Introduction
I wanted to talk to you a little bit today about high flow nasal oxygen. There are a lot of terms that are tossed around. From my perspective, when working with students, I know there can be some confusion as some terms mean the same thing. For example, we have similar terms: high-flow nasal cannula, high-flow nasal oxygen, high-flow nasal therapy, heated high-flow nasal oxygen, heated high-flow nasal cannula. I have experience using these in acute care, the ICU, and the NICU.
What is High Flow Oxygen?
- High flow oxygen systems include those that can supply a flow that meets or exceed the patient’s peak inspiratory flow.
- These systems use air-entrainment or blending systems to create precise Fi02.
For oxygen devices, there are high-flow, low-flow, and reservoir systems. Many times, the terms high-flow and high liter flow all get mixed. When by definition, they are quite different. A high-flow oxygen therapy system includes those that supply a flow that meets or exceeds the patient's inspiratory flow demand. Many of these terms are used synonymously when they are very different. You might have learned the magic box or some other formula to calculate the total flow of an oxygen device. When we are talking about total flow, that is how we get a true high-flow device.
Although they can get to higher liter flows, traditional oxygen delivery devices are often diluted by room air, so the patient is breathing oxygen and room air. The FiO2 then becomes variable. These devices cannot meet the definition of true high-flow because they do not bring any additional flow from another source to increase the total flow of the device. Systems that do meet this are high-flow air entrainment and blending systems. An entrainment system, for example, would be a venturi mask. A blending system would be just like it sounds-- a machine that has a blender built inside of it so it can create a precise FiO2.
Who Needs High Flow Oxygen?
- Typically high flow oxygen is reserved for severe oxygenation issues.
- Patients with high inspiratory flow demands
- Patients who need help in C02 removal
- Can be used in all patient populations
What kind of patients need this type of therapy? Some patients potentially have severe oxygenation issues but also need to breathe spontaneously. However, they need to be able to protect their airway. They can do mild to moderate work of breathing but not severe work of breathing. Usually, by the time they have reached that level of muscle fatigue, it is too late in the game to try high-flow nasal oxygen.
Those with high inspiratory flow demand are another group that needs high flow oxygen. This is one of those terms that is not tossed around in everyday language when talking about taking care of patients. Terms that may be a little more familiar to you would be large tidal volumes, short inspiratory times, and increased minute ventilation. They have increased work breathing or an increased drive to breathe. Those are the type of patients you will see with increased or high inspiratory flow demands.
An aspect of high-flow nasal oxygen therapy is that it is also capable of CO2 removal. Sometimes, this device gets intertwined with non-invasive therapy, but the way CO2 is removed using this type of therapy is slightly different. We will discuss this a little bit later.
A considerable benefit to high-flow nasal oxygen and nasal cannular therapy is that it has been designed for all patient populations. Depending on the device or the model you are using, which I will also discuss in just a little bit, some therapies will work great for the neonatal population to the adult population and everything in between.
One question that I am frequently asked when teaching this to students or discussing high flow with someone who is not well versed in using it is, "Why cannot I just put a non-rebreather on this patient?" If we are looking at giving them higher FiO2, the non-rebreather mask goes up to 15 liters. However, in these cases, we need to provide them with more FiO2. It has been tossed around about starting with a non-rebreather mask first, but there are instances where you should and instances where you should not.
Alternative Types of Masks/Devices
Non-Rebreather Masks
- Non-rebreather masks are capable of higher liter flows.
- They are not high flow (total flow) devices.
- Fi02 is variable
Here is a quick review of the non-rebreather mask. It runs up to 15 liters a minute. It does have a high liter flow, but it is not a high flow total flow device.

Figure 1. Non-rebreather mask.
When we look at total flow, we have to have some kind of entrainment of air/oxygen mixture. This is where we are increasing the total output that the device is capable of delivering. The non-rebreather does not do that. The non-rebreather can provide approximately up to 70% FiO2, but again it is variable. The reasons why it is variable depends on the way the patient is breathing. It also depends on how well the mask fits the patient's face. You could see two patients put on the same settings of a non-rebreather, but if you were capable of measuring the FiO2 being delivered, it could be pretty different even if they were both on a 15-liter non-rebreather mask.
There are quite a few variabilities in the non-rebreather. This is not saying it is not a suitable device or should not be used, but it is in a different category. It is sometimes intertwined with high flow oxygen when people talk about delivering higher FiO2s and higher liter flows.
Venturi Masks
- Venturi masks/ AEM masks are true high flow (total flow) devices.
- The air - entrainment increases the total output of flow.
- Deliverable FiO2 is lower but generally more precise.
There is the venturi mask (Figure 2).

Figure 2. Venturi mask.
The venturi mask is sometimes referred to as the air entrainment mask. This is a true high-flow device. Remember, it can meet or exceed the patient's inspiratory flow because it mixes the air and oxygen to increase a total flow and a greater output. The deliverable FiO2 is precise, and the color-coded devices give a specific FiO2. A downside to these is that most devices, or at least the most familiar ones, max out at about 50%. As there are patients that need more than 50% FiO2, what do we do in these situations? We need to give them a total flow device to meet that inspiratory demand. They need more than 50% FiO2, thus creating the need for high-flow nasal cannular devices.
High (Liter) Flow Cannula
- High (liter) flow cannulas deliver oxygen at greater flow rates than a standard nasal cannula.
- Most max out at a flow of 15 lpm and require humidification.
- In most situations, this is not a high flow device and the Fi02 is variable.
This is another one that I have seen out there that can be confusing. This particular device is referred to as a high flow nasal cannula, as seen in the two examples in Figure 3.

Figure 3. Examples high flow cannulas.
It is not only a high flow nasal cannula, but it is a high liter float nasal cannula. If you are familiar with using this particular cannula, it will go up to approximately 15 liters. I used this cannula several years ago when I first started practicing, and then it disappeared. It has resurfaced again in recent times. This cannula is designed like a traditional cannula, but it does not max out at that 6-8 liters that a conventional nasal cannula will. This one will go up to 15 liters per minute, but it does require humidification. You can see the refillable humidifier device in the right picture. A downside to this is there is a potential for cross-contamination when you use refillable devices. If this device works well for your patient, that is great.
A higher FiO2 will meet some client's oxygen needs. Again, this is still a variable FiO2 variable device, and it is not a total flow device. It is a high liter flow device because the patient will still be able to breathe room air around the prongs, around their nares, and through their open mouth. The amount of oxygen that they are taking in will be diluted, and the FiO2 will be variable.
When These Are Not Enough
- High inspiratory flow
- High tidal volume
- Fast rate of breathing
- Large minute ventilation
- Short inspiratory time
There are some instances when the devices I have just talked about are not enough. What is going to be the right approach? How do you know when you should start with a high-flow nasal cannula versus some of the other devices that I just mentioned? It is not that those devices are harmful. Except for the air entrainment or the venturi mask, all of the others are genuinely low-flow devices. There are instances where we would start a patient on a high flow nasal cannula instead of some low flow devices. They include someone who does have a high inspiratory flow, a high or a large tidal volume, or an individual with a fast breathing rate, so the respiratory rate is elevated. Another way of describing that is large minute ventilation with a short or a quick inspiratory time. These specific conditions make using a high flow nasal cannula more favorable to meet the patient's inspiratory needs.
High Flow Nasal Cannula (HFNC) Review
- High flow nasal cannulas offer flow rates up to 60 lpm with precise FiO2 concentrations up to 100%.
- Humidification is often incorporated into the device setup.
- Indications are continually evolving with numerous benefits in both adult and pediatric populations.
- New devices are being developed frequently to meet the demand for this type of device.
Here is a quick review of high flow nasal cannula therapy before breaking down some of the devices and looking in a little more detail. In general, high flow nasal therapy or high flow nasal cannulas offer flow rates up to 60 liters per minute while offering a precise FiO2. Most of the time, those concentrations will go up to a hundred percent. One of the tricks that I teach my students is the rule of four, where one liter is approximately 24% oxygen, two liters is about 28, 3 liters is 32, and so on. High flow nasal cannulas have a blender system already incorporated into the device. The air and oxygen are blended manually. I can offer a precise FiO2 that is no longer dependent on liter flow with this device. For example, I can deliver 50% oxygen at 40 liters. I can offer 100% oxygen at five liters in a NICU setting. Oxygen concentration and amount of liters are no longer dependent upon each other in a high flow nasal cannula, differentiating it from some of the other oxygen therapy systems.
Humidification is often incorporated in the high-flow nasal cannula setup. I will talk to you in a minute about why that is so important. The indications of HFNC use are continually evolving, with numerous benefits in pediatric and adult populations. There are new devices that are constantly and frequently being developed. High-flow nasal cannula therapy is gaining widespread use in the treatment of COVID, especially in the early-onset trying to avoid intubation. There are several benefits that I will break down and talk about in just a few minutes.
The Role of Humidity
- All humidity is NOT equal!
- Heated humidity is required for all HFNC.
- The flow rates generated by HFNC can cause the isothermic saturation boundary to shift distally.
- This can lead to further complications.
The reason why humidity is so essential in HFNC is that all moisture is not equal. Some of the traditional devices, like the ones I just showed you, are not heated. If we are using a high-flow nasal cannular therapy, it has to have heated humidity.
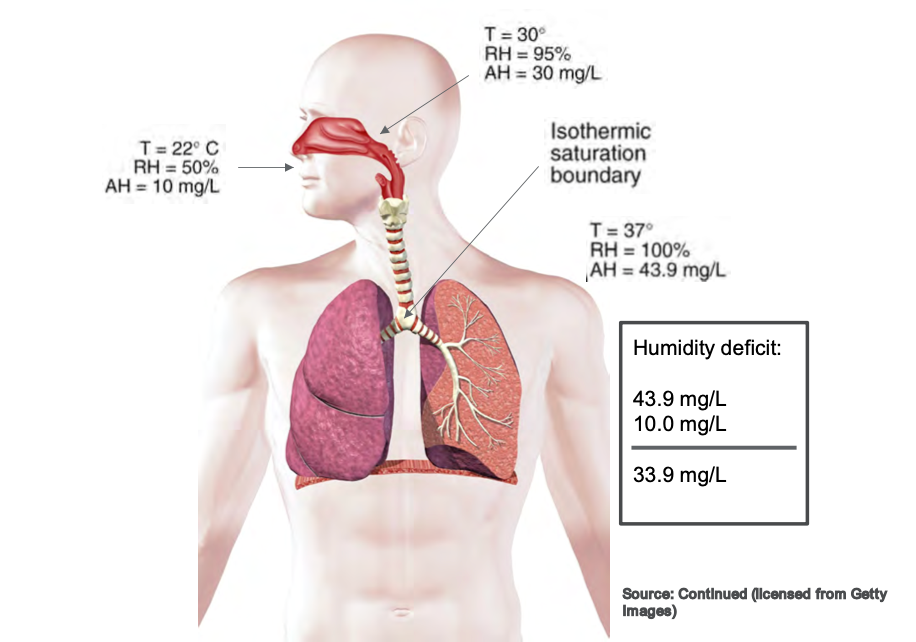
Isothermic Saturation Boundary
The flow rates generated by a high flow nasal cannula can cause the isothermic saturation boundary to shift. When that occurs, we can cause all sorts of complications in the airway, and the isothermic saturation boundaries shifts. This can cause mucosal trauma, dried secretions, and impaired mucociliary escalator function. It results in a myriad of complications that we do not want in the upper airway because we want our patients to cough, clear their airways, and maintain normal function of the upper airway. Whenever we use high flow therapy, those flows are too significant for the regular operation of the isothermic saturation boundary to overcome. This is why we have to add heat so that we can help balance that out. Figure 4 shows a picture of the isothermal saturation boundary.
Figure 4. Illustration of the isothermic saturation boundary. Click to enlarge the image.
The primary function of the nose is to warm and humidify inspired gas. If the temperature was approximately 22 degrees Celsius, the relative humidity would be about 50%. If we increase the temperature by the time it reaches the oropharynx at the back of the throat, we are looking at a higher temperature of about 30 degrees Celsius and relative humidity of 95%. Movement from the nose to the oropharynx causes a significant increase in temperature and relative humidity. By the time it reaches the isothermic saturation boundary around the carina before it enters the lung, we want it to be full relative humidity at a hundred percent saturated and our average body temperature of 37 degrees Celsius. That is a whole lot of words to say that the nose warms the inspired air typically. When we put a nasal cannula in someone's nose, we are potentially disrupting that normal function.
When we use heated high flow therapy, we are generating flows that far exceed the patient's normal inspiratory flow, and the nose cannot warm those gases fast enough. It is imperative that we use heated humidity for high flow therapy because we do not want to negatively impact the humidification and the normal function of the upper airway itself.
HFNC: How It Works
- HFNC improves oxygenation by:
- Washing CO2 from end expiration
- Reducing dead space
- Providing positive end-expiratory pressure
- Optimal PEEP levels are directly linked to a regular breathing pattern and a closed mouth
(Dres and Demoule, 2017)
It improves oxygenation in these three ways. First, it washes out the CO2 from the end expiration. Every time a person exhales, they have end-expiratory gas that remains in the upper airway. Whenever they exhale, there is a little bit of CO2 that is left in that end expiration. Whenever we use higher flows, we wash out CO2 to have a more oxygen-rich environment when the patient goes to inspire, and there are fewer traces of those end-expiratory gases. Ultimately, this increases the oxygen that is being delivered to the patient.
We can also reduce dead space. Dead space is anywhere that oxygen exchange cannot occur. Oxygen exchange cannot happen in any upper airways like the nose, sinuses, or trachea. Oxygen exchange cannot occur until deep in the lungs, where it crosses over in the alveoli and membranes there. If we can reduce dead space by generating flows that get the oxygen down to where it can be absorbed, not only are we going to improve oxygenation, but chances are we will also improve the work of breathing. The patient is not having to work as hard to overcome their normal anatomical dead space to get that oxygen down into their lungs where it needs to be.
Over the last few years, there have been varying studies about whether high flow therapy provides PEEP or positive end-expiratory pressure. Dres and Demoule (2017) reported that optimal PEEP levels were directly linked to a regular breathing pattern and a closed mouth. This means that if the patient has a normal rate and pattern, they can get up to approximately seven centimeters of pressure. However, we know that that is not always the case. Sometimes our patients are talking, eating, or taking medications, and their mouth is open. We cannot get them to keep their mouth closed at all times. So yes, PEEP is possible.
We know that PEEP increases the alveoli's surface area, creating lung expansion and improving the potential for oxygenation. However, it is a catch-22 when we look at it as a non-invasive support device. I will talk about that in a little bit more detail later. Another interesting aspect I found about this study is that they also reported not only positive end-expiratory pressure but also for every 10 liters of the flow used on a high flow therapy device, there was an increase in central airway pressures. This was a .69 increase if the patient's mouth was closed and a .35 increase for the same user if the patient's mouth was open. These are not huge increases, but if you have a patient with high main airway pressures, you need to be mindful of this.
Looking at the CO2 and nasal washout, this is an excellent illustration in Figure 5 that Moller et al. (2017) saw in their study.
Figure 5. CO2 and nasal washout using tracer gases. Click here to enlarge the image.
They had the patient inhale a tracer gas to see a visual of the nasal washout. Looking at the first picture, the gas is inhaled so that it can be seen. In the middle, you can see that the end-exhalation gases remain in the nasal and upper airways in the control subject. However, with the individual on high flow therapy (45 liters per minute), you can see that those gases are almost non-existent in the nasal airway. There is a drastic improvement in oxygenation because we have washed out CO2 and primed that nasal cavity for higher oxygen concentrations. This is why it is particularly effective in individuals who have hypoxemic acute respiratory failure.
Types of HFNC
Let's now look at the different types of high-flow nasal cannulas. I am just going to talk about a few. I do not claim to be inclusive of all devices that are on the market. I spoke with a few therapists that I know, and these are the main ones that everyone seems to be currently using.
Optiflow
- Provides flowrates from 2-60 lpm
- With Airvo 2, this device can be used during transport
- Several interfaces available to increase patient comfort and compliance
The Optiflow is one of them. This version is made by Fisher & Paykel, and this device uses flow rates of 2-60 liters per minute. It has several patient interfaces to fit the needs of various patient populations. A benefit to using this device is that it has compatibility with the Airvo 2. The Airvo 2 is a humidification integration device that has a built-in humidification and flow generator. It generates its flow, making it easier to set up and transport per the feedback I got from many therapists. Figure 6 shows an example of this.

Figure 6. Example of an HFNC device with a humidification integration device.
It also improves the accessibility of this device. In one older hospital where I worked, some floors did not have multiple oxygen outlets, or some of them only had oxygen outlets and no air outlets. I know this may still be the case in some areas. Ideally, all hospitals should have multiple oxygen and air wall outlets for multiple device access. The Optiflow has its flow generator, which helps with accessibility. Figure 7 shows several interfaces available to increase patient comfort and compliance.

Figure 7. Examples of Optiflow patient interfaces.
These can range in sizes from infants to adults. Adult models come in small, medium, and large, and there are infant and pediatric sizes and trach attachments. If you get on the Fisher & Paykel website and look up their Optiflow, there was also a mask interface. I could not find much information or any patient testimonials, but there is an aerosol-type mask that will also work with the Optiflow. I asked around, but I do not know anyone who has used it.
Vapotherm
- Flow rates of 1-40 lpm
- Can be integrated into EMR and nurse call systems.
- HeliOx compatible for 80/20 mixture
- Multiple cannula sizes are available (premature, infant, pediatric, adult, adult large).
Vapotherm is the HFNC that I am well-versed in as I used it quite frequently. This particular device has flow rates of 1-40 liters per minute, so a little bit lower than the Optiflow (Figure 8).

Figure 8. Vapotherm on a rolling stand.
The newer models can be integrated into the EMR, and the nurse call light systems. This is something new that I found out when preparing for this lecture. If they were to run out of humidification in the past, you would have to be in pretty close proximity to hear it alarming. There was also a concern that these devices might overheat. It is a gravity-feed liquid system, but it just has to be watched and replaced from time to time to ensure that the humidifier continues to function the way it is supposed to. Now, this system can be integrated into the existing call light, which is a huge benefit to this device. It is also compatible with HeliOx with an 80/20 mixture. I searched, and I did not find many patient studies about the use of a high flow HeliOx therapy, but it could be because it is brand new. This is an area that I will also continue to look at to see how it is integrated into practice.
The Vapotherm also offers quite a few interfaces, even more so than the Optiflow (Figure 9).
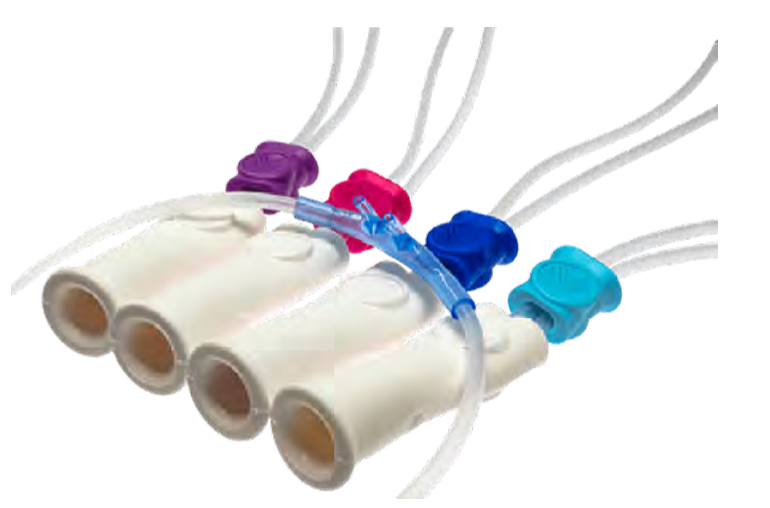
Figure 9. Various size interfaces of the Vapotherm.
There are cannulas for preemies, infants, children, adults, and even adults large. Eight different interfaces are available on the market through the Vapotherm site. There are various settings, as shown in Figure 10.
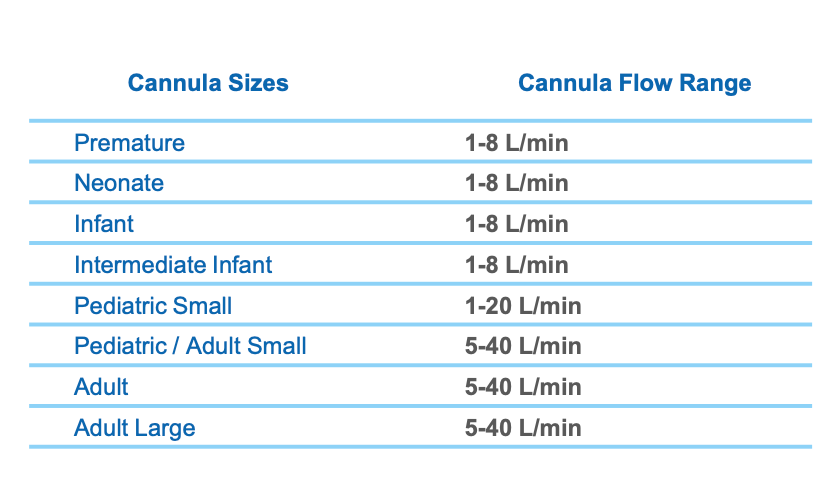
Figure 10. Cannula sizes and flow range chart for various ages.
The premature style ranges from 1-8 liters per minute; neonate, infant, and intermediate infant all have that same liter flow range. The spacing and the size of the prongs help you to determine how best to fit a client. The pediatric setting is a flow of 1-20 liters. Once we get up to the adult small, can crossover from pediatric, the flow range is 5-40 liters per minute.
Why are there so many different sizes? Everyone's nose is different, like the spacing of their nares and how far apart they are. I know this was my experience. It is essential, especially in the NICU with the preemies, that it fits correctly. Even in the adult setting, there was a lot of variability in nose structures. As we know, compliance is dependent on patient comfort.
HFNC Convertible Ventilators
- Some ventilator models have HFNC capabilities integrated into the vent.
- ▪ Hamilton C-6, G-5, C3, C1, and T1
- ▪ Offers more complex features in addition to
- HFNC
A few ventilators on the market today are convertible to high-flow nasal cannular devices (Figure 11).

Figure 11. Ventilators that convert to HFNC.
In particular, the Hamilton models (C-6, G-5, C3, C1, and T1) can be converted. I have not used any of these. I know at Midwest State, where I teach, we have the Hamilton G-5. This is a ventilator with widespread use in many of my clinical affiliates. It offers a lot of additional monitoring. High-flow nasal cannulas provide a built-in SpO2 monitor. The Hamilton is not only a ventilator that can convert to a high-flow, but it also has SpO2 capabilities.
The flow rates of these devices are up to 60 liters per minute. The G-5, in particular, offers integration with the Aerogen nebulizer. You can also incorporate the nebulizer capabilities with this device to be delivered through the high flow nasal cannula. The interfaces that are available with this device include adult, pediatric, and neonatal varieties and trach attachments.
These are all of the high flow nasal cannula studies that I could find.
HFNC Vs. NIV
- HFNC does generate PEEP however it varies across patients.
- When compared to traditional oxygen masks and NIV, the outcomes were similar.
- However, when initiated early in patients with hypoxemic ARF intubation rates were significantly lower.
(Dres and Demoule, 2017)
How do you know when to use high-flow nasal cannula therapy versus non-invasive? Or, when should you have started non-invasive instead of high flow? We do offer the PEEP and expansion, so there are some of the same similarities here. How do you know which one is best? Unfortunately, there is not a hard, fast rule. In my opinion, they offer some similar features, but it is like comparing apples and oranges.
The high flow nasal therapy does offer PEEP. However, it varies across patients and interfaces. As mentioned, depending on if your patient has their mouth open or closed, their PEEP will vary all day long. Whereas, with NIV, you can set the PEEP and inspiratory/expiratory pressure depending on the modes you are using. This is pretty much what you will get with the high flow if they are opening their mouth, talking, awake, sleeping, etc.
Compared to traditional oxygen masks and non-invasive ventilation, HFNC had very similar outcomes in a study by Dres and Demoule (2017). I want to discuss that a little bit. They evaluated patients who were admitted primarily for pneumonia. Once the patients were admitted, they were assigned to traditional oxygen masks, NIV, or HFNC. Initially, the study found that the outcomes were similar in almost half of the subjects. Across all three categories, subjects failed and had to be intubated. Most of the time, high flow nasal cannula therapy failure is marked by the need for intubation, not the progression to non-invasive. This is where I think a lot of therapists ask the question, "If high-flow nasal cannula therapy fails, do I go to non-invasive, or do I go to intubation?" All of the studies that I found marked high-flow nasal cannula therapy failure as the movement to intubation, not the progression to non-invasive. For individuals who presented with severe hypoxemic acute respiratory failure and used high flow nasal cannula therapy, their failure rate was significantly lower. So, when you look at the patients who not only had pneumonia but also had a hypoxemic acute respiratory failure with frequent or early-onset initiation of high-flow nasal cannula therapy, they did have a favorable outcome. Their intubation rate was lower compared to individuals who were put on non-invasive or traditional oxygen masks.
Recommendations for Clinical Practice
- Assessment of Need: Determined by measurement of inadequate oxygen tensions and/or saturation, and the presence of clinical indicators.
- AARC Clinical Practice Guidelines for Oxygen Therapy
- Adults: Acute hypoxemic respiratory failure,
- Postoperative support, pre- intubation,
- post-extubation respiratory failure, DNR/DNI
- Pediatric: Asthma, bronchiolitis, pneumonia
- Neonatal: RDS and stabilization of preterm infant, post-extubation
Recommendations for clinical practice were somewhat challenging to find. I think many therapists would agree that there are no cut-and-dry recommendations for high flow nasal cannula therapy. There are significant variations in how it is used, when it should be initiated, how to determine its failing, when it should be started, when it is appropriate, early initiation versus late initiation, and how to determine if it is failing? I began to look at some studies to see any trends in clinical practice or types of appropriate patients.
The AARC has clinical practice guidelines for oxygen therapy. For one, it has to be determined by a measurement of inadequate oxygen tensions and/or saturation, so either blood gases or monitoring in the presence of a clinical indicator. It also looks at the work of increased breathing, hypoxemia, dusky appearance, and all of those things where a client needs oxygen.
High flow nasal cannula therapy was indicated in acute hypoxemic respiratory failure, in postoperative support, and in particular, postoperative support of cardiothoracic surgeries, which I will discuss in the next slide.
In pre-intubation, setting up a whole high flow system is not the norm while preparing to intubate someone. Still, it was found that high flow nasal therapy was successful or adequate in providing oxygenation to an individual who was already on it but clinically needed to be intubated. So, there are instances in which it will meet the oxygenation needs while preparing for intubation
Post-extubation respiratory failure is another indication. This is for an individual who has been successfully or relatively successfully weaned from a ventilator but still needs a little bit of support. This is a great example where high-flow could offer some assistance for PEEP to ease and assist with work of breathing while also offering appropriate FiO2s. This is where we are waiting for them to regain their strength and control and the ability to breathe on their own.
Additionally, there are instances in which it is appropriate for our "do not resuscitate" and "do not intubate" clients. If you have a patient who is adamant that they do not want to be intubated, but they are presenting with some oxygenation needs, many times you will find that families and patients are more accepting of the high-flow nasal cannula as it looks similar to a traditional nasal cannula. Although we know that it is not and has additional functions, it is frequently more accepted.
In pediatric patients, individuals who are suffering from an asthma exacerbation may benefit from HFNC treatment. This supports them with increased flow and oxygenation through the higher FiO2 capabilities. This is similarly true for bronchiolitis and pneumonia. It is a necessary treatment in the neonatal setting, particularly with respiratory distress syndrome and the stabilization of preterm infants. High flow treatment is different from C-PAP as the neonate can begin to eat and take oral food when using it. If they were on C-PAP and positive pressure devices, they would have to wait and have different forms of nutrition. High-flow nasal cannular therapy, if the patient tolerates it, is a favorable option. And for post-extubation, it offers the babies additional support versus just putting them on a traditional low-flow nasal cannula.
Early Intervention
- Early intervention shows promising results in HFNC therapy
- When compared to conventional low-flow devices, HFNC was associated with reduced escalation of therapy/ length of stay.
(Wang, Huang, Ni, & Liang, 2020)
There is an argument that early intervention is vital. It states that the earlier you get clients on high-flow nasal cannula therapy, the more favorable the outcomes are going to be. In this particular study, they compared conventional low-flow devices to a high-flow nasal cannula. They found that HFNC was associated with reduced escalation of therapy, and ultimately, a decreased length of stay. They also evaluated the initiation of high flow nasal cannular therapy following extubation of these cardiothoracic surgical patients. Most of them I believe had a CABG. High-flow nasal cannular therapy met their oxygenation needs and got them off the ventilator. It got them back to using their own muscle strength, but it also eased their work of breathing. After the thoracic area is opened in these types of procedures, they are usually very painful. If we can offer that little bit of PEEP to help keep their oxygen levels up and provide lung expansion, this will promote breathing and reduce the risk of developing postoperative pneumonia. So, it was very favorable in that setting. It not only reduced the need to escalate to either non-invasive or reintubation, but it also helped with decreasing their overall length of stay in the hospital and ICU.
Too Good To Be True?
- Absolute clinical practice guidelines are still very limited.
- HFNC failure was associated with the delayed application of NIV support or intubation.
- Another concern is that HFNC is repeatedly being initiated directly from low-flow devices with no documentation of other O2 device attempts.
(Kim et al., 2020)
On the other hand, there are arguments out there that claim that high-flow nasal cannula therapy is too good to be true. Their belief is that there are no clear guidelines for when we should take it off the HFNC or when we should determine that they have failed and need either non-invasive support or intubation. There is the argument that early initiation is how patients are more successful. The other argument is that signs of failure are not being recognized quickly enough in patients on high-flow nasal cannula. We are delaying therapy that could be more beneficial increasing the potential for complications and increased lengths of stay. There are both sides of the story here.
This study compared the failure rates of high flow nasal cannula and found that the cases were widely varied. I think all therapists would agree there is no set path for certain signs and symptoms. Again, there are not those hard, fast rules for HFNC use, but there are criteria for low-flow. So, they looked at the particular group of patients and found that there was such varied use that it was hard to even compare them. However, one finding from this study is that high-flow is often initiated with no documentation of any other O2 attempts. There is also no use of reservoir or low-flow devices used. Instead, clients are immediately put on high-flow. Again, there was not a lot of information on that. Another conclusion that they found was that failure was associated with who prescribed the high-flow. For example, there was a higher failure rate among residents versus pulmonologists. Thus, if residents were the ones prescribing the high-flow therapy, there was a higher failure rate. I do not know why this is other than to say I would hope that pulmonologists would be better at recommending equipment as that is their specialty. It also could be dependent upon the patients and environment.
Spo2/FIO2: Breathing Frequency
- ROX Index- indicator for HFNC failure
- ROX= Spo2/FIO2
RR
- It has been used to predict failure at 2, 6, and 12 hrs.
- Success is determined when the ROX index stays above 4.88.
(Roca et al., 2019)
There is a model for determining high flow nasal cannula failure called the ROX Index. I found a few studies that used this as a clinical indicator for outcomes. For more information, I would encourage you to review the F&P Optiflow website. They have a section that is called Flow Matters. This study is linked on the site, and this calculator is linked at the bottom of that page. This calculation tells us the patient's SpO2 as compared to their FiO2 in relation to what their breathing frequency is or respiratory rate. We plug these numbers into the above formula, and we get what is called a ROX Index. For example, a patient has a SpO2 of 95, their FiO2 is 21% on room air, and have a normal respiratory rate of 12. Using this formula, their ROX Index is probably going to be somewhere in the 30s. That would be a normal index. This particular calculation is evaluated upon initiation at 2 hours, at six hours, and then at 12 hours of use. If we see a steady decline in those numbers, that indicates that the high flow therapy is essentially failing. If at any point we get below a 4.88, we should start looking at intubation. Actually, the scale that I found was anything greater than 4.88, there is little risk for intubation; a score between 3.85 to 4.87 is an increased risk for intubation; and at 2.85 to 3.84, we should monitor them in the ICU setting if at all possible as they have a highly increased risk of intubation. If their ROX score is less than 2.85, we should consider intubation at that time and not wait. And, if you get less than a 2.85 at two hours, you would consider it a failure and not continue to measure for 6 hours.
Role of RT
- Progression and Weaning
- The success of HFNC is undeniable although the devices have limitations
- Specific to patient condition and underlying cause
- Monitoring is Key
What is our role? What is the role of the respiratory therapist when working with high-flow? There are lots of areas that we need to be involved in, and I understand that in current times we are pulled in every direction. I feel like that is all of healthcare in general, but there are some areas that we should specifically focus on in order to determine and best optimize the use of high-flow nasal cannula therapy.
Should you wean FiO2 first, or should you wean flow first? I really do like that ROX indicator score. It has not been validated widespread, but there I have seen studies on its use as early as 2019, a couple in 2020, and one in 2021. I think it has promising outcomes when using it to assess the progression of high-flow nasal cannular therapy and knowing when it has been successful or when it has failed. In my experience, I always weaned flow first and then FiO2 taking a stair-step approach. For instance, if they could tolerate less flow and did not have an increase in work of breathing, then I would drop the FiO2. I would look for the same signs and symptoms and continue to stair-step this down until we could wean them off of it.
It is very important that the respiratory therapist is involved in the weaning of high flow because no one understands oxygen therapy quite as well. Sure, there are great allied health professionals, nurses, and doctors that understand what an oxygen device does, but no one is going to understand all the treatments options like low-flow, high flow, reservoir, cannula, trach, humidity, etc.
The success of high-flow nasal cannula therapy has shown promise in the treatment of COVID. If we can avoid intubation in those patients while meeting their oxygen needs, that is the best for this patient population.
It has limitations. If the patient begins to have an increased work of breathing or muscle fatigue, high flow nasal cannula therapy is not going to be enough. We need to recognize the signs and symptoms so that we are able to intervene appropriately. Their oxygen saturation may still be 95 or even 90, but if we see that they are retracting and using accessory muscle, we know that it is time to make a change.
There may be underlying causes that we have to consider. The most successful application of high flow nasal cannula therapy is for acute respiratory failure associated with hypoxemia. We also have to consider what other comorbidities and conditions they have. As I said in the beginning, we need to know if they spontaneously breathing and are able to protect their airway. We also need to know if they have been huffing and puffing for a long time, and they are ready to give out because they are so tired. We need to continuously monitor these patients, which I know is easier said than done because we can be pulled in so many directions.
Again, we are so well versed in oxygen therapy that we know the limitations, indications, and different parts and pieces of this equipment. We need to hold our ground and make our presence known when it comes to the use of these types of devices.
In conclusion, I wanted to let you know is that the ROX Index is available in an app and can be downloaded through Google Play or Apple Stores. I also want to encourage you to review the existing literature on high flow nasal cannulas. I found tons of literature just in the year 2020 especially for the treatment of COVID. I could find the arguments for both sides of whether it was successful or not. I particularly one study on the Fisher & Paykel for Optiflow website that is included here.
I want to thank you for your time today. I hope that you learned something new and interesting about the use of high flow nasal cannula therapy.
References
Available in the handout.
Citation
Fino, J. (2021). High flow nasal oxygen: What's what!. Continued.com - Respiratory Therapy, Article 106. Available at www.continued.com/respiratory-therapy