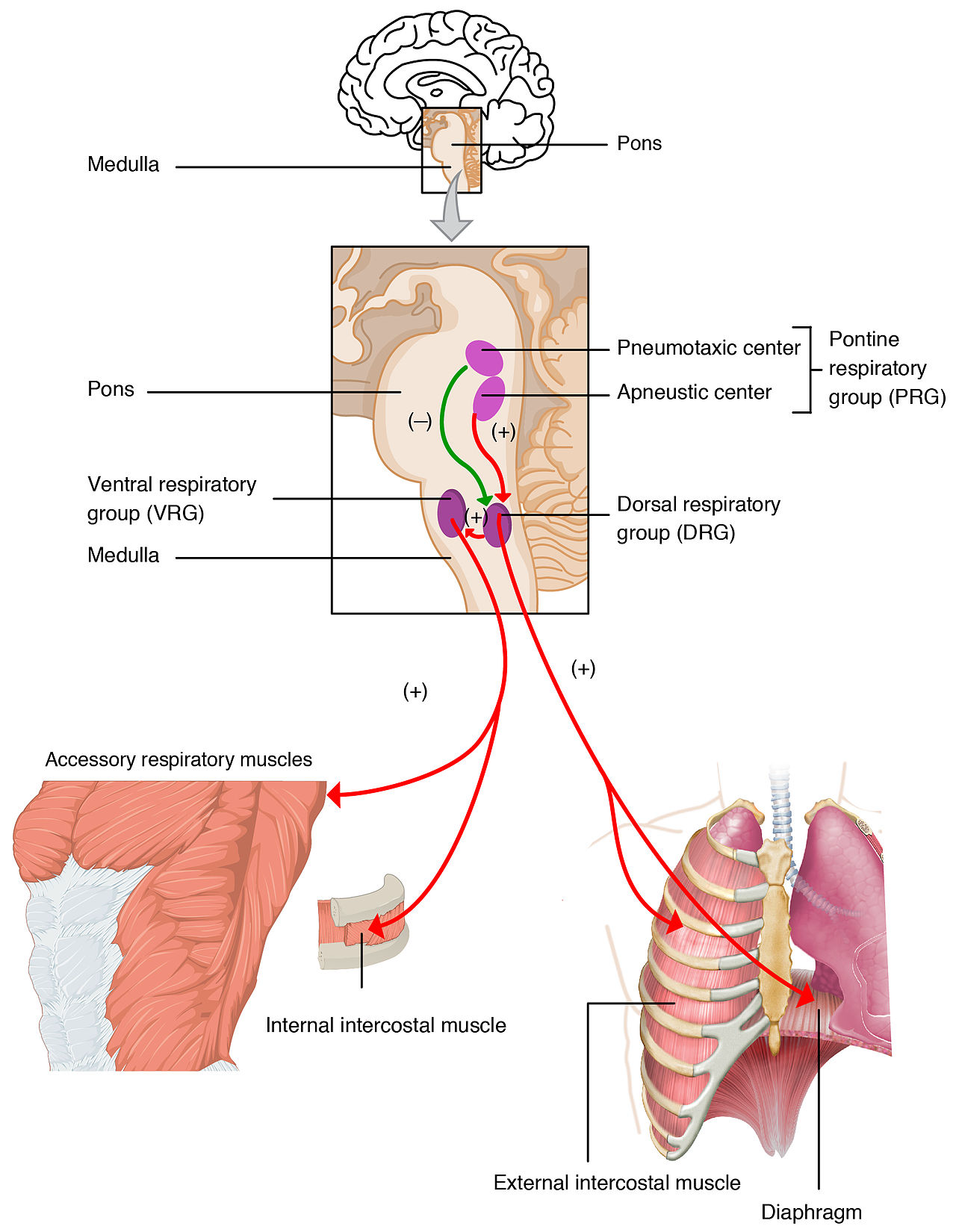
Figure 2. Respiratory Center (CC by 3.0 Respiratory Centers of the Brain).
We know that there is quite a bit of brainstem control over breathing and swallowing (Figure 2). It is not surprising to know that the central pattern generator for respiration and the central pattern generator for swallowing are very much intertwined and communicate with each other in the brainstem. A relatively sophisticated degree of coordination occurs between these two systems. Large boluses, thin liquid boluses, fast-moving boluses, and serial swallows- represent three of the more challenging swallow tasks. When we do these three somewhat challenging swallow tasks, we do it at higher lung volumes. Your brainstem says, "Oh, it will be a little tricky. Let's ensure we have enough air to get us through these more challenging swallows."
Lung Volumes
I will add a caveat that the data around large boluses is equivocal. There is a lack of agreement in the literature about what constitutes a large bolus, we do not have much information about what average sip sizes are and that sort of thing, so it makes defining a large bolus a little tricky.
- Why?
- Is more oxygen reserve available for 0-2 saturation?
- Enhanced expiratory pressure to reduce aspiration risk?
- Swallows at lower lung volumes (end-expiration) more likely to result in aspiration May contribute to breathing-swallow discoordination – decreased feedback from pulmonary stretch and/or subglottic pressure receptors to the respiratory Central pattern generator (CPG)
Indeed, we see that these swallows are occurring at higher lung volumes within liquid boluses and with serial swallows. I am not suggesting that every time you take a sip of water, you fill your lungs to get through it, but swallowing occurs in the mid-range of lung volume. These more challenging swallows occur at the higher part of that mid-range. We have to have some assurance that if we want safe swallowing, our patients can at least get to the middle part of the lung range comfortably and repeatedly. We need that oxygen reserve available because of this period of breath-holding and this potential lack of oxygenation. As brief as it is, think about the demands swallowing places on the respiratory system. It means repeatedly holding your breath briefly, but over, and over, and over, until whatever time it takes for you to complete your meal. It puts much stress on the respiratory system, mainly if we are talking about a respiratory system that already has some compromises.
The other physiological reason for needing to swallow at a slightly higher lung volume might be to do with airway protection. That enhanced expiratory pressure if you are swallowing at a middle-range lung volume might also help with that exhalatory clearance we discussed a moment ago. We know that when swallows occur at lower lung volumes (near the end of the exhalation, in other words), they are more likely to result in aspiration. Research supports this in patients with COPD and those of us who are "normal breathers" and "normal swallowers." When we get into trouble, we choke or aspirate on something, usually because we were eating and drinking while talking or laughing. Our breathing swallow coordination was off, and we were near end exhalation, so we inhaled when we should have been exhaling, and it gets us into trouble. Even with typical systems, we will sometimes get into trouble regarding this breathing swallow coordination. Suppose we are swallowing at lower lung volumes. This may contribute to discoordination relating to changes in feedback, which the individuals receive from the subglottic pressure receptors.
Breathing and Swallowing
- Mastication (Chewing)
- Appears to disrupt respiratory cycles
- Airway is open, breathing, during mastication...and during bolus aggregation in the pharynx (Matsuo et al, 2008)
What about boluses that require mastication? Mastication does seem to further impact breathing, swallow coordination, and respiratory cycles. While you are chewing, the airway is open. You are breathing while managing that food, manipulating it, breaking it down in your mouth. Sometimes, depending on the food you are eating, it could be a somewhat prolonged process, so we continue to breathe while we chew. However, if you are someone who loses control of that bolus and it falls back into your pharynx, the airway is going to be open. That is an important consideration, understanding why some patients have more difficulty with solid boluses than liquid boluses.
Impact of Hypercapnia
Nishino et al. (1998) is an old study, but it is an interesting study. The study took a group of healthy subjects and induced hypercapnia during serial swallow tasks. They found that swallow frequency decreased. The subjects swallowed less frequently and were likelier to demonstrate a post-swallow inhalation. In other words, they were getting air hungry. Primarily, it revealed more coughing associated with the post-swallow inhalation.
Respiratory-Swallow Coordination
- Respiratory-Swallow Patterning (exhale-swallow- exhale)
- Lung Volume Initiation (low-middle to middle lung ranges or 42-55% of vital capacity)
- Respiratory Pause Duration (0.5 to 1.5 seconds) (Curtis et al, 2019)
Logically, when you cannot breathe well, you may not swallow safely. Your body will say, "Nope, cannot swallow right now, we have to keep breathing." It is important to remember that the swallow requires breathing cessation. As we think about this concept of respiratory swallow coordination, we are talking about three components 1) exhale, 2) swallow pattern, and 3) exhale some more. Lung volume initiation: We are looking for low, middle, to middle-range lung volumes for which the swallow occurs so that we can safely and efficiently get through that period of breathing cessation. Moreover, we are looking for a period of respiratory pause or swallow apnea between 0.5 and 1.5 seconds. Again, lots of variabilities here.
Respiration and GI Functions
- Consider:
- Pressure relationships
- Energy relationships
- Innervation
- Aspiration
Let's bring digestion into this discussion of interrelationships between systems. As we think about how the respiratory and gastrointestinal (GI) systems interact, we want to think about pressure relationships, energy relationships, innervation, and of course, we have to talk about aspiration. Let's start by talking about pressure relationships. The respiratory and GI systems are adjacent to each other, and they interact in several ways, not the least of which is they press on each other. When there is an expansion of the lungs, the expansion of the respiratory system puts pressure on the esophagus and stomach. Patients with COPD with mildly hyper-inflated lungs have increased reflux because those hyperinflated lungs are pressing on the stomach and the esophagus. Patients with increased stomach and esophageal distention related to GI problems are more likely to feel and report shortness of breath. The inflated GI system is pressing onto the respiratory system, and those pressure relationships are essential.
Pressure Relationships
- Crural muscles of the diaphragm are critical to the competence of the lower esophageal sphincter (LES)
- Postural stability decreases with increased respiratory effort; resulting in increased gastroesophageal reflux (GER)
- Constipation, and pharyngeal dysphagia correlated with reductions in maximal expiratory pressure, and maximal inspiratory pressure in patients with MD and NIPPV (Lee et al, 2020)
- When inspiratory pressures increase, the LES barrier can be overcome, resulting in reflux
- So...“exaggerated ventilatory effort, as occurs with exercise or in resp distress, can result in GER” (Avazi et al, 2011)
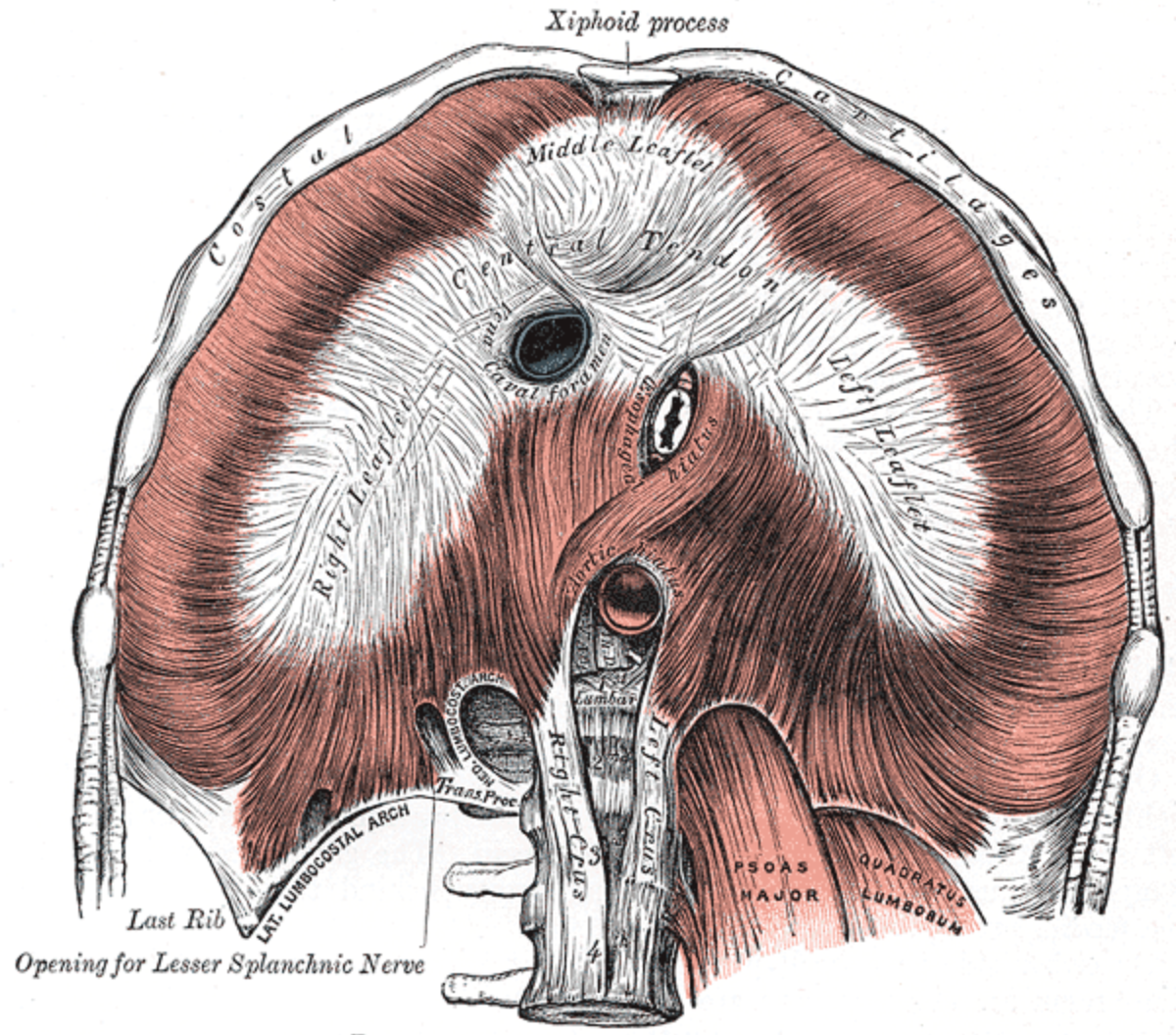
Figure 3. Crural muscles of the diagram (Public Domain).
Figure 3 illustrates that the crural muscles of the diaphragm are essential to keeping the lower esophageal sphincter (LES) in alignment and functioning appropriately. Suppose there is any pressure on the diaphragm, then there is likely to be pressure on that lower esophageal sphincter. It is potentially going to impact gastrointestinal functioning reflux. We know that the respiratory muscles are also part of the muscles that make up the core. The core is crucial for postural stability. If respiratory compromise is related to muscle function, there is likely to be some postural instability. Think about what we were saying a moment ago regarding lung volumes. If you have a patient who does not have good postural stability, who has much weakness, respiratory muscle core weakness, that is a whole lot more difficult for them to expand their lungs and get to the middle part of the lung range, which is critical to safe swallows.
You see all of these interrelationships starting to come into play. We also know that when there are pressures in the GI system like constipation or pharyngeal dysphasia, it often correlates with reductions in expiratory and inspiratory pressures. Specifically, in patients with neuromuscular disease, this has been well-documented. Lee et al. (2020) looked at two groups of individuals: athletes and people in respiratory distress. What do those two groups of people have in common? They are working hard to breathe. It turns out that when those inspiratory pressures increase, the LES pressure can be overcome, resulting in more reflux.
Energy Relationships
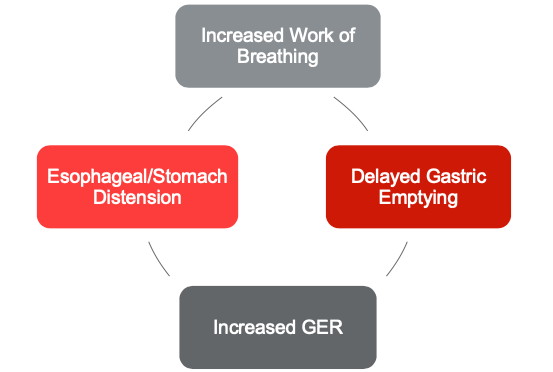
Figure 4. Energy Relationships.
When we see exaggerated ventilatory effort, no matter the cause, it can increase reflux. What that means for some of our compromised patients is that they get into a cycle of dysfunction. They work hard to breathe for whatever reason, putting pressure on the GI system and increasing reflux. The increased reflux results in more stomach and esophageal distension, which puts more pressure on these already compromised lungs, resulting in even further work of breathing. We see these folks kind of get into these cycles where the respiratory system and the GI system are just kind of at odds with each other. These patients are working hard to breathe, and we must think a little about energy relationships (Figure 4). At any moment, we have a finite amount of energy available to us. For most of us, it is plenty. For those of us who are healthy, we have the energy to spare. You may not feel that way at the end of every day, but you have the energy to spare to keep your body going. Patients with many medical compromises do not have the energy to spare. Thus, when there is insufficient energy, organ systems have to compete for the available energy. In any competition, breathing always wins. Your body always says, "Yeah, we are going to breathe right now, we will do some of those other things later." One thing that happens is that the work of breathing increases, and the energy goes to breathing. Well, that energy has to come from somewhere and often comes from digestion. So as the work of breathing increases, digestion slows. Unfortunately, when digestion slows and reflux increases, the esophagus distends, putting pressure on this already compromised lung, and we are back in that loop again.
But also...Vagal Nerve Impacts
- “Reflux cough” is sometimes the result of esophagobronchial response
- Perfusion of acid in the esophagus results in bronchoconstriction
It is not just about pressure and energy, however. It is always more complicated than that in the body. We also know that the vagal nerve has some role to play here. We often hear about folks who struggle with reflux and who have a reflux cough. The assumption is that the patient is coughing because the reflux is coming up into the pharynx and interacting with the airway, so they cough to protect the airway. Now, in some individuals, that is the case. In comparison, that is not always what is going on, as we know that the reflux cough is sometimes more of a bronchial response when the esophagus is exposed to prolonged durations of acid exposure, which triggers a response, a bronchoconstrictive response in the lungs.
Aspiration
- Consequences of Aspiration of Gastric contents
- Asthma exacerbations
- COPD exacerbations
- Chronic cough
- Bronchiolitis
- Respiratory difficulties
- Pneumonia
The acid exposure in one part of the system triggers a response in another part of the system. We also have to think about aspiration because that is often a link between the respiratory and GI systems. It is dangerous to aspirate reflux or gastric contents. Aspiring stomach contents, particularly acid, can make asthma harder to control and may result in COPD exacerbations, hospitalizations, chronic cough, bronchiolitis, shortness of breath, and aspiration pneumonia. Aspiration pneumonia is caused by aspiration of gastric contents as often as they are caused by aspiration of food and liquid. We see patients with aspiration pneumonia or recurrent aspiration pneumonia.
The Perfect Storm
- GERD and COPD
- Flattened diaphragm in COPD results in decreased abdominal pressure (muscle lowers to a lesser degree) and increased lung volume – LES is misaligned
- Hyperinflated lung compresses esophagus, stomach
- Aspiration of reflux triggers COPD exacerbations
- Increased WOB slows stomach emptying
- Bronchodilators lower the tone in the LES
- Chronic hypoxia deoxygenates gastric mucosa, alters pH; impairs the integrity of the mucosa
- Reductions in airflow increased coughing lower tone in LES
- Stress of dyspnea triggers reflux episodes
Of course, we have to look at swallowing, but we also have to consider reflux as a potential cause. Thinking about our patients with reflux disease and COPD illustrates the perfect storm of harmful interactions between the respiratory and GI systems. Everything that can go wrong between the two systems potentially goes wrong in this patient population. Several things are happening here. Hyperinflated lungs in individuals with COPD often result in a flattened diaphragm that decreases abdominal pressure and facilitates increased lung volume while pulling the LES out of alignment. Remember, the diaphragm's crural muscles are critical in keeping that lower esophageal sphincter aligned. If the lower esophageal sphincter is pulled out of alignment, it does not close as efficiently, and reflux occurs more frequently. Once you have refluxed and potentially aspirated stomach contents, that will trigger an exacerbation of COPD.
The other thing that is potentially happening with these patients is medication effects. We know that some medications, like bronchodilators, can impact the lower esophageal sphincter and lower the tone in the LES. If the LES does not close, stomach contents move up and into the esophagus, increasing reflux and pressure. There are several other relationships here as well. Chronic hypoxia associated with COPD deoxygenates the gastric mucosa and has the potential to change the pH and impact the integrity of the mucosa. In other words, it is less likely to heal and regenerate with continuous exposure to the acidic environment. Not so much more reflux physiologically, but more damage potentially associated with those reflux episodes.
Dysphagia and COPD Exacerbations
Reductions in airflow and increased coughing also tend to lower the tone in the lower esophageal sphincter. We have to talk about stress here. There is a physiological relationship between stress and reflux episodes, and it is related to the fight or flight response, which is an ancient response that goes back to early human beings. When we are under stress, several things occur physiologically. The important thing from our perspective today is that when you are under stress, blood flow shifts away from the core, organs, digestive system, and extremities, then digestion slows. The stress of having difficulty breathing moves people into this chronic fight or flight mode. Slow digestion results in more reflux, putting more stress on the respiratory system. What happens in one part of the body affects what happens in other parts of the body. It is certainly a truth we cannot get away from here. We have folks who have COPD and are dyspneic, which impairs their breathing and swallowing coordination. Perhaps they are aspirating, and that aspiration leads to an exacerbation of the COPD, and around and around we go.
Mechanically Ventilated Patients
- Significant increases in GER:
- Dry mouth/reduced salivary clearance
- Medication effects (e.g sedatives)
- Supine body position
- NG tube
- Impaired gastric motility
- Low LES pressures due to sepsis, hypoventilation
Let's talk about our patients who are mechanically ventilated. We know these folks have a significant increase in reflux episodes for several reasons. These are complicated patients, so anything that's going on with them is usually multifactorial, but one of the things is dry mouth or reduced salivary clearance. What is the relationship to saliva here? Why does saliva matter? Saliva is quite an amazing fluid and has a lot of different physiological functions. Reflux management is one of those functions, in addition to wetting the mouth and allowing for better muscle movement within the oral cavity. Natural antacids in our saliva help neutralize acid, plus the mechanical act of swallowing your saliva clears your esophagus. So saliva swallows are essential to reflux management on a regular daily basis. Many mechanically ventilated patients have dry mouths, so they have lost access to the saliva for clearance and acid-neutralizing mechanisms. We also know that they have reflux for other reasons. They might have sedating medications on board and are often supine for long periods. In many cases, they have nasogastric tubes in place, which may facilitate more reflux by propping open that lower esophageal sphincter. They have impairments in gastric motility because of the stress on the system. Ladopoulos et al. (2018) documented that half to three-quarters of mechanically ventilated patients experienced at least one episode of pulmonary aspiration directly related to reflux. It is undoubtedly an issue that we need to be aware of.
What Do We Know About Specific Disease and Conditions?
Let's talk a little bit now about what we know is going on with specific diseases in specific respiratory conditions. We have been talking a bit about our patients with COPD. I will not belabor this, but we know they have impaired swallowing. They have impaired breathing and swallowing coordination. They are more likely to swallow at lower lung volumes and demonstrate the post-swallow inhalation we discussed earlier, particularly with boluses that require chewing or more oral manipulation. We talked about that how chewing throws off the breathing swallow coordination. That hyperinflated lung pulls the larynx into a lower resting posture, which means it has farther to go during the swallow.
Patients with Chronic Obstructive Pulmonary Disease (COPD)
Cerebral Vascular Accident (CVA)
What about our patients who have had strokes? The studies are not consistent, which is not surprising because we would expect to see differences depending on the stroke's severity and location. We see some discoordination related to a more frequent post-swallow inhalation pattern (Leslie et al, 2002). That does seem to be related to stroke and dysphagia severity. We see differences in breathing swallow coordination in this population, although we expect much variability (Butler et al, 2007).
Neurological Disorders
What about patients with neurological disorders? Hadjikoutis et al. (2000 ) looked at breathing swallow coordination, but their subjects were quite heterogeneous. This group has several neurological disorders: brain injury, stroke, and motor neuron disease. In general, they found a tendency for more post-swallow inhalation. Patients with motor neuron disease were likelier to demonstrate changes in swallow apneic response and particularly more prolonged periods of swallow apnea. They would stop breathing to swallow but had trouble getting back to breathing once the swallow was complete, as you would imagine would be reasonably fatiguing.
Neuromuscular Diseases
Terzi et al. (2007) study explicitly focused on patients with neuromuscular disease, but they had some patients with tracheostomies who were ventilator-dependent and some who were not. In general, they saw a tendency toward more frequent post-swallow inhalation patterns and piecemeal deglutition, meaning patients needed several swallows to manage a single bite or a single sip. They were pacing it out over several breathing cycles. As larger boluses require more extended periods of respiratory pause, that may be unmanageable in folks with neuromuscular diseases.
Restrictive Lung Disease
What about our folks with restrictive lung disease? Our patients with neuromuscular diseases might fall into this category. More acutely, we are talking about people with acute respiratory distress. We tend to see a more rapid shallow respiratory pattern that is fatiguing, often associated with respiratory muscle weakness. Thus, we see what is very concerning in this group in terms of airway protection is a lack of limited ability to cough and clear. That is certainly problematic in terms of managing secretions, but also terms of response to potential aspiration.
Parkinson’s Disease
In Parkinson's disease, we generally see shorter periods of respiratory pause, and those periods seem to be associated with more aspiration and more post-swallow inhalation. These patients are swallowing at lower lung volumes across bolus types as well. In this population, almost every aspect of breathing swallow coordination has the potential for impairment (Gross et al, 2008; Troche et al, 2011).
Cerebral Palsy
These are some studies primarily with adolescents with cerebral palsy and saw a tendency toward post-swallow inhalation and more extended periods of swallow apnea. They saw much variability. Depending on the study, there were varying amounts of variability. The variability was bolus-dependent, specifically in terms of viscosity and thickness (Mishra et al, 2019; Rempel & Moussavi, 2005; McPherson et al, 1992).
Head/Neck Cancer and Laryngectomy
Brodsky et al. (2010) study included patients with head and neck cancer. They were more likely to demonstrate a post-swallow inhalation pattern. That inspiratory bracketing was associated with more airway compromise. We have a few studies (Fullerton et al, 2020) that look specifically at patients who were post-laryngectomy and found that they were also presenting with impairment in terms of breathing and swallowing coordination. Charbonneau et al. (2005) study did not see a change in patterning, but they did see a change in the duration of swallow apnea.
Obstructive Sleep Apnea
- Has been associated with...
- Delayed swallow response
- Longer respiratory pause
- Increased dwell times and pharyngeal stasis
- But...
- Low frequency of aspiration
- And...
- Not associated with severity of OSA
- Why?
- Chronic hypoxia? Sensory changes? Neural injury?
- May resolve with CPAP treatment (Schindler et al, 2014; Wang et al, 2016; Shah et al, 2018, Caparroz et al, 2019; Ghannouchi et al, 2016)
We sometimes pretend to look at homogeneous populations, but we can see that we are not. We can expect variability from individual to individual. There has been recent interest in swallow function in patients with obstructive sleep apnea (OSA). They have changes in terms of swallow response, not much aspiration, but some delays and inefficiencies in the swallow responses. Nobody is entirely a hundred percent sure why this is occurring. There are several theories. Some of it is related to chronic hypoxia that patients with OSA experience might be there might be some neural injury. In other words, does dysphasia improve? We are not so sure about that. In some cases, it seems to, but not in all cases. We are not sure precisely what is going on, but it is essential to know that patients with obstructive sleep apnea potentially have some baseline swallow dysfunction.
- OSA: Post-surgery
- Uvulopalatopharyngoplasty; coblation channeling of tongue; radiofrequency ablation of the tongue base, soft palate
- Odynophagia
- Laryngeal penetration
- Reduced hypopharyngeal pressures; increased stasis
- Reduced UES opening
- Globus
- GER (Kato et al, 2017; Schar et al, 2017; Corradi et al, 2018)
We also see these patients experiencing swallow difficulties after surgical correction. Some patients for whom the CPAP is not working or the CPAP is just too unpleasant will opt for surgical interventions. Uvulopalatopharyngoplasty (UPPP) is surgically resecting a portion of the uvula and soft palate. There are also less invasive techniques where they do ablations or coblations, decreasing the tongue base mass to improve respiration during sleep. Most of these patients do very well overall, but some have swallow impairments following these surgeries, so we sometimes see them in the clinic post-surgery because they are having some difficulty.
Congestive Heart Failure
- Fluids leak into alveoli (pulmonary edema) or pleural space (pulmonary effusion)
- Pulmonary hypertension – forces fluid into alveoli
- Fatigue and breathlessness with eating
- Work of breathing can exacerbate cardiac condition
High Flow Nasal Cannula (HFNC)
For patients with congestive heart failure, what happens here is that fluid sort of starts to accumulate in the alveolar and the pleural spaces. They are experiencing breathlessness quite a bit, and eating is a challenging task. Remember the demands that swallowing places on the respiratory system. Thus, these patients will have much fatigue around eating and swallowing, and the increased work of breathing then that we see during eating can be an exacerbating condition. We have to help these patients put some compensatory strategies in place.
The relationship between high-flow nasal cannula and swallowing is not well-studied. We know that a high-flow nasal cannula has many benefits. It helps reduce atelectasis, improves gas exchange, and is more comfortable for people, but we do not know much about what that means in terms of swallowing. We are just beginning to see some data. We know that pressure in the pharynx increases as the flow increases (Parke et al., 2009). What does that mean for swallowing? It probably means it will require increased muscular effort to counteract those pressures during swallowing. The patient would require a more robust swallow to safely swallow with a high-flow nasal cannula. That may be a problem considering the population of patients using a high-flow nasal cannula. They are not usually the most robust group of patients. I think, even in the absence of such data, we can presume that this is going to be a group of folks who are at risk for swallow dysfunction and for potential aspiration related to whatever got them to the place where they needed the oxygen support in the first place and potentially related to the oxygen support itself.
Tracheostomy
- Subglottic pressure changes
- Loss of expiratory airflow – cough, sensation,
- taste, smell, voice
- Decreased PEEP secondary to opening the valve – decreases the potential for oxygenation
- Cuff issues – esophageal impingement can result in reflux, trauma, decreased transit
- Inability to Valsalva – toileting, exercise, equilibrium
Approximately 30 – 50% of patients with tracheostomy demonstrate aspiration (Skoretz et al, 2020). Aspiration may be higher in older patients and is often silent aspiration. In other words, aspiration without a protective airway response. Most of it seems to occur in those first few weeks after the tracheostomy placement is placed. We cannot pretend that this is a homogeneous group of folks, it is widely heterogeneous, and therefore the swallow outcomes are widely variable.
No patterns here necessarily to look at. When the tracheostomy is in place, it creates some physiological changes. It certainly has the potential to impact swallowing. Subglottic pressure changes, perhaps most importantly, loss of expiratory airflow, the expiratory airflow through the trach means little to no airflow through the upper part of the airway. No airflow through the larynx means impaired cough, impaired laryngeal sensation, impaired voice, tastes, smell, and decreased PEEP, which decreases oxygenation potential. There are cuff issues in some patients. If the cuff is not well-managed and is over-inflated, that can create some esophageal issues. We know that there are these issues at baseline with any patient with a tracheostomy that could potentially be impacting swallow function. Then you have to ask yourself, why did this person need the tracheostomy in the first place? The list goes on trauma, brain injury, stroke, and respiratory disease—the potential for a swallow dysfunction sort of gets laid on, right on top of all that.
Mechanical Ventilation
- Disruption of normal apneic interval and subglottic
- pressures
- Separates respiratory/swallowing systems - disrupts coordination
- Air escape through mouth, nose further disrupts coordination
- Complicated by: medications, prolonged inactivity, underlying neuro, pulmonary illness, intubation trauma, trach tube
- But...swallowing may be more efficient for some when work of breathing is shared by ventilator
Our patients who require mechanical ventilation are an interesting group regarding swallow function. We have been talking about breathing swallow coordination here, and here is a group of patients for whom one of those things is not entirely within their control. Breathing is not wholly within their control. We expect to see some alterations in breathing swallow coordination, and we do- all exacerbated by the complexity of these patients. You have to think about what got them to this point in the first place. Was it trauma? A neurological event? Was it a progressive neurological disease? Was it a pulmonary illness? Again, a sort of heterogeneous group of patients. It may be that swallowing may be more efficient when the patients receive assistance from the vent (Terzi, 2007; Garguilo et al, 2016). Both of these studies looked at patients who were actively weaning from the ventilator, spending some part of the day with ventilatory support and some part of the day without it. They looked at the swallow under both conditions and found that it looked better when patients received ventilatory assistance. If the work of breathing is all on you, then you are perhaps more likely to have some difficulty. These two studies do not say feeding every vent patient or swallowing is safe when you are on the ventilator. What these studies are saying is the theme of our entire webinar today, as breathing changes, so does swallowing. We cannot expect the swallow function always to be the same if respiration changes.
Can We Improve Breathing and Swallow Coordination?
What can we do to improve these interrelationships? What interventions are available to us? One of the things is respiratory muscle strength training. There are options for both inspiratory and expiratory muscle strength training. They target different muscles and different functions, but both have the potential to improve respiration.
Expiratory Muscle Strength Training (EMST)
The expiratory muscle strength trainer (EMST) device is a calibrated one-way valve that increases the load on the respiratory musculature during expiration. So the patient is instructed to take a deep breath and exhale through the device. As you blow through the device, you have to blow with a fair amount of effort to open the valve. The valve is calibrated and can increase the amount of pressure that is required. You can make the task continually more challenging as function improves and respiratory muscles improve. Several patient populations have a demonstrable improvement in swallow and respiratory outcomes associated with this intervention.
Outcomes
EMST has been studied in patients with ALS, and they have documented improved maximum expiratory pressures. Significantly, from a functional perspective, EMST improves cough for airway protection. That is a critical improvement for these vulnerable patients. It has also been studied in patients with multiple sclerosis, with similar outcomes, improved expository pressures, improved cough, and improved airway protection. In patients with obstructive sleep apnea, it has been demonstrated to improve respiratory muscle strength and quality of sleep. EMST has been studied in patients with a laryngectomy. It was fascinating, and you are asking yourself the same question I asked myself, how did they do this with patients with laryngectomy? They created this adaptation so patients could use the device through their stoma and exhale through the adaptation and then through the EMST device, which they could continue to increase and calibrate. van Sluis, et al. (2020) documented improved lung function, specifically maximum excretory pressures. Mainly studied in patients with Parkinson's disease, this is the group when first introduced, and several studies are looking at outcomes. van de Wetering-van Dongen et al. (2020) completed a recent systematic review looking at all of the research around EMST and Inspiratory Muscle Strength Testing (IMST) for patients with Parkinson's disease. We see some excellent outcomes in inspiratory and expiratory pressures, work of breathing, voice, and swallow improvement.
- Increased Max Inspiratory Pressure
- Improved perception of dyspnea
- Increased voice (loudness, phonation duration) EMST
- Increased tidal volume
- Increased Max Expiratory Pressure
- Improved swallow safety
It has also been studied in patients with COPD. This challenging group has documented improved respiratory muscle strength and higher expiratory pressures. Some data is looking at patients who have had strokes. Neves et al. (2014)combined IMST and EMST intervention documenting improvements in peak expiratory flow and resulting improvements in swallow function. They measured swallow function using several outcome measures in clinical swallow evals. They did not measure swallow function instrumentally (no swallow study to look at pharyngeal function), but these were clinical and patient-reported outcomes.
Compensations
The team can implement some compensatory strategies as we work with patients with compromised respiratory and swallow systems. We want them to be as well-positioned and as comfortable as possible during any meal time or swallow task. We want to make sure that they are conserving energy for swallowing. The critical thing to remember is that swallowing places demands on the respiratory system. Breathing and swallowing coordination can be challenging if you have underlying impairment in one or both of those systems. We often talk about frail, compromised, and medically complex patients, so we must consider conserving energy for this critical but potentially dangerous task of eating. We need to ensure that individuals are well-positioned, that they are comfortable, that we encourage them to take breaks when they need to, and slow the pace with smaller bites and smaller sips. When talking about breathing swallow coordination, we talked about the duration of the respiratory pause associated with the swallow. As bites and sips became more prominent, there was an earlier onset of breathing cessation and longer duration.
Let's turn that around and use it to our advantage. Smaller bites, and smaller sips, mean more time for breathing, later onset, and shorter durations of breathing cessation. By putting these compensatory strategies into place, we can improve respiration, breathing, swallow coordination, and decrease risk. The bolus hold is another compensatory strategy I encourage team members to talk to patients about. Some patients do this without our help. Their body is telling them, I cannot swallow right now. I have to hold onto this sip of water or not swallow this chew this sandwich because I need to breathe.
We also know that some of our patients are not so in tune. In my experience, this occurs a lot with patients with COPD. I think they get used to feeling breathless and are not so tuned in to that feeling of breathlessness anymore. I have sat across from many patients with COPD at snacks or meal times, and they are simply powering through and getting increasingly dyspneic. I have to say to them, Stop, slow down, take a breath. The bolus hold is a particular strategy we can teach patients to help with that. We teach them to wait before they swallow. Take that sip of water, but hold it for a second before swallowing it. Let your breathing regulate. Chew up that sandwich or that piece of cake, but hold for a second before you swallow it. Check in with your breathing. Let your breathing regulate. This straightforward strategy is helpful to patients in improving their breathing and swallowing coordination. Recently, there has been some interest in setting out to retrain breathing swallow coordination.
Retraining Outcomes in Respiratory and Swallow Coordination
- Patients with HNC (Martin-Harris et al, 2015)
- Healthy Adults (Hopkins-Rossabi et al, 2020)
- A patient with Anoxic Brain Injury (Curtis et al, 2020)
- A patient with Parkinson’s Disease (Curtis et al, 2020)
- Patients with ALS when combined with EMST (Donohue et al, 2020)
Dr. Bonnie Martin-Harris did the original work with a group of patients with head and neck cancer and impaired breathing swallow coordination. They had in place a retraining program that included illustrations, step-by-step instructions, and visual feedback teaching people to exhale a little, swallow, exhale some more, and over and over-trained that pattern. They documented instrumentally improved post-swallow and the frequency of post-swallow exhalation, which resulted in improvements in pharyngeal swallow function. Videofluoroscopic swallow studies were completed before and after the training to document changes in pharyngeal swallow physiology. Specifically, they saw improved pharyngeal valve closure, less pharyngeal residue, and less aspiration due to their retraining efforts. Since then, that protocol has been utilized with other patient populations. This retraining effort in calling people's attention to their breathing and being more mindful about their breathing swallow coordination has the potential to improve swallow function. It is a simple thing that every team member can help patients by retraining and calling attention to that healthier pattern. Let your air out, swallow, and exhale some more. That combined with the bolus hold, stop for a second, let your breathing regulate, swallow and exhale. We combine these two simple outcomes that every member of the team can be talking to the patients about. We can have a measurable improvement in breathing, swallow coordination, and, more importantly, swallow safety.
Summary
If we can improve swallow safety, we can improve lung health. Breathing and swallow coordination are critical to swallowing safety. If we are going to protect our airways, we need to ensure that our breathing swallow systems are well-coordinated and well-timed. There is also a relationship to the gastrointestinal system, so we need to consider those interrelationships between the respiratory, swallowing, and gastrointestinal systems. We need to be thinking about those interrelationships between those systems, as impairment in any of those systems can result in impairment in the other systems. Again, what happens in one part of the body affects what happens in other parts of the body. As the medical team, we want to be looking at all of these interrelationships between systems, and by putting reasonably simple interventions into place, we can document improvement, not just in swallow function but across systems.
References
References are in the course handout and can also be downloaded here
Citation
Mansolillo, A (2021). If you cannot breathe, you cannot swallow...breathing and swallow coordination in respiratory disease. Continued.com - Respiratory Therapy, Article 150. Available at www.continued.com/respiratory-therapy
