Editor’s note: This text-based course is an edited transcript of the webinar, HIV Education for Respiratory Therapists, presented by Sara Pullen, DPT, MPH.
Learning Outcomes
After this course, participants will be able to:
- Describe the basic disease process of HIV and AIDS.
- Identify the systems involved in HIV infection.
- Identify common HIV-related respiratory impairments.
Introduction
Hello everyone. I am thrilled to be back with continued. Today, we will be talking about HIV education for respiratory therapists. I am a physical therapist and see great collaboration between respiratory, physical, and occupational therapists in inpatient and some outpatient areas. We all need to have a working and current knowledge of HIV.
Appropriate Terminology: 2021
- Appropriate terminology has been defined by scientific understanding and input from the HIV community.
First, we will talk about the appropriate terminology for 2021. I put the year here because things do change. I last did this talk in 2020, and things have changed since then. Appropriate terminology has been defined by a scientific understanding and input from the HIV community. This collaboration between the scientific community and the HIV community is one of the exciting parts of HIV work and one of the reasons that I am so dedicated to it. See Figure 1 for some of the recent changes.
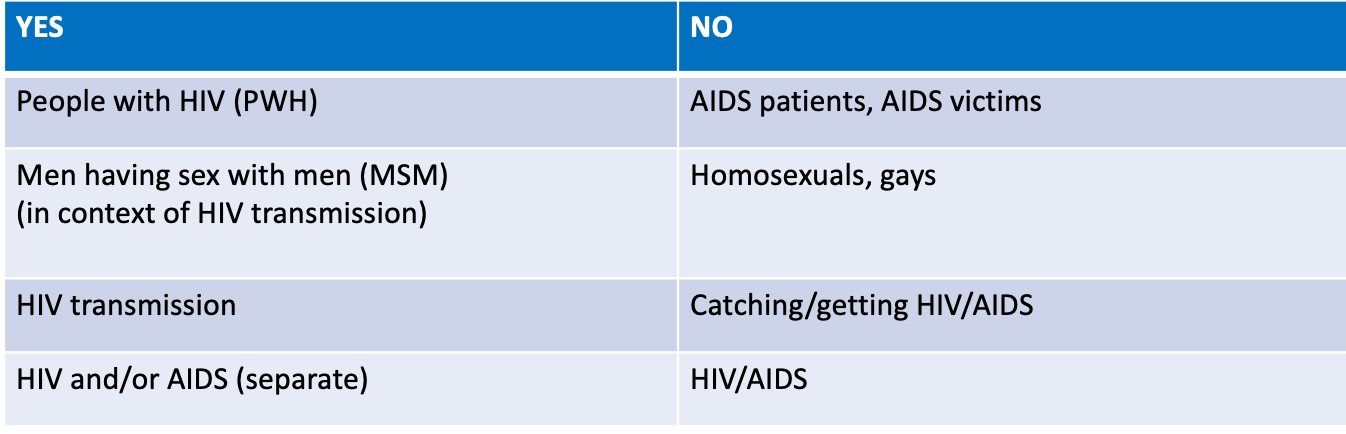
Figure 1. Appropriate terminology to use. Click to enlarge the image.
For example, we used to say HIV patients, but now we put the patient first. It is people with HIV. We also do not say AIDS patients or AIDS victims. We say men having sex with men (MSM) in the context of HIV transmission. This definition is significant because it has been referred to as homosexuals or gays in the past. It is who you are in a relationship with as opposed to what you do. Is that clear? I have plenty of patients who do not identify as gay, but they have perhaps had intimate relationships with other men, and that may be how they got HIV. We talk about it in terms of HIV transmission, not identity.
HIV transmission is the transmission of the virus. HIV and or AIDS are separate. HIV is the virus that causes AIDS, a syndrome of a full breakdown of your immune system. In the past, we said HIV/AIDS, but now those terms are separate.
HIV and AIDS Definitions
- HIV: Human Immunodeficiency Virus
- Progressive failure of the immune system allows life-threatening opportunistic illnesses (cancers, pneumocystis pneumonia (PCP), toxoplasmosis) to thrive.
- Untreated, HIV progresses to AIDS
- AIDS: Acquired Immunodeficiency Syndrome
- The immune system is severely compromised and vulnerable to opportunistic illnesses.
- CD4+ < 200 cells/mm3 (normal CD4+ 500-1600 cells/mm3)
- 1 or more opportunistic illnesses such as encephalopathy, tuberculosis, PCP, mycobacterium avium complex (MAC), lymphoma, herpes
- PWH
- People With HIV
Let's go over some basic definitions of HIV and AIDS. HIV stands for Human Immunodeficiency Virus. In a human, the immune system is deficient, caused by a virus. It is a progressive failure of the immune system that allows life-threatening opportunistic illnesses, such as certain types of cancers, pneumocystis pneumonia, PCP, which we will discuss at length later, and toxoplasmosis to thrive. In other words, your immune system is so weak that other illnesses are allowed to flourish. People die of AIDS-related symptoms or infections, not of HIV. You can live with HIV for a very long time.
AIDS is Acquired Immunodeficiency Syndrome. Your immune system is severely compromised and vulnerable to opportunistic illnesses. AIDS is measured through CD4 counts and viral load. We will talk about that in the next slide. CD4s are the helper cells that keep a person healthy. Anything less than 200 cells per mm3 is an AIDS diagnosis. An average CD4 count in a healthy individual is between 500 and 1600 cells per mm3. For example, if you are fighting a nasty virus, your CD4 cells can drop a little, and that is normal. However, anything under 200 in the context of HIV is an AIDS diagnosis. One or more opportunistic illnesses such as encephalopathy, tuberculosis, PCP pneumonia, mycobacterium avium complex MAC, lymphoma, or herpes are criteria for a diagnosis of AIDS. Lastly, the acronym PWH is for people with HIV.
- CD4+(“T-cell”): type of white blood cell that fights infection. Measured in cells/mm3
- Move throughout the body identifying and destroying viruses and bacteria
- HIV binds to and enters CD4 cells makes copies of itself gradual decline of CD4 cells and immune system
Here is a little more detail about the immunology of HIV and AIDS. You have probably heard of CD4 or T cells in the context of HIV. These are a type of white blood cell that fights infection and are measured in cells per mm3. Here is a visual in Figure 2.
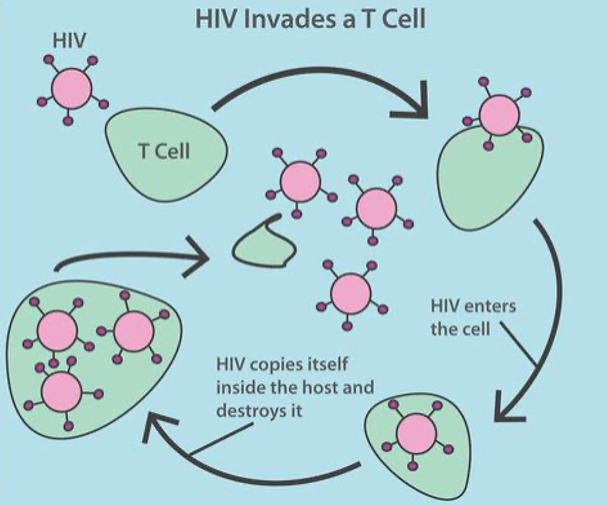
Figure 2. Infographic of T cells and HIV.
The green is a healthy T cell in the top left. The T-cells move throughout the body identifying and destroying viruses and bacteria. For all of you who have had your COVID vaccine, the second shot can pack a punch as your T cells go into overtime. HIV is in pink. You can see it looks similar to the coronavirus. You can see how HIV copies itself inside the host to destroy the CD4/T cells. Now, one HIV copy has become three. The T-cell, or the helper healthy white blood cell, is destroyed. What is left is three copies of HIV when there was just one before.
HIV Disease Process
- Viral load: measurement of HIV copies in a blood sample. Measured in copies/mL
- Viral suppression: defined as having less than 200 copies of HIV per milliliter of blood. When medication makes viral load so low that a test can’t detect it, it is called an undetectable viral load.
The viral load is a measurement of HIV copies in a blood sample measured in copies per milliliters. Viral suppression is having less than 200 copies of HIV per milliliter of blood. When medication makes the viral load so low that a test cannot detect it, it is called an undetectable viral load. In other words, you will have patients with a viral load of less than 200, meaning that the medication is working so well that it is keeping HIV at bay, and a blood test cannot detect it. They are still HIV positive but undetectable. Figure 3 shows the four transmission routes.
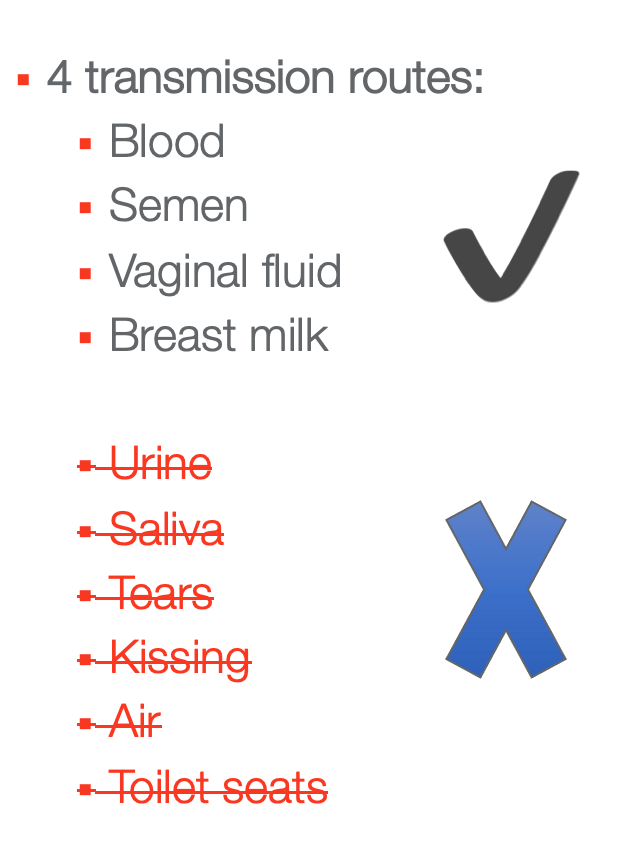
Figure 3. The four transmission routes of HIV.
The transmission routes of HIV are blood, semen, vaginal fluid, and breast milk. It can also be transmitted through pregnancy if the mother is not on HIV prophylaxis while she is pregnant. It can not be transferred through urine, saliva, tears, kissing, air, or toilet seats. There is a lot of misinformation out there.
HIV Treatment
- The pharmacologic treatment for HIV is called antiretroviral therapy (ART).
- The goal of ART is viral suppression.
- Current guidelines: Initiate ART in all adults with HIV who are willing/ready to start therapy regardless of CD4 count
- ART can't cure HIV but can help people with HIV live longer, healthier lives.
- PWH who initiate ART promptly live as long as their HIV-negative peers…IF they have access to medical care
The pharmacologic treatment for HIV is called Antiretroviral Therapy or ART. You may also see this as HAART, which is Highly Active Antiretroviral Treatment. You can see it written either way. The goal of ART is to suppress the virus to make someone's viral loads undetectable. Guidelines have changed over the years. It used to be that once someone's T-cells dropped below 200, you initiated ART. Now, guidelines are that all adults who test positive for HIV and are willing to start therapy, regardless of their CD4 count, should start right away. Early treatment is now preferred because if the patient's T-cells dropped too low, it was harder to pull them up. And, if the ART treatment starts right when the patient tests positive, it makes for greater outcomes. While ART cannot cure HIV, it can help people with HIV live longer, healthier lives. People with HIV who initiate ART promptly live as long as their HIV-negative peers if they have good access to medical care.
Science is outstanding for what it has done for people with HIV, but we all know science will not get you anywhere if you do not have access to medication. There are barriers to healthcare like a lack of transportation and stigma against people with HIV. This graphic (Figure 4) is one that I like to show. It compares the medicine regimens from the 1990s to now. In the '90s, people took up to 20 pills at different intervals throughout the day.
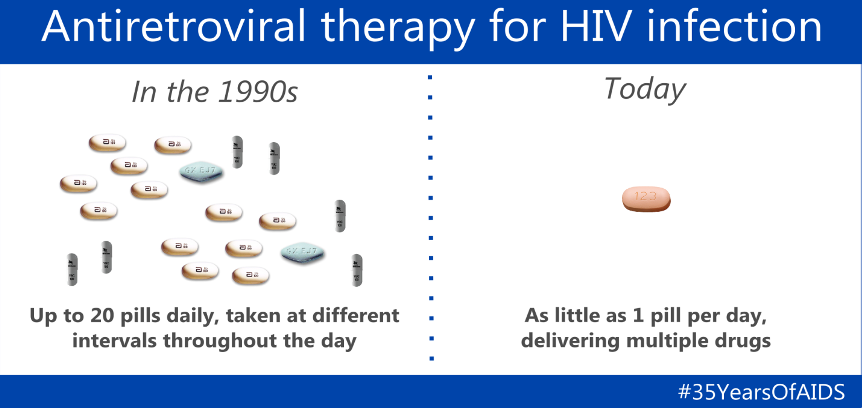
Figure 4. Antiretroviral therapy for HIV infection infographic. Click to enlarge the image.
Patients have told me about their strict regimen. "You had to take a few pills right when you woke up before you ate anything. Then, you had to wait an hour. The next round, you had to take with a full stomach. The next one had to be on an empty stomach." Right now, it is one pill per day. There are multiple drugs in one pill. This is a significant scientific advancement.
Stages of HIV Infection
- Acute HIV Infection (weeks 2-4 post-infection):
- Develop flu-like symptoms; “worst flu ever”
- Large amounts of HIV in the blood and immune system
- Greatest transmission risk
- Chronic HIV Infection:
- HIV reproduces at low levels
- People may be asymptomatic but still contagious
- With proper treatment – life expectancy = general population
An acute HIV infection is about two to four weeks post-infection. People typically say they have flu-like symptoms. There are large amounts of HIV in the blood and immune system during that time, and they are at the most significant transmission risk.
Chronic HIV infection is where HIV reproduces at low levels. People may be asymptomatic but still contagious. With proper treatment, life expectancy in the general population improves.
- AIDS – Final stage of HIV
- CD4+ count = less than 200 cells/mm3
- HIV has destroyed immune system
- The body can’t fight off opportunistic illnesses such as pneumonia and cancer --- cause of AIDS-related death
- Life expectancy without treatment = 3 years
The final stage of HIV, if it progresses to this, is when the CD4 count is less than 200 cells per mm3. HIV has destroyed the immune system, and the person's body cannot fight off opportunistic illnesses such as pneumonia and cancer, which is a significant cause of AIDS-related death. Life expectancy without treatment is three years.
You may have heard of something called U equals U. This means "undetectable equals untransmissable." Researchers have found that once you are undetectable, you cannot transmit HIV. The global HIV goal is to have everyone who has HIV become undetectable through medication to decrease transmission. What will that mean? If we get everyone the HIV medication they need, HIV transmission can hopefully stop.
HIV and AIDS: Historical Overview
My background is in physical therapy and public health. As therapists and medical providers, we need to understand the history of HIV to understand best what our patients may have gone through and are still going through. Right now, we will talk about a brief historical overview of HIV.
- 1981: 270 cases of “severe immune deficiency” among MSM- 121 of those individuals have died.
- 1982: 771 people with AIDS diagnoses. 618 reported deaths.
- 1983: 2,259 people with AIDS diagnoses. 917 reported deaths.
- 1987:
- The first mention of HIV and AIDS by the current president (Ronald Reagan)
- Cumulative known deaths from AIDS (1981-1987) 20,436

Figure 5. Early AIDS demonstration.
In 1981, 270 cases of severe immune deficiency were found among MSM (men having sex with men), and 121 of those individuals died that year. The CDC stated, "there is a strange disease among MSM." About half of those with the "severe immune deficiency" died. In 1982, just a year later, 771 people were diagnosed with AIDS, and 618 people died. In 1983, more than 2200 people had been diagnosed with HIV, and 917 had died. As you can imagine, HIV was affecting mainly MSM and IV drug users at this time. Specifically for MSM and the gay community, this was a terrifying time. The first mention of HIV and AIDS was by Ronald Reagan in 1987. By this time, more than 20,000 people had died. He joked around about it at a press conference. Figure 6 shows the first time HIV was ever mentioned in a major publication,
The New York Times on July 3rd, 1981.
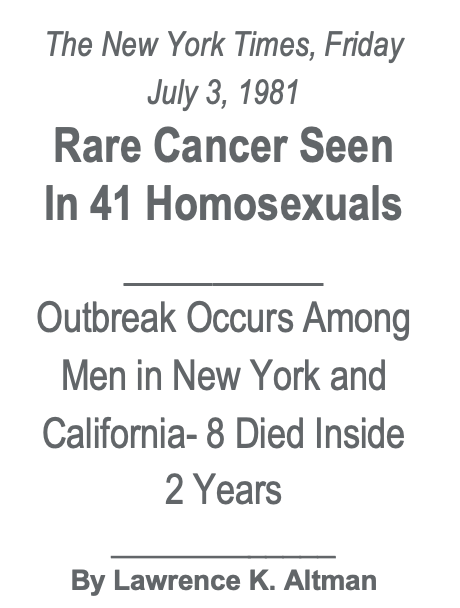
Figure 6. First time HIV noted in The New York Times.
We know it was not just cancer. We would also never say "41 homosexuals." I always get a chill looking at this headline because I know that many more than eight died within two years.
- The 1980s-1990s: Birth of grassroots organizations like ACT UP to
- Fight HIV and AIDS
- Put pressure on the government to recognize the crisis AND
- Pressure on the FDA to approve HIV drugs
The 1980s and 90s saw the birth of HIV grassroots organizations as there was no government recognition or funding for HIV. ACT UP stands for AIDS Coalition to Unleash Power. Figure 7 shown an early 80's march.
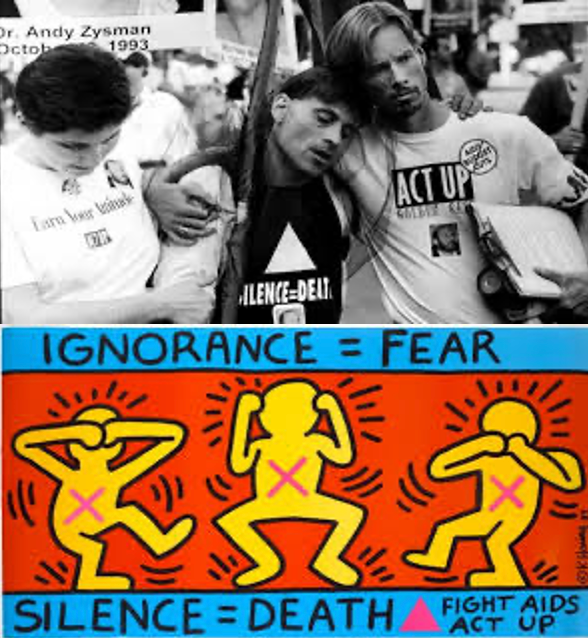
Figure 7. An early march and infographic on HIV and AIDS. (CDC via the Library of Medicine).
In this early picture, you can see the man in the middle is being held up by his partner or a friend. These demonstrations pressured the government to recognize the crisis and pressure the FDA to approve HIV drugs.
Milestones in HIV History
- 1997 – highly active antiretroviral therapy (HAART/ART) becomes the primary treatment for HIV and AIDS
- Deaths related to AIDS decreased by 47% from the year before
- March 2012:
- Life expectancy with treatment once CD4+ reaches 500 cells/mm3 EQUAL to HIV negative counterpart
- July 2012 – FDA approves Pre-exposure Prophylaxis (PrEP)
- One pill each day (same medication used to treat HIV)
- Risk of HIV >90% lower for those who take the pill consistently
In 1997, highly active antiretroviral therapy (HAART) or ART became a primary treatment for HIV. Remember, 1981 was when things started. Before this, there were 16 years of people dying in vast numbers. In 1997, deaths related to AIDS decreased by 47% from the year before. In March 2012, life expectancy with treatment (once CD4 count is 500 cells mm3)was equal to an HIV-negative counterpart.
In 2012, the FDA approved pre-exposure prophylaxis or PrEP, one pill taken each day, similar to a birth control pill. It lowered the risk of HIV by over 90% for those who took the pill consistently. They realized that treatment equals prevention. There is so much more to say about the history of HIV. If any of you have any questions, please feel free to ask or email me about it. There is a lot of incredible reading and documentaries talking about the early days of HIV.
HIV: Epidemiological Profile
Current HIV Statistics
- 36,400 new HIV infections in 2019 in the US.
- 1.7 million new infections globally
- Approximately 1 million PWH are currently in the US.
- 1 in 7 HIV+ people is unaware of their infection.
- Among 13-24-year-olds, 51% don’t know they are infected
- Highest risk communities: economically disadvantaged urban areas in the US, the South, MSM (men who have sex with other men) and African-Americans (12% of US population; 41% of HIV infections), Geriatric population (55 or older) – 26% of all HIV infections in the US.
Let's talk about the epidemiological profile of HIV. Epidemiology is the study of medicine. This data is for 2019, but we should get the 2020 data soon. There were 36,400 new HIV infections in 2019 in the US and 1.7 million new infections globally. Remember, undetectable equals untransmissable. We want to cut down on new infections, of course, but as you can see, there are approximately 1 million people with HIV currently in the US right now. One in seven HIV-positive people is unaware of their infection. It is imperative to educate people to stay safe. Among 13 to 24-year-olds, 51% do not know they are infected. This statistic stops me in my tracks. This population is probably the most sexually active (young 20s) and at the highest risk of HIV transmission. The highest risk communities also include economically disadvantaged urban areas in the US, the South, and the Southeast. I live in Atlanta, where there is a massive HIV problem. Huge infection rates are also present in New Orleans, Miami, Baton Rouge, and many Southern cities.
MSM and African-Americans make up 12% of the US population but 41% of HIV infections. We talked about barriers to care. There will be another webinar about implicit bias in healthcare that I am doing for continued.com, including discrimination in healthcare. The senior population, 55 or older, is 26% of all HIV infections in the U S. That is not new infections but an HIV infection. People who are now living longer and aging with HIV. Thus, this statistic makes sense.
Geographical Spread of HIV Diagnoses, 2020
Let's look at this geographical spread of HIV diagnoses in 2020.
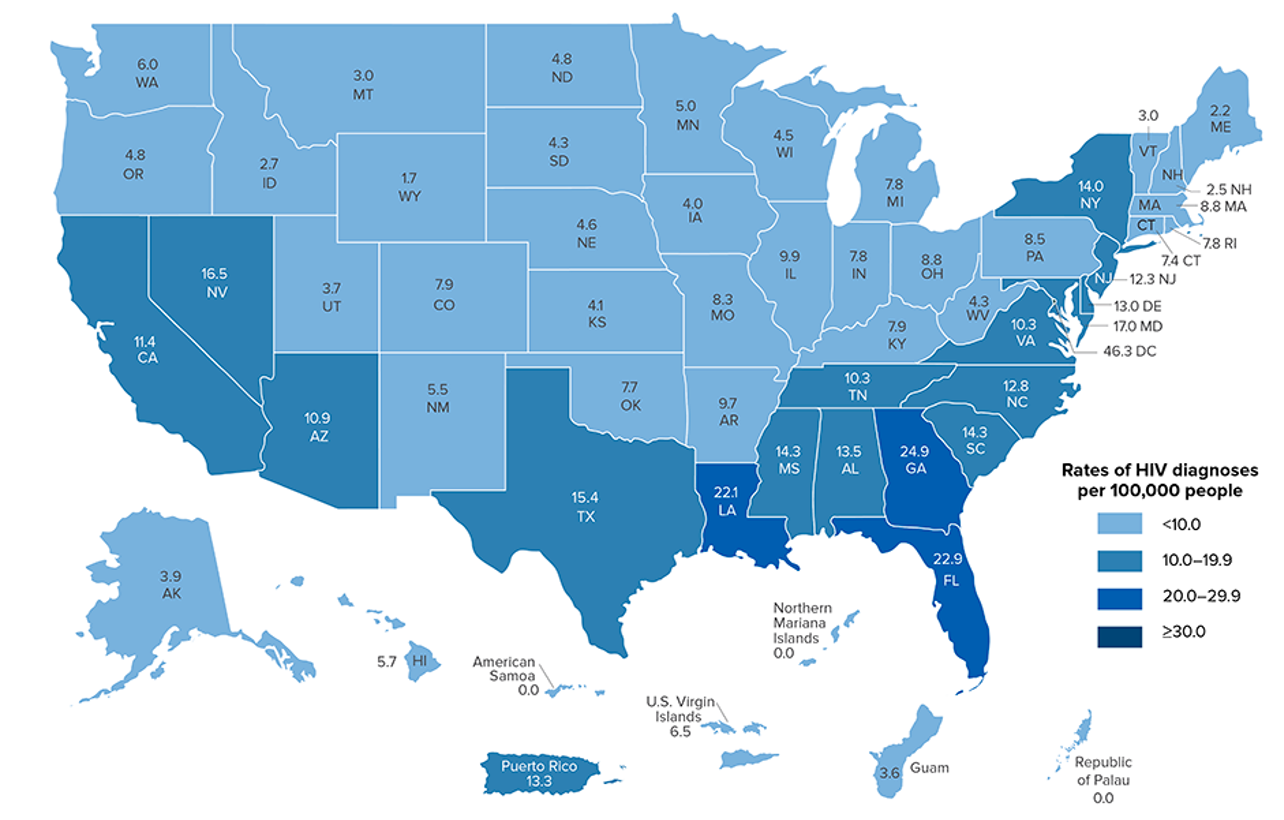
Figure 7. The geographical spread of HIV in 2020. Click to enlarge the image.
Do not get too caught up with the numbers, but you can see the darker color blue denotes the highest infection rates. The pattern shows the highest incidence of HIV throughout the South and the East coast specifically. There are many barriers to care, including poverty and HIV stigma. People talk about the "stroke belt" and "the Bible belt" of the Southeast. It is also the "HIV belt," unfortunately.
Barriers to Implementation of Effective, Long-term HIV Management
- Finances – personal income and lack of insurance
- Structural effects – housing
- Individual – substance abuse, social support
- Stigma – HIV-related, LGBTQ-related, race-related, gender-related
- Non-collaborative approach, i.e., “silo effect” of medical providers
Let's now talk about the barriers to the implementation of effective long-term HIV management. Do they have access to the following things: finances, personal income, and insurance? If people do not have insurance, that is a significant barrier as they are less likely to go to the doctor. There are payment insurance medication options for uninsured people in the US and globally for HIV. However, I also put personal income as a barrier as these individuals have to because we also have transportation and housing. There are other barriers like substance abuse and lack of social support. We also know there can be stigmas towards those with HIV, in the LGBTQ community, and about different genders and races.
A non-collaborative approach or a silo effect of medical providers can be prohibitive in terms of HIV care. For example, if someone needs to go to the dentist for a bad toothache and get to their HIV doctor, they are probably going to prioritize the dentist. They may delay picking up their meds until the next month. We need to have a collaborative approach with everything under one roof. If that is not possible, all the providers interacting with this client must think about the concept of a care team.
Multisystem Involvement in HIV and AIDS
Next, we will talk about multisystem involvement in HIV and AIDS.
Figure 8. Graphic of the systems involved in HIV and AIDS.
HIV is in the middle, surrounded by the musculoskeletal, neurological, respiratory, and psychological systems in this graphic. This graphic shows how HIV affects almost every body system, including the integumentary, for example. However, for respiratory therapists, I included these four areas.
Musculoskeletal Involvement in HIV and AIDS
- Musculoskeletal manifestations in PWH are common and sometimes are the initial presentation of the disease.
- Musculoskeletal and orthopedic complications have emerged as potential results of the disease itself and/or the ART treatment regimen.
- Example: Low bone mineral density (BMD) has been associated independently with HIV disease itself and as a direct effect of ART
- All PWH should be screened for BMD/Vitamin D supplementation.
Which comes first, the chicken or the egg? Some things are caused by HIV and other manifestations by the medication. Back in the 80s and 90s, before there was medication available, there was muscle wasting in those with AIDS. Now, this is a little different as there are complications related to the medicines as well. Musculoskeletal and orthopedic complications have emerged as potential results of the disease and/or the ART treatment regimen. An example is that low bone mineral density has been associated independently with HIV and directly due to ART. All people with HIV should be screened for low bone mineral density (BMD) and Vitamin D supplementation.
Where do respiratory therapists play a part? Frailty is a significant danger for people with HIV, and it happens earlier than it would maybe in someone without HIV due to the medication. If you have a frail individual (maybe just in their 50s or 60s), you need to make sure to ask them if they are on vitamin D supplementation.
- Most commonly seen MSK impairments are myalgia, arthralgia, low back pain, osteoporosis, avascular necrosis of the femoral head.
- PWH have a higher prevalence of fractures compared to HIV(-) peers
- HIV affects bone remodeling bone fragility
- ART may also affect bone metabolism
The most commonly seen musculoskeletal impairments are myalgia, arthralgia, joint pain, low back pain, osteoporosis, and avascular necrosis of the femoral head. People with HIV have a higher prevalence of fractures as compared to HIV-negative peers. Often, they get hip and rib fractures due to falls. As a respiratory therapist, you might work with someone with a rib fracture. The disease itself does not typically affect an individual's lungs unless later in the condition. As a respiratory therapist, you need to know the risk of fractures and how the HIV and ART treatment affects bone remodeling, fragility, and bone metabolism.
Exercise and HIV
- Large systematic reviews indicate that continuous or interval aerobic exercise or a combination of progressive resistive and aerobic exercise is safe and potentially beneficial for medically stable adults living with HIV.
- In PWH, exercise was associated with improvements in cardiopulmonary measures, strength, weight, body composition, quality of life, and psychological status.
Weight training and aerobic exercise are safe and potentially beneficial for medically stable adults living with HIV. People with HIV exercise outcomes showed improved cardiopulmonary measures, strength, weight, body composition, quality of life, and psychological status.
- Dufour et al. (2013): adults with HIV who self-report exercising are approximately half as likely to show neurocognitive impairments in comparison to those who do not exercise
- Exercise in PWH has NOT been associated with adverse immunological/virological outcomes.
- Stable CD4+ count and viral load
Here is an excellent article by Dufour and colleagues. They said that adults with HIV who self-report exercising are approximately half as likely to show neurocognitive impairments compared to those who do not exercise. This is across the board. We all know that exercise is vital for physical strength and neurological function. Activity in people with HIV is not associated with adverse immunological or virological outcomes, and there are stable CD4 counts and viral loads. This is excellent news as we used to think that people with HIV should not exercise as it stressed the immune system and negatively affected CD4 counts and viral loads. The great news is that that has not been shown at all. We want to ensure our clients are getting in both cardio and aerobic exercise for the lungs, of course, with their primary doctor's approval.
Neurological Involvement in HIV and AIDS
- HIV-associated neurocognitive disorders (HAND) cluster of milder symptoms
- Viral infections Cytomegalovirus, progressive multifocal leukoencephalopathy (PML), rapidly progressing and often terminal
- Fungal/parasitic infections toxoplasmosis
- Neuropathy
- Vascular myelopathy most common in untreated HIV
- CNS Lymphomas
- Neurosyphilis
- AIDS Dementia Complex
HIV-associated neurocognitive disorders or HAND is a cluster of milder symptoms. Viral infections include cytomegalovirus, or CMV, and progressive multifocal leukoencephalopathy, or PML. These are rapidly progressing infections and often terminal. Fungal or parasitic infections like toxoplasmosis are other issues. Neuropathy is common, and vascular myelopathy is the most common in untreated HIV (people not on ART). Central nervous system lymphomas, neurosyphilis, and the AIDS dementia complex are other neurological problems.
- The virus can settle in the brain (CNS) as early as four months after infection.
- When HIV+ people are off treatment, the CNS can provide an additional reservoir for the virus, possibly leading to neurological damage/events.
- The combination of HIV and ART can result in an increased incidence of neuropathy/neurological impairments.
HIV can settle in the brain and the central nervous system as early as four months after initial infection. In some older HIV documentaries, you can see many individuals with AIDS, dementia, and brain dysfunction with untreated HIV. It was very tragic and sad for the patients and their loved ones who saw this deterioration. When HIV-positive people are off treatment, the CNS can provide an additional reservoir for the virus leading to neurological damage and events. Remember that graphic about HIV making its way around the body. The combination of HIV and ART can result in an increased incidence of neuropathy and neurological impairments.
- Encephalopathy
- May be associated with untreated or “treatment interrupted” HIV AIDS
- Stroke
- HIV infection can result in stroke via several mechanisms - opportunistic infection, vasculopathy, cardioembolism, and coagulopathy.
- Average age of stroke in PWH = 49-51 (Burke et al.), compared to the general population (65)
Encephalopathy may be associated with untreated or treatment interrupted HIV or AIDS. Encephalopathy is swelling in the brain and can lead to vast cognitive, neurological effects. We used to call interrupted treatment a "drug holiday." People who go off their medications for whatever reasons (lack of money, transportation) can lead to adverse effects. For example, HIV infection can result in stroke via several mechanisms like opportunistic infection, vasculopathy, cardioembolism, and coagulopathy. Burke and colleagues showed that the average age of stroke in people with HIV was 49 to 51 years old. This is much earlier than the general population, in which the average is 65.
Mental Health
- Increased prevalence of mental health disorders in PLH, especially depression, Alzheimer’s, dementia, PTSD
- Primary care providers are ideally positioned to manage some mental health issues and/or mental health referrals.
- HIV proteins alter the response to stressors and cortisol production
- Exercise has emerged as a significant protective factor for HIV-related cognitive decline
- MSM (men who have sex with men) who survived the 1990s with HIV likely have lost 9/10 of their immediate social group
There is an increased prevalence of mental health disorders in people living with HIV, especially depression, Alzheimer's, and PTSD. Primary care providers and all therapists are ideally positioned to manage some mental health issues and are mental health referrals. HIV proteins themselves alter the response to stressors and cortisol production. Exercise has emerged as a significant protective factor for HIV-related cognitive decline, as I said earlier.
A study probably five years ago stated that MSM, who survived the 1990s with HIV, have lost nine out of 10 of their immediate social group to AIDS. There is an incredible amount of trauma that they have survived, and understandably, some have PTSD. HIV proteins can alter the response to stressors and cortisol, and HIV itself is a stressor. Stressors can lead to depression. People living with HIV, no matter how long they have had it, worry that they will die.
Cardiopulmonary Involvement in HIV and AIDS
- Cardiopulmonary
- Long-term cardiac outcomes of HIV and/or ART can include
- Noninfectious cardiovascular complications, including cardiomegaly, pericarditis, myocarditis
- The lung is a frequent target organ for disorders associated with HIV infection, such as HIV-related pulmonary arterial hypertension
- Long-term cardiac outcomes of HIV and/or ART can include
Long-term cardiac outcomes of HIV and or ART can include noninfectious cardiovascular complications, including cardiomegaly, pericarditis, and myocarditis. The lung is a frequent target organ for disorders associated with HIV infection, such as HIV-related pulmonary arterial hypertension.
The Role of the Respiratory Therapist in the Care of PWH
I hope I have given you a good background on the virology of what HIV is doing in the body. I have also given you the epidemiology of HIV and its history. I have shared the statistics about where it is in the world and the country. Lastly, I have overviewed how it affects the different systems, which all in turn, of course, affect the respiratory system.
Respiratory System and HIV
- ART has drastically improved the lifespan and quality of life for PWH
- However, PWH report increased respiratory symptoms, including chronic cough and breathlessness, than their HIV-negative counterparts (Brown et al., 2016)
- Respiratory morbidities were historically linked to AIDS-related deaths, especially pre-ART
- We will review several respiratory comorbidities related to HIV to assist in clinical understanding
Antiretroviral therapy has drastically improved the lifespan in the quality of life for people with HIV. However, people with HIV report increased respiratory symptoms, including chronic cough and breathlessness, than their HIV-negative counterparts. Even though people with HIV have an improved lifespan and quality of life, people with HIV are more likely to report respiratory symptoms.
Respiratory morbidities were historically linked to AIDS-related deaths, especially pre-ART. I always wonder how respiratory therapy had been involved with HIV care from the beginning how impactful that could have been in terms of quality of life and survivability. Respiratory therapists still have an essential role.
Now, we will review several respiratory comorbidities related to HIV to assist in the clinical understanding of HIV with respiratory therapy.
Pneumocystis Pneumonia
- PCP is caused by a ubiquitous fungus.
- Symptoms: nonproductive cough, dyspnea, fever may be present, hypoxemia. The most common lung exam finding is inspiratory crackles, but the lung exam may be normal.
- Treatment: Typically Antibiotics
- Prognosis: mortality rate 30-50%
- PCP was – and still is – a common predictor of death once HIV has progressed to AIDS
Pneumocystis pneumonia is a primary ubiquitous fungus. I saw that terminology in an article and had to write it because it is descriptive and evocative. It is a fungus that is everywhere. If your immune system is in good shape and you are not immunocompromised, you are fine. We all have this fungus somewhere in our bodies. Symptoms of pneumocystis pneumonia are a nonproductive cough, dyspnea, fever, and hypoxemia. The most common lung exam finding is inspiratory crackles, but the lung exam may be normal. See Figure 9 for an example of this.
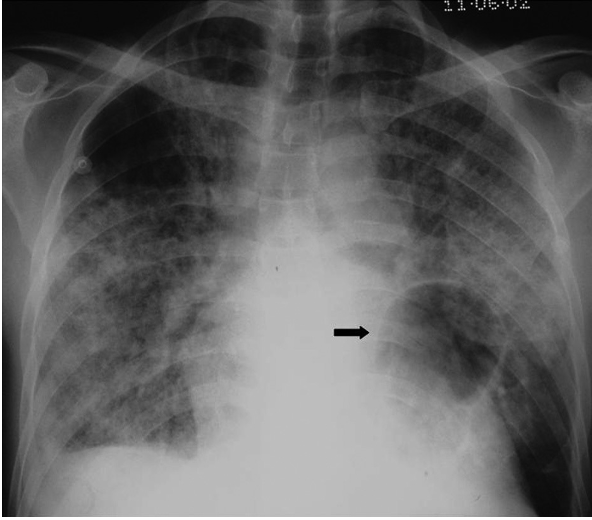
Figure 9. PCP - “ground glass” opacities.
Treatment for PCP is typically antibiotics. I usually say in front of all my "treatments" because I am not a physician or a pulmonologist. I cannot recommend anything particular. The mortality rate is still 30 to 50% which is very high. If someone has HIV that has progressed to AIDS and gets PCP, the mortality rate is pretty high. It was and still is a common predictor of death once HIV has progressed to AIDS. Before ART, PCP was the most common death.
Cytomegalovirus
- Cytomegalovirus (CMV) is a common virus: over half of adults in the US have it in their bodies by age 40
- Symptoms: nonproductive cough, dyspnea, fever, malaise.
- Can cause blindness
- Lung exam: may demonstrate crackles, but may be normal
- CMV pneumonitis is rarely found in isolation; it typically presents in the setting of disseminated disease
- CMV among PWH: most at risk CD4<100, CMV-retinitis, weakness, diarrhea, pneumonia, encephalopathy
- Prognosis: no cure but can be controlled with antifungals and ART
Cytomegalovirus (CMV) is also a common virus. Over half of adults in the US have it in their bodies by age 40. It is a virus that floats around the atmosphere. You may have it in your body but never know if your immune system is robust and not compromised. Symptoms of cytomegalovirus are a nonproductive cough, dyspnea, fever, and malaise. It can also cause blindness. A lung exam may demonstrate crackle, but it may show up as normal. It is rarely found in isolation. For example, someone would have HIV, progress to AIDS, and also have CMV. Among people with HIV, the most at risk for CMV are people with CD4 counts below 100. Remember, below 200 is an AIDS diagnosis. CMV retinitis, weakness, diarrhea, pneumonia, and encephalopathy are other issues. There is no cure, but it is controlled with antifungals and ART.
Tuberculosis
- HIV-TB co-infection is a global health priority
- Mycobacterium Tuberculosis bacteria are airborne
- Co-diagnosis of HIV and TB = AIDS-defining
- TB may present at any level of CD4 count
- Symptoms:
- CD4 counts >200: similar presentation to an HIV- negative person (fever, chills, night sweats, weight loss, productive cough, and occasional hemoptysis)
- Severely immunocompromised persons with advanced HIV: lymphadenopathy, central nervous system involvement)
- Treatment: isolation, drug combination
You all know about tuberculosis and have probably treated people with TB in your careers. HIV-TB co-infection is a global health priority. When I was researching and preparing this talk, I went down a rabbit hole looking at articles about HIV and TB. It is not controlled in nations and communities that are underserved and under-resourced. It is a priority because once HIV and TB both take up residence in your body, the prognosis is poor. A co-diagnosis of HIV and TB is AIDS-defining. In other words, if you have this, TB is one of the things that will define AIDS along with that CD4 count. And, TB can be present with any level of CD4 count. Symptoms include CD4 counts below 200. The symptoms with TB are similar to an HIV-negative person, including fever, chills, night sweats, weight loss, productive cough, and occasional hemoptysis. Severely immunocompromised people with advanced HIV can experience lymphadenopathy and central nervous system involvement. Due to TB being infectious and airborne, treatment is isolation and different drug combinations.
Mycobacterium Avium Complex
- Mycobacterium avium complex (MAC) – a group of bacteria related to TB
- Almost everyone has them in their body from food, water, soil
- PWH with low CD4 (<50) – most at risk
- Opportunistic infection
- Primary Symptoms: fever, weight loss, anorexia, hepatosplenomegaly, lymphadenopathy, abdominal pain, chronic diarrhea
- Disseminated MAC: MAC spreads all over the body and can lead to systemic infections, hepatitis, pneumonia
- Treatment: antibiotics
Mycobacterium avium complex or MAC is a group of bacteria related to TB. Almost everyone has them in their body from food, water, and soil. People with HIV with low CD4 lower than 50 are most at risk. It is an opportunistic infection. Primary symptoms are fever, weight loss, anorexia, loss of appetite, hepatosplenomegaly, lymphadenopathy, abdominal pain, and chronic diarrhea. Disseminated MAC is when MAC spreads all over the body. This is a bacteria and can lead to systemic infections, hepatitis, and pneumonia. MAC treatment includes antibiotics.
Immune Reconstitution Inflammatory Syndrome (IRIS)
- IRIS develops in the context of recovery of CD4 cell counts following the initiation of ART
- Typically develops within the first few weeks after starting ART
- Most commonly seen in conjunction with such infections as TB, PCP, MAC, and Cryptococcus, more rarely with Kaposi sarcoma
- Symptoms:
- Fevers, lymphadenopathy, meningeal symptoms, and pulmonary infiltrates
- Risk factors:
- Low CD4 count prior to initiation of ART
- There are no definitive diagnostic criteria for IRIS- diagnosis of exclusion.
- Treatment with corticosteroids can be life-saving in severe cases
- ART should be continued during IRIS if at all possible
Immune reconstitution inflammatory syndrome (IRIS) develops in the context of recovery of CD4 counts following ART initiation. You are diagnosed with HIV, you take ART just like you are supposed to, and the CD4 counts start to climb back up where they are supposed to be. Within the first few weeks of starting ART, you can get IRIS if you also have an infection such as TB, PCP, MAC, cryptococcus, or Kaposi sarcoma, which we will talk about in a second. The symptoms are fever, lymphadenopathy, meningeal signs, and pulmonary infiltrates. It is dire. The risk factors are low CD4 count before starting ART. There are no definitive diagnostic criteria for IRIS diagnosis, but rather it is a diagnosis of exclusion. In other words, you cannot point your finger and say that is IRIS. However, if you have all these other things, that can lead to a diagnosis. Treatment consists of corticosteroids and can be life-saving in severe cases. ART should be continued during IRIS if it is at all possible.
Malignancy: Kaposi Sarcoma
- Kaposi sarcoma (KS):
- Malignancy that was common in HIV patients prior to ART
- One of the markers of AIDS in the early days of the epidemic
- The primary risk factor is low CD4 count (particular <50, very rare with CD4 >200), and the incidence is higher in MSM
- Up to 15% of PWH with KS may have isolated pulmonary disease
- Presenting symptoms of pulmonary KS include dyspnea, cough, and fever; hemoptysis may be present
Kaposi sarcoma is something that you may recognize from early pictures of people with HIV and AIDS. It looks like a port wine spot. It could come like these smaller clusters or kind of big red splotches (Figure 10).

Figure 10. Kaposi sarcoma presentation on the arm.
It is a malignancy common in HIV patients before ART and one of the markers of AIDS in the early days of the epidemic. People would realize they had HIV when they saw those on their skin. The primary risk factor is a low CD4 count, particularly less than 50, and it is scarce with CD4 over 200. There is also a higher incidence of MSM. We are not sure why it affects this population more, but it could be how HIV is transmitted. Up to 15 percent of people with HIV and KS have isolated pulmonary disease and pulmonary symptoms like dyspnea, cough, and fever. Hemoptysis, or bloody cough, also may be present.
In Summary of Opportunistic Infections
- Often no cure, so ART initiation and ART fidelity are key
- If a patient with HIV presents with any persistent respiratory complaints, REFER immediately to a primary physician
There is often no cure for opportunistic infections. ART initiation and fidelity are fundamental. If a patient with HIV presents with persistent respiratory complaints, they need to be referred immediately to their primary physician. Right now, I work exclusively with people with HIV in an HIV clinic. I am highly honored to be doing this work. Before this, I saw patients with these symptoms and thought it sounded like HIV or AIDS. Once I referred them, the diagnosis was typically positive.
HIV as a Prevalent Disease
- Greater prevalence calls for an increasing role for rehabilitation in the continuum of care for PWH
- Respiratory therapists may treat PWH of all ages and in various clinical settings
- For example:
- Pediatric patient in the NICU
- Geriatric patient in a rehab setting
- For example:
- HIV and AIDS may be simply listed as a comorbidity, or the patient may have an HIV-related impairment as the primary diagnosis of referral
- Asthma with HIV only listed in PMH
- AIDS-related PCP
HIV is a prevalent disease. It is everywhere, and there is an increasing role for rehabilitation with this population. Respiratory therapists may treat people with HIV of all ages in various clinical settings, from the NICU to a senior rehab setting. HIV and AIDS may be listed as a comorbidity, or the patient may have an HIV-related impairment as a primary referral diagnosis. For example, they may have asthma and HIV or AIDS-related pneumocystis pneumonia listed in their history.
HIV as a Chronic Disease
- In the era of ART, people can increasingly live longer with HIV, delay or avoid opportunistic infections, and live with HIV as a chronic health condition.
- However…research shows that quality of life decreases with age, mostly related to physical decline, lower levels of independence, and poorer emotional wellbeing
- Chronic inflammation due to long-term HIV infection
- Autoimmune dysfunction, cardiovascular disease, neurocognitive disease, osteoporosis/frailty, liver disease, kidney disease, and some cancers
HIV is also chronic as people can live longer with HIV with ART treatment. ART can help clients to avoid opportunistic infections and live with HIV as a chronic health condition. However, research shows that quality of life decreases with age, mostly related to physical decline, with lower independence and poor emotional wellbeing. There can be chronic inflammation, autoimmune dysfunction, cardiovascular, neurocognitive, osteoporosis, liver, kidney, cancer, and respiratory issues with a long-term HIV infection.
- Effects from the disease itself and its pharmacological treatment can cause long-term and acute health complications.
- However - less than 1/3 of deaths among PLH are attributed to HIV-related causes
- Increasing role of “care team” in the long-term management of HIV and non-HIV-related impairments
- Increasing role of rehabilitation, mental health
- Collaborative effort between disciplines and AIDS Service Organizations for comprehensive care
The effects of the disease and ART can cause long-term and acute health complications. However, less than a third of deaths among people living with HIV are attributed to HIV-related causes. There is an increasing role of the care team in long-term management. There is also a growing role in the rehabilitation and mental health management of the disease and not just pharmacologic and infectious areas. We must have a collaborative effort between disciplines and AIDS service organizations for comprehensive care. We need to know what is going on in the HIV community to learn from that and supplement any areas of need.
HIV and Aging
- The number of PWH who are aged 50 years and older has tripled since 2000
- Several HIV-related factors could possibly prevent healthy aging: inflammatory processes, cardiovascular disease, frailty, social isolation
- Remember…It is estimated that MSM who survived the 1980s with HIV had 9/10 of their peers die of AIDS
The number of people with HIV who are age 50 and older has tripled since 2000. Part of it is that people with HIV are living longer. Also, people are getting newly infected at age 50 and older. One reason is that people 50 or older do not necessarily use birth control as pregnancy is not a concern. Several HIV-related factors can also prevent healthy aging like the inflammatory process, cardiovascular disease, frailty, and social isolation. Remember, it is estimated that MSM with HIV who survived the 1980s had nine out of 10 of their peers die of HIV. If that happened to someone in their 20s and now they are in their 60s, they will need plenty of support.
Long-term HIV Management
- The long-term care of people living with HIV is increasingly focused on chronic disease management and health promotion.
- Mental health; drug and alcohol use; sexual and reproductive health; cardiovascular, renal, liver, and bone disease; malignancies; and prevention
- The majority of people living with HIV can be managed in the general practice setting, with specialist support where appropriate.
The long-term care of people with HIV is increasingly focused on chronic disease management, health promotion, mental health, drug and alcohol management, sexual and reproductive health, cardiovascular, liver, and bone health, et cetera. We should focus on prevention in addition to treatment. Most people with HIV can be managed in a general practice setting with specialist support where appropriate instead of the big AIDS clinics in the past.
“How Do I Ask About It?”
- A client may not wish to disclose HIV status or, they may refer to it as “the virus,” “when I got infected,” etc.
- DO: Ask about medications: which ones, any side effects, any trouble with medication compliance, if they are followed regularly by an infectious disease doctor, if they know their most recent CD4 count
- Why is this important?
- DO NOT: Ask how they were infected
- DO: Ask about medications: which ones, any side effects, any trouble with medication compliance, if they are followed regularly by an infectious disease doctor, if they know their most recent CD4 count
How do I ask about it? You may choose not to ask as you do not need to, or the client may not want to disclose their HIV status. You do need to ask about medications and any side effects. You also want to know their medication compliance. If they are followed regularly by a doctor, they should know their recent CD4 count. As we know, going off of ART can be fatal and have vast effects on someone's health and mortality.
Here are some questions you can ask. "What medications are you on?" "Any trouble with those?" "Are you taking them every day?" "Are you followed regularly by an infectious disease doctor or primary care?" "Do you know your most recent CD4 count?" This is all you need to know. Do not ask how they were infected. It is incredible how many of my patients have said that people like their dentist or a nurse have asked how they got HIV. This is a no-no as it is not anyone's business.
Social Support
- This is especially important for PWH. It can affect both mental and physical health, including medication compliance.
- Family support?
- Friends ?– "Do you have people you feel like you can call if you are sad/having a hard time/in the middle of the night?"
- Partner/spouse?
- Who have they disclosed their status to?
- Living situation (stable housing or not, safety concerns)
- Be sensitive to stigma that client may have experienced – including from family, work, friends (yes, even in 2021)
Social support is critical for people with HIV. It can affect both mental and physical health, including medication compliance. "Do you have people you feel like you can call if you are having a sad or hard time in the middle of the night?" I always ask this question. Who have they disclosed their status to? Everyone should have at least one person who knows they have HIV. Do they have a good living situation? Be sensitive to the stigma the client may have experienced from family, work, and friends. Sadly even in 2021, there is still HIV-related stigma.
Physical Exam
- Generally, no different than for non-PWH, except if the patient has HIV and AIDS-specific diagnosis
- Universal precautions for blood-borne pathogens
- Reminder: how is HIV spread?
- Fellow staff may need a friendly reminder about HIV transmission
A physical exam is no different than for people without HIV except that there is an HIV or AIDS-specific diagnosis. If someone has PCP pneumonia from AIDS, of course, that is going to be a different exam than someone who comes off for an outpatient asthma appointment.
What are the universal precautions? How is HIV spread? It is not spread through casual contact, patient-provider contact, sputum, or saliva. Fellow staff may need a friendly reminder about HIV transmission.
Future Directions
- Multi-disciplinary collaboration to ensure that needs of this diverse population are met.
- Palliative care model
- HIV management in primary care
- HIV Prevention and screening at all life stages
- PrEP
- Screening older patients for sexual health-related risks
- National study: adults > age 50 at risk for HIV are 80% less likely to be tested for HIV than younger people
We need to have multi-disciplinary collaboration to ensure the needs of this diverse patient population are met. In a palliative care model, everyone comes together to improve the client's quality of life. HIV management (PrEP), primary care, and prevention screening are essential at all ages. It is also important to screen older patients for sexual health-related risks. People over age 50 are 80% less likely to be tested for HIV than younger people even though they are high risk.
In Summary
- As PWH live longer, fuller lives, they will inevitably present to rehabilitation therapy for both HIV-related and non-HIV-related issues.
- It is key to know the patient’s
- HIV status: viral load, recent CD4 count
- Antiretroviral regimen and adherence
- Social support networks
- Despite vast advances in treatment, stigma and isolation are still major issues facing PWH.
- As rehabilitation medicine practitioners, we must be both clinicians and advocates for this unique patient population.
As people with HIV live longer, inevitably, they will present to rehab therapy for both HIV and non-HIV-related issues. It is vital to know the patient's HIV status, viral load, CD4 count, antiretroviral regimen inherence, and social support and networks. Despite vast advances in treatments, stigma and isolation are still major issues for people with HIV. As rehabilitation practitioners, we must both be clinicians and advocates of this unique patient population.
This concludes our HIV education for respiratory therapists. If you have any questions or comments or information that you wish I had covered about respiratory therapy and HIV, I am always open to learning and questions. Please feel free to contact me at sara.pullen@emory.edu. Thank you so much for coming today and for being interested in this topic. Additionally, thank you for all of your work in the past year with coronavirus. My heart and thanks go out to each of you as you have borne the brunt of this past year. Thank you all for your work and compassion.
References
http://www.avert.org/stages-hiv-infection.htm
http://aidsinfo.nih.gov/education-materials/fact-sheets/19/45/hiv-aids--the-basics
Brown J, Roy A, Harris R, Filson S, Johnson M, Abubakar I, Lipman M. Respiratory symptoms in people living with HIV and the effect of antiretroviral therapy: a systematic review and meta-analysis. Thorax. 2017 Apr;72(4):355-366. doi: 10.1136/thoraxjnl-2016-208657. Epub 2016 Oct 24. PMID: 27965402; PMCID: PMC5520276.
Citation
Pullen, S. (2021). HIV education for respiratory therapists. Continued - Respiratory Therapy, Article 113. Available at www.continued.com/respiratory-therapy
