Editor’s note: This text-based course is an edited transcript of the webinar, Current Guidelines in Asthma Management Across all Age Groups, presented by Nancy A. Nathenson, RRT.
Learning Outcomes
After this course, participants will be able to:
- Recognize the age group and severity classifications of asthma.
- Identify the criteria for determining asthma severity.
- Describe the key components of the Asthma Action Plan.
- List the most common types of patient non-compliance
Much of the information for this course comes from the Allergy and Asthma Network, the National Institute of Health, and the CDC, so there are a lot of resources available to you that are listed at the end of this presentation.
Why I Became a Respiratory Therapist
I became a respiratory therapist because of my mother, Margaret. My mom had asthma when she was a child, and over a number of years up until when she was a teen, she had no asthma symptoms. She went to the doctor and the doctor said, "Why, Margie, you outgrew your asthma because you rode your bike so much." We all know that asthma is a lifelong disease and that really was not the case. My father was in the military and was transferred to Yokohama Air Base in Japan. When my parents and I were living there, my mother picked up what the locals called Yokohama asthma, which was from the volcanic ash that was in the atmosphere. This triggered her allergic asthma. She suffered through that for many years, all of my childhood and into my adulthood.
What is Asthma?
Asthma is a lung disease caused by an increased reaction of airways to stimuli, and it can be life-threatening. Of the individuals that die every day, a third of them all were diagnosed with only a mild form of the disease. That is important when we talk to our patients. Just because they have mild asthma, they should know that there is still a threat that they could suffer a severe asthma event and even death.
Asthma is a chronic, lifelong disease, with symptoms that may come and go. It is often related to allergies. About 60% of asthma is what is called allergic asthma. There are two other types of asthma, nocturnal and exercise-induced asthma. Those are the main three types of asthma.
What Happens During an Asthma Attack?
When I talk to people in the community, I always say it is like a triple threat. There is airway inflammation where the airway lining becomes red, swollen, and narrow. Then you have bronchoconstriction, where the muscles that encircle the airway tighten up and spasm, further constricting the airway. There is also airway obstruction. As the airway tightens and narrows, it can be very difficult to get air in and out of the lungs, especially out. Airway hyperresponsiveness occurs when the muscles that encircle the airway respond more vigorously and quickly to smaller amounts of allergens and irritants. In addition, secretions (mucus production) within the airway lining increase during an asthma attack.
What Causes Asthma?
There are multiple causes of asthma. There are genetic and environmental factors that contribute to asthma. If the individual has a family history of allergies or asthma, that can tend to make them more likely to have asthma. If both parents suffer from asthma, there is more likelihood that a child could have asthma. If there is just one parent, that likelihood decreases a little bit.
Mothers smoking and exposure to secondhand smoke or air pollution while pregnant can cause asthma, in addition to early childhood exposure to secondhand smoke, air pollution, and indoor allergies. Damage to lung development from a premature birth or early childhood respiratory diseases that are chronic and reoccurring can cause asthma. For adults, exposure to industrial dust or chemicals in the workplace contributes to asthma. This is what we sometimes call occupational asthma.
Asthma Statistics
The Bad News
The bad news is about 24 million Americans have asthma, and about 270 million people worldwide. Those are the patients that we know have asthma and do not include those not yet diagnosed. About 6 million of those diagnosed Americans are children. Asthma is a leading chronic disease in children and has been for some time. Boys are more likely to get asthma than girls. African-Americans, Hispanics, and Non-Hispanics are more adversely affected than Caucasians with asthma. Ten per million individuals die each day from asthma.
Health Disparities
There are health disparities as well with asthma, and with many chronic diseases. The factors that lead to asthma disparities and other diseases are access to care, income, such as lower socioeconomic conditions, environmental allergens and irritants, education inequality, and language and cultural differences.
The Good News
The good news is there are better diagnoses and management. The big picture is improving. Over the last almost 20 years, we have had some advances and some good news to share. The Expert Panel Report 3 (EPR-3), put out by the National Allergy Education and Prevention Program (NAEPP), was published in 2007. We are still using those guidelines in conjunction with the new 2020 guidelines from the NAEPP. From 2001 to 2018, the overall deaths have declined. Emergency room visits have been stable over this time period and asthma attacks have declined. New medications are always being developed.
Clinical Practice Guidelines
We know that asthma cannot be cured, but it can be controlled. The Expert Panel Report that came out in 2007 stressed the need to control asthma. We control asthma by looking at impairment and risk. It also identified new approaches for monitoring, a new age group to childhood management, and new treatment recommendations, which happens over time with the development of new medications.
They also chose to focus on patient teaching in a myriad of settings. This means that we want to make sure that our teaching is consistent whether the patient comes into the ER, is in the ICU, on the general floor, in the physician's office, or in the home receiving home care. We want to make sure that we focus on the information and make sure that it is clear across all of the continuum of care. In addition, it includes the control of environmental factors.
Goals of Long-Term Asthma Care
The goals of long-term asthma care include decreasing impairment and decreasing risk to the patient. Let’s look at each of these more closely.
Decrease Impairment
One of the goals of long-term asthma care, identified by the EPR-3 report in 2007, is to decrease impairment. We want to prevent symptoms such as coughing or breathlessness day or night or after exercise. We want to decrease the need for a patient to use their quick-relief inhaler to less than two times per week. We want to maintain near normal pulmonary function studies, and we want patients to maintain normal activity levels. We want those individuals to be able to do whatever activity they so desire and do it safely. We also want to meet the patient and family's expectations of and satisfaction with asthma care. We are going to do that through education.
Decrease Risk
We also want to decrease risks, including exacerbations and emergency room visits or hospitalizations. We want to give patients the proper medications that address inflammation so in order to prevent the loss of lung function in adults and lack of lung growth in children. We also want to provide optimal drug therapy with few or no adverse side effects. We want to give just the right amount of medication with few or no side effects.
Pulmonary Function Testing (PFT’s)
The normal value ranges of pulmonary function testing are based on the patient’s age, height, gender, and sometimes weight and race. The results are expressed in a percentage of the expected value based on those ranges.
Pulmonary function studies identify two types of lung disease. One is obstructive, in which the airways are narrowed and there is a decreased ability to exhale fully. This includes patients with asthma, emphysema, COPD, and bronchitis because they are unable to exhale fully.
Restrictive lung disease is also identified with pulmonary function studies. With restrictive lung disease, there is a decrease in lung tissue and a decrease in the ability to expand or in gas exchange capability. Some of the conditions that are restrictive include:
- Pneumonia
- Scleroderma
- Pulmonary fibrosis
- Sarcoidosis
- Multiple sclerosis
Spirometry
Spirometry measures the peak expiratory flow rate (PEFR), which is the velocity of air that is forcefully exhaled after a maximum inhalation in the first second. The EPR-3 report identified the use of the ratio of the Forced Expiratory Volume in one second (FEV1) to the Forced Vital Capacity (FVC) to class severity in children. They identified that this ratio may be more sensitive than measuring FEV1 alone.
The EPR-3 report also added an age group classification. Previously, children age five to adults were all lumped into one classification. Now there are three age group classifications: up to age four, children age five to 11, and children 12 years of age or older and adults.
Steps to an Accurate Diagnosis
Sometimes the diagnosis of asthma is difficult to come by and it is not definitive. Start with the history and the physical exam, and look at eczema, dermatitis, or atopic dermatitis in children. We know that children that have atopic dermatitis are likely to develop asthma. We also do spirometry, pre-, and post-bronchodilator. We may use the methacholine challenge if we are unable to have a definitive asthma diagnosis by our history, physical exam, and spirometry. The methacholine challenge causes a brief tightness in the airway which is then evaluated.
There are some individuals that find the methacholine challenge to be an irritant or they cannot tolerate that type of evaluation. The provider may need to consider doing a Fractional Exhaled Nitric Oxide (FENO) test. Also, allergy testing is involved and can be a skin prick, oral challenges, or blood work.
Since some other diseases mimic asthma symptoms, we want to evaluate the individual for gastroesophageal reflux disease (GERD) and obstructive sleep apnea (OSA). We will do a sinus evaluation to determine if the patient has rhinitis, sinusitis, or nasal polyps, all of which can create asthma-type symptoms. You may even do a chest X-ray for possible obstruction in the airway and an ECG in case it is a cardiac issue.
The FENO test measures lung inflammation. It can be used in lieu of the methacholine challenge if you have a patient that is not able to tolerate the methacholine and it is an irritant to them. It is used only if there is the inability to have a definitive asthma diagnosis. It is not for ages zero to four years old, only for older children and adults.
Severity Classifications of Asthma
There are four severity classifications. This was new with the EPR-3 report in 2007. There used to be an additional classification of asthma severity called mild intermittent. The four classifications are:
- Intermittent
- Mild persistent
- Moderate persistent
- Severe persistent
Keep in mind that all of the age groups are included in each of these classifications, zero to four, five to 11, and 12 to adult.
S.A.L.S.A.
S.A.L.S.A. is an acronym that helps you to stay organized when you are assessing a patient with asthma. S.A.L.S.A. stands for:
- Symptoms
- Activities
- Lung function
- SABA use
- Awakenings
We are going to first look at asthma symptoms. Then we will look at activities, lung function, short-acting bronchodilator (SABA) use, and awakenings.
Intermittent Asthma
Figure 1 shows an example of the impairment that an individual who has intermittent asthma would experience. The classification here is for most age groups, and highlighted in red are the age ranges that the other criteria describe.
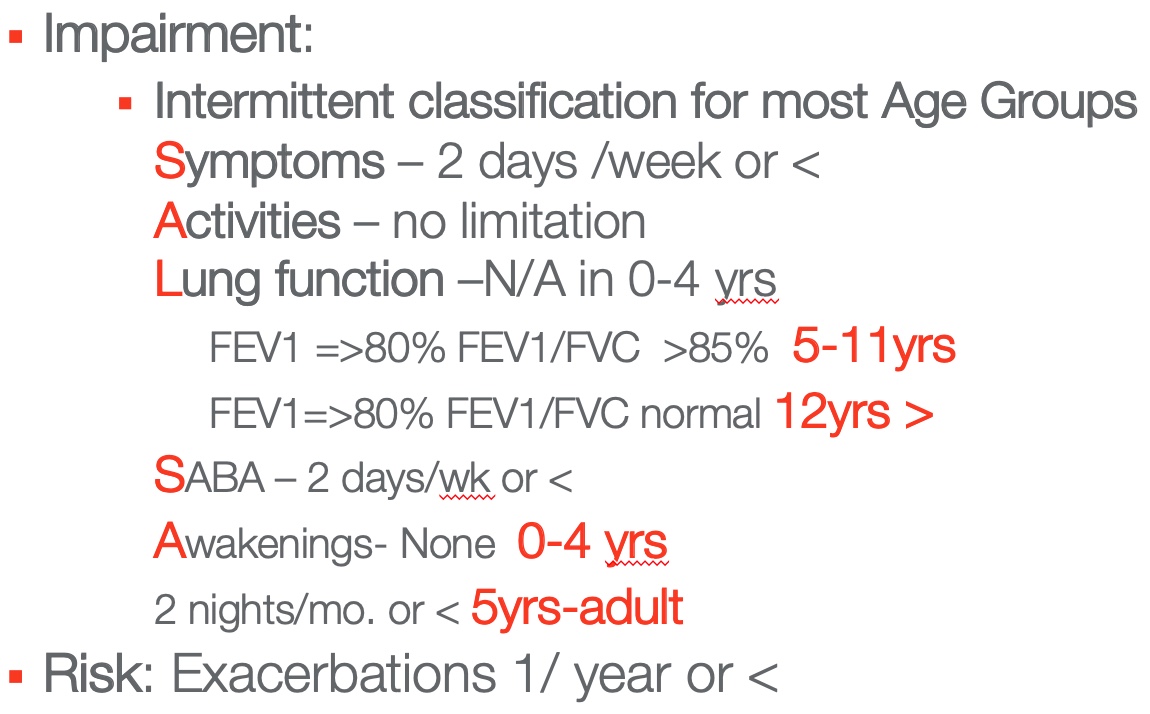
Figure 1. Example of the impairment an individual that has intermittent asthma would experience.
For an intermittent patient, there would be two days a week or less they might have asthma symptoms. There would be no limitations on their activities. You cannot get spirometry for children zero to four years, so that does not apply. Looking at lung function, for children five to 11 years, the FEV1 would be greater than 80% and the FEV1/ FVC ratio would be greater than 85%. For children 12 years and older, the FEV1 would be greater than 80% and the FEV1/ FVC ratio would be normal. The SABA use for all age groups in the intermittent category is two days per week or less of SABA use. For children zero to four years, there would be no awakenings, and two nights per month or less for children five years to adult.
The exacerbation risk for this group is one per year or less. This category of impairment includes individuals across all age groups that do not have significant symptoms that require very much intervention.
Mild Persistent Asthma
Now our asthma patient is having more symptoms and falls in the classification for mild persistent. Figure 2 shows an example of the impairment an individual that has mild persistent asthma would experience.
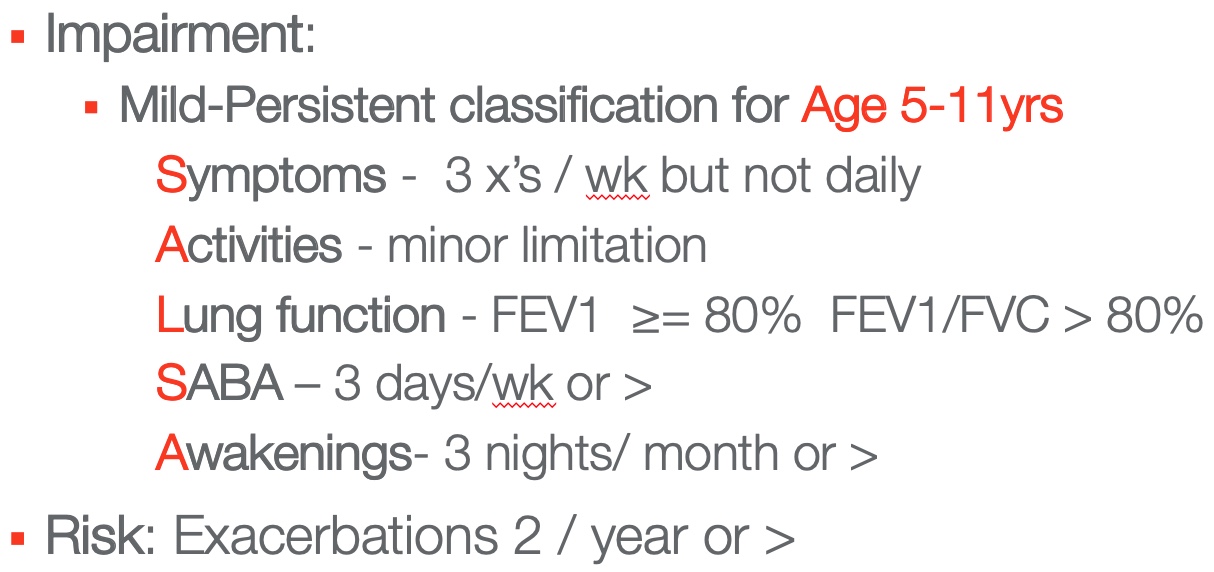
Figure 2. Example of the impairment an individual that has mild persistent asthma would experience.
This classification is for children ages five to 11 years. Symptoms for this class of individuals are three times a week, but not every day. There are minor limitations for activities in this category. Looking at lung function, the FEV1 would be greater than or equal to 80% and the FEV1/ FVC ratio would be greater than 80% of their predicted. The SABA use would be three days a week or greater and awakenings would be three nights per month or greater.
The exacerbation risk is two per year or greater. The symptoms are slowly increasing and there is more limitation with activities. Lung function is changing, SABA use is increasing, and awakenings are increasing in the mild-persistent category for individuals five to 11 years of age.
Moderate Persistent Asthma
Next is moderate persistent classification for ages 12 to adult. Figure 3 shows an example of the impairment an individual that has moderate persistent asthma would experience.
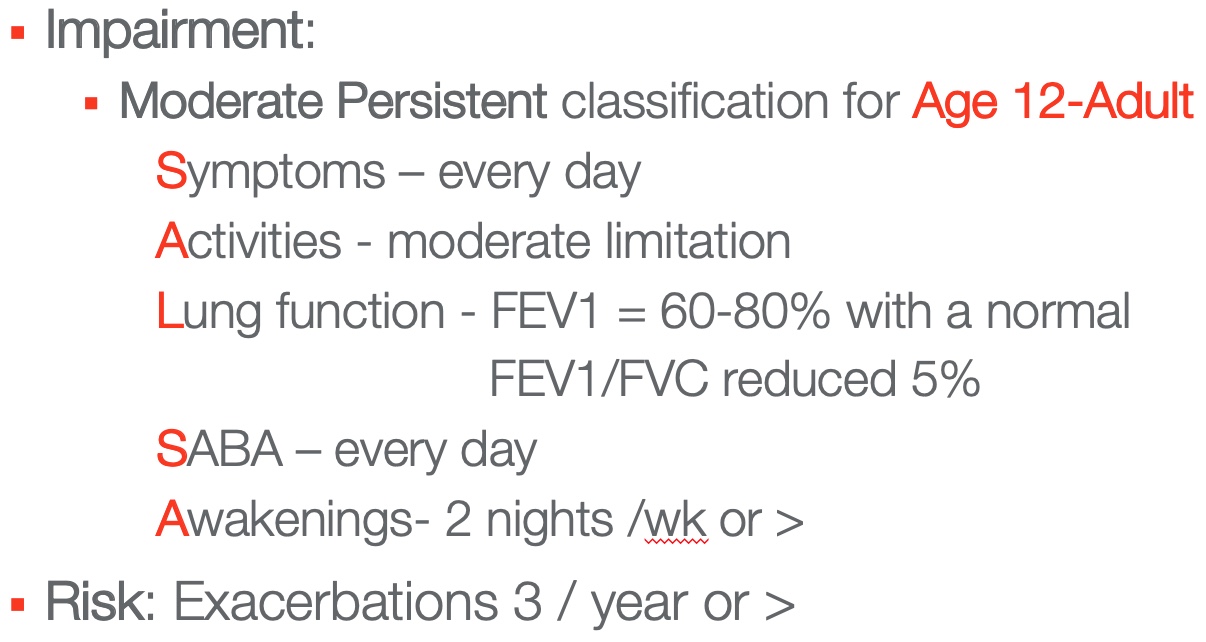
Figure 3. Example of the impairment an individual that has moderate persistent asthma would experience.
A patient with moderate persistent classification would experience symptoms every day. There is a moderate limitation to the activities that they enjoy. Lung function of FEV1 equals 60 to 80% of their normal with a normal FEV1/ FVC ratio, which is reduced by just 5%. There is SABA use every day by a patient with moderate persistent asthma. They may have nebulizers a couple of times a day or throughout the day, or inhalers. There are awakenings two nights per week or more.
The exacerbation risk for patients with moderate persistent asthma in this age group is three times per year or greater they would need to go to the emergency room or be hospitalized.
Severe Persistent Asthma
The final severity classification we will look at is severe persistent for children ages five to 11 years. Figure 4 gives you an idea of the S.A.L.S.A. criteria that this type of patient is experiencing.
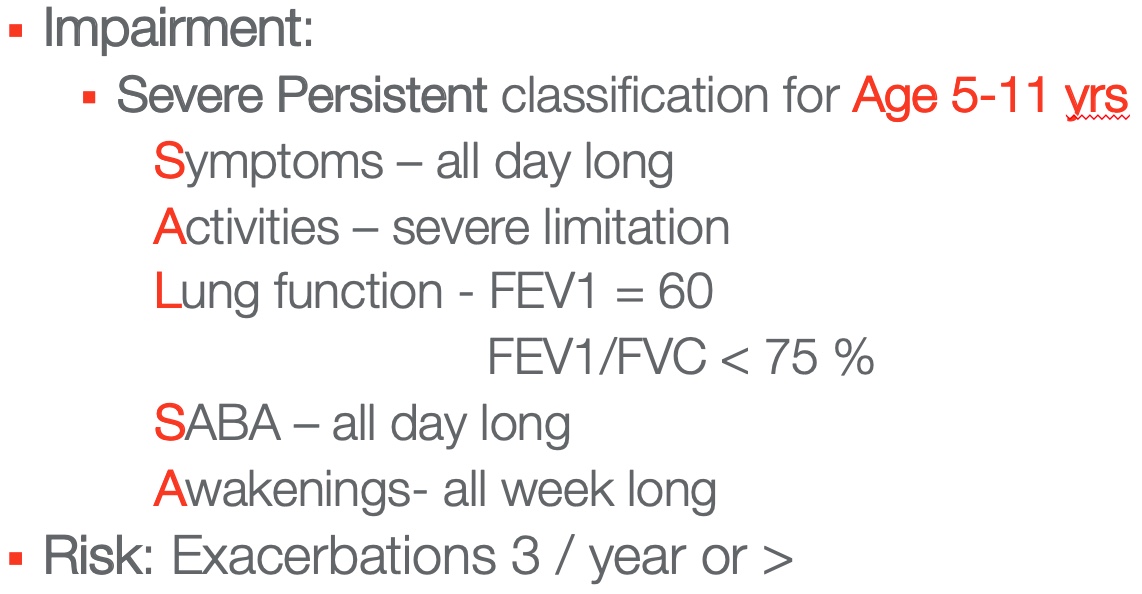
Figure 4. Example of the impairment an individual that has severe persistent asthma would experience.
Patients with severe persistent asthma would have symptoms all day long. They have severe limitations in activities. Looking at their lung function, the FEV1 is equal to 60% of their predicted. The FEV1/FVC ratio is less than 75% of their predicted. They are using the short-acting bronchodilator all day long. Awakenings occur all week long. Their exacerbation risk increases to three per year or greater.
Those are the impairment and risk categories and manifestations for the four severity classifications, from intermittent to mild to moderate and severe.
Keep in mind, all of the age groups are present within each of these severity classifications. This just gives you an idea. Remember S.A.L.S.A. because it can help you hone in on where your patient might fit in the classification system.
The new 2020 Clinician's Guide from the National Asthma Education and Prevention Program mentions that the 2007 EPR-3 report, which we discussed earlier, should be used in conjunction with this full report.
Stepwise Approach for Long Term Asthma Control
When we look at asthma, we always look at a stepwise approach for long-term asthma control.
- RX tailored to the level of asthma severity or control
- NOT to replace clinical decision making
- Step UP: After checks on RX adherence, inhaler technique, environmental control, and co-morbidities.
- Step DOWN: When asthma controlled for 3 months
We will start with six steps under each severity classification. These include the medications that are tailored to the level of asthma severity or control that is going on with that particular patient in that age group classification. It is never to replace the clinical decision-making that might need to be made on the fly for an individual. It is always individually determined.
When you are looking at the six steps and trying to determine which way to go, whether you step up and add treatment or whether you step down, you will only step up first if you make sure that you check on the patient's medication adherence. For example, before you move from step two in the plan and add medication, you need to evaluate if they are taking their medications and if they are taking them properly. Is their inhaler technique correct? Is their nebulizer technique correct?
Also, you want to look at environmental control. What has happened in their environment, if anything, that could be causing increased issues related to their symptoms right now? Look at any comorbidities. For example, maybe the individual has diabetes and their blood sugar is exacerbated at this time. Or maybe it is an older person and they have developed sleep apnea which is causing them to have more symptoms and they may need to have more medication.
Every time you move from one step to the next step and add medications, evaluate these things, every single time.
When do you step down? You step down when asthma in that particular step has been controlled for three months. That gives you a good handle on how things are being controlled. You may be able to entertain the idea of stepping down in dosages and treatment plans for that patient.
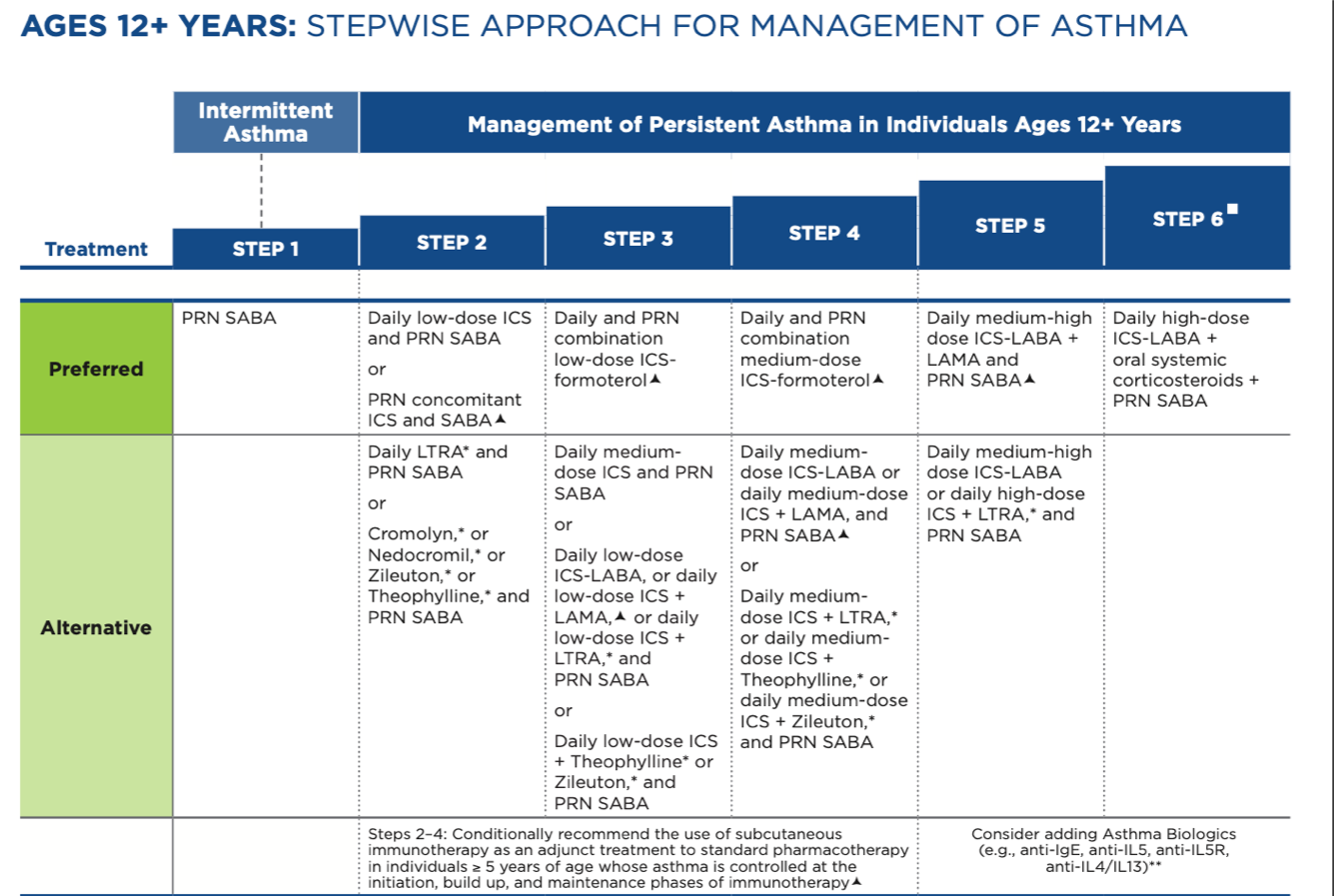
Figure 5. Stepwise approach for management of asthma. (www.nhlbi.nih.gov)
Figure 5 shows an example of the stepwise approach for ages 12 years and over. You can see that it goes from step one to step six and there is a category for preferred medication delivery and one for alternatives. When we start talking about medications, you will see that some of these medications are not the first choice for controlling an individual's asthma. They are alternative if the patient’s asthma is not able to be controlled. All of these steps under all these categories are available in the 2020 guidelines.
In general, the stepwise approach and treatment for an intermittent patient in that category are that they require no daily medications, but they do have a short-acting beta 2 agonist (SABA) to be used when they need it.
In general, if a patient is in the mild persistent category they will have a short-acting bronchodilator and a low dose inhaled corticosteroid to keep the inflammation down, make sure their airways are open, and ensure the smooth muscles are relaxed around their airways. This is especially important if there is evidence of a variable expository flow limitation by reduced FEV1/FVC.
Any age patient that is in the moderate persistent category, generally speaking, may need a low to medium dose inhaled corticosteroid with a long-acting beta 2 agonist (LABA). For a patient with severe persistent asthma in those categories, generally speaking, a high dose inhaled corticosteroid, a long-acting beta-agonist, and oral corticosteroids may be needed. That is a general medication regimen for all age groups in the stepwise approach over the severity classifications.
Exercise-Induced Asthma
Everybody wants to be able to do the activities that they so enjoy. Exercise-induced asthma or bronchospasm is triggered by vigorous or prolonged exercise or physical exertion. This could be a kid running amok in the playground or a teen that is a competitive athlete. It could be an older person that just wants to mow the lawn or go for a power walk. We want all of those individuals to be able to participate in those activities.
Typical asthma symptoms that manifest with exercise-induced bronchospasm include coughing, chest tightness, wheezing, shortness of breath, and unusual fatigue. It can begin during exercise, but it can worsen even five to 10 minutes after exercise or after that activity is completed.
How do we prevent exercise-induced asthma? For the individual that has exercise-induced bronchospasm, they should always warm-up before the exercise or activity and cool down after. There should be five to 10 minutes of warm-up and five to 10 minutes of cooldown
Another prevention for exercise-induced bronchospasm is to take medication. The short-acting bronchodilator should be taken 15 to 20 minutes before exercise. The long-acting bronchodilator should be taken 30 minutes prior to exercise.
Asthma Medications
There are two categories of asthma medications. It is important when we instruct our patients to let them know that there is a quick relief, oftentimes called rescue, and a controller or maintenance medication.
Quick Relief (Rescue)
The quick relief, or rescue, inhaler is used to promptly reverse acute airflow obstruction that is caused by bronchoconstriction. There is instant gratification when you use a quick-relief inhaler for your asthma symptoms.
Controller (Maintenance)
The controller or maintenance medication is for long-term daily control to achieve and maintain control of persistent asthma, whether it is moderate persistent or severe persistent. It can be inhaled corticosteroids (ICS) or systemic corticosteroids. Sometimes patients just need to take it in the morning or they may need to take it in the morning and at night or all the time to keep their symptoms and inflammation at bay.
Short-Acting Beta2 Agonists (SABAs) – Quick Relief
SABAs relax the smooth muscles around the bronchial tubes. Here is a list of common bronchodilators that we use for our patients.
- Albuterol
- ProAir HFA
- Pro Air Respiclick
- Ventolin HFA
- Proventil HFA
- Levalbuterol
- Xopenex
These are best used as rescue drugs PRN. They do not address the inflammation. When inflammation is not addressed with asthma, the lungs can remodel. Also, in younger children, if that inflammation is not addressed it can stunt lung growth.
The nice thing about SABAs is they have few side effects. When my mom used to take breathing treatments, she used Bronchosol in a nebulizer. Bronchosol increased everybody's heart rate by 16 or 20 points. We always had to stop the treatment if the heart rate went 16 points above their resting heart rate. Bronchosol was a tough drug, but the drugs have certainly been improved over time.
Long-Acting Beta2 Agonists (LABAs)
The long-acting beta2 agonists or bronchodilators (LABAs) relax the smooth muscle by stimulating beta2 receptors which antagonize bronchoconstriction. They do this over a longer period of time than a short-acting bronchodilator. For patients 12 years and older with moderate or severe persistent asthma, LABAs are used as an adjunct or with an inhaled corticosteroid for long-term control and prevention. This is where a SABA is not going to work for them. They need an ICS with a longer-acting bronchodilator. Serevent or Salmeterol is an example of that type of medication.
Rules of 2TM
The rules of two is another one of my favorite things like S.A.L.S.A. When do you need more than a rescue bronchodilator? You would want to ask your patient, do you take your quick-relief inhaler more than two times per week? Do you awaken at night with asthma symptoms or do you have a child that awakens at night with asthma symptoms more than two times per month? Do you refill your quick-relief inhaler more than two times per year? Think about that. Meter dose inhalers have 200 – 300 doses in them. If an individual is refilling that prescription more than two times per year, think of how often they are taking it.
The exception to that is for exercise-induced asthma. My daughter, Sophie, has exercise-induced asthma. She takes her inhaler nearly every day because she climbs mountains, mountain bikes, swims, and runs, and such. In that case, because it is the airways and the smooth muscle surrounding the airways that is the problem in exercise-induced bronchospasm, the increased use of a SABA is fine for that individual.
However, if the answer is yes to any of these questions and it is not exercise-induced asthma, a long-term anti-inflammatory medication may be needed.
Corticosteroids (Controller)
Corticosteroids or controllers are maintenance medications. The inhaled corticosteroids (ICF's) treat inflammation. They are most effective with individuals with persistent asthma. Also, they reduce both the impairment and the exacerbation risk for individuals. It is great because adverse effects are quite rare.
Here is a list of the types of corticosteroids that we use to treat patients. There are a couple that are relatively new in treating patients.
- Fluticasone HFA (Flovent)
- Budesonide (Pulmicort)
- Beclomethasone(QVAR)
- Mometasone(Asmanex)
- Ciclesonide (Alvesco)
- Flunisolide(Aerospan)
- Fluticasone (Arnuity Ellipta)
We always remind our patients to rinse their mouth and spit after using if there is a steroid or a steroid component to an inhaler because you can develop yeast infections in your mouth.
Inhaled Combination Medications
Inhaled combination medications may contain both inhaled corticosteroid (ICS) and a long-acting beta2 agonist (LABA). Here are some examples of inhaled combination medications containing both an inhaled corticosteroid and long-acting beta2 agonist (LABA).
- Advair Diskus/HFA - fluticasone, salmeterol xinafoate
- Airduo Respiclick - fluticasone, salmeterol
- Wixela Inhub - fluticasone, salmeterol xinafoate
- Breo Ellipta - fluticasone furoate and vilanterol
- Dulera - mometasone and formoterol
- Symbicort - Budesonide and Formoterol
Again, remind patients using these to rinse and spit if there is a steroid component to an inhaler.
Here is a list of the different types of inhaled combination medications that are used to treat patients. These inhaled combination medications contain both LABA and Long-Acting Muscarinic Antagonist (LAMA). There are a couple of relatively new medications on this list.
- Anoro Ellipta - umeclidinium, vilanterol
- Bevespi Aerosphere - glycopyrrolate formoterol fumarate
- Stiloto Respimat - tiotroprium bromide olodaterol
- Utibron Neohaler - indacaterol, glycopyrrolate
- Trelegy Ellipta - fluticasone furoate, umeclidinium, vilanterol
Long-Acting Muscarinic Antagonists (LAMAs)
Long-acting muscarinic agents are longer acting and open asthma constricted airways for 24 hours. An example is Spiriva Respimat or tiotropium. They are used for children six years of age and older. They may reduce the risk of asthma flares. They are an add-on or an alternative for individuals that have symptoms that persist despite a long-acting bronchodilator or an inhaled corticosteroid. It may be that the LAMA must be added on in the treatment of an individual that is not getting controlled with the LABA or ICS.
Oral Corticosteroids (Controller)
Oral corticosteroids are the controller or maintenance medication. The EPR-3 recommends that oral corticosteroids are only used for the most severe, hard-to-control cases of asthma due to the risk of side effects.
My mother was put on prednisone when I was born in 1952. She suffered from multiple side effects, including very brittle bones and vasculitis, or inflammation of her vascular system. She had very sensitive and thin skin. Unfortunately, she was never able to wean off the prednisone in her lifetime.
Often, oral corticosteroids have greater than 10 times the dose of an inhaled corticosteroid. When we use oral corticosteroids we are bringing out the big guns to take care of our patients. Use the burst and taper when we prescribe oral corticosteroids. We bump up the dose and then we always taper it off in the end. You cannot just stop the dosage dead in its tracks because it can cause harm to the patient. We can also do alternate day dosing, which is effective and can cause fewer side effects. Some of the oral corticosteroids are prednisolone, prednisone, and dexamethasone.
Leukotriene Modifiers (LTRAs)
The leukotriene modifiers (LTRAs) block the action of leukotrienes that cause inflammation, swelling, and tightening of the airways. Here are some of the medications that we use that are LTRAs.
- Singulair - montelukast
- Accolate - zafirlukast
- Zyflo - zileuton
It is important to remember that LTRAs are not used to treat sudden-onset symptoms. They are used as an adjunct with ICS therapy or as an alternative. Like the LAMA and the LABA, they are not frontline use. They are used as alternatives. Keep in mind that LABAs, not LTRAs are preferred in patients older than 12 years.
Biologics (Immunomodulators)
We have a very severe, difficult-to-control asthma patient if we are at the biologics stage. Biologics target specific cells and pathways that cause allergic inflammation. They are given via IV or injection for specific phenotypes of severe uncontrolled asthma that are determined by assessment. Biologics are very costly. Here are some examples of the different biologics that are used.
- Xolair - omalizumab
- Cinqair - reslizumab
- Fasenra - benralizumab
- Nucala - mepolizumab
- Dupixent - dupilumab
Sometimes there can be a threat of anaphylaxis. We want to be mindful of that. It is important that providers always keep their patients a little longer to observe them to make sure that they do not have any type of a reaction to the biologic.
Bronchial Thermoplasty
Bronchial thermoplasty is for patients 18 years of age and older with uncontrolled severe asthma. It is a minimally invasive procedure that uses mild heat to reduce airway smooth muscle, potentially leading to fewer severe asthma flares, fewer ER visits, and fewer days lost from activities.
However, the EPR-3 does not recommend in the new guidelines that bronchial thermoplasty be used. They do say if you have an individual that places a lower value on the harm that it could cause and a higher value on the potential benefits, that they might be an individual that with their healthcare provider might decide to do this.
PDE4 Inhibitors
Daliresp-roflumilast is an example of a PDE4 inhibitor. Those are often given sublingual or subcu. The EPR-3 does not recommend sublingual for the treatment of patients that have severe persistent asthma. They recommend subcu.
Emergency Management
For emergency management, we are going to assess the patient, treat them, do some labs, and give them adjunct therapy, including anything that they need to support them to get through this stage.
Here is an example of emergency management on a status asthmaticus patient who comes into the ER. We are going to get the best history that we can and do our clinical exam and check lung function. We may or may not be able to do spirometry on a patient that is admitting to the ER.
We will run some labs, including blood gas, CBC, or electrolytes when our patient admits. We will get their vital signs, their SpO2, and always ask if the patient is having pain, especially if they are a respiratory patient. We will observe their work of breathing and their accessory muscle use, and their breathlessness, especially with speech. If they are unable to even take a drink of water or say a few words, then they are in a crisis.
We might give them oxygen and a short-acting bronchodilator, along with some oral corticosteroids. If these things are not working, it is possible that aerosolized magnesium sulfate may be used in those critical cases. Magnesium sulfate increases and helps by decreasing the respiratory rate, increasing the peak excretory flow, and oxygen saturation. It provides a faster improvement in all of those signs.
Another option is to use heliox, which has a very low specific gravity when helium is mixed with oxygen. It helps to decrease resistance and decrease work of breathing for those patients. It also changes any turbulent flow that is going into that asthmatic patient as they are breathing and struggling into a laminar flow. It helps deliver pressure and oxygen more effectively. Usually, we give our patients a non-rebreather mask with the heliox. If they are still in triple trouble, we are going to put them on noninvasive ventilation and hope that that helps. Otherwise, we may need to intubate them and place them on mechanical ventilation.
A Partnership in Asthma Care
Asthma care is a partnership. There are many goals of patient education, and we always want to think about these goals as we are educating our patients.
- Increase patient’s understanding of asthma
- Improve self-treatment skills
- Enhance patient outcomes and satisfaction
- Boost patient confidence in treatment
- Increase patient and family adherence with the treatment program
- Shared decision making
- Treatment aligns with patient preferences and cultural values
- Build trusting relationships
We want to increase the patient's understanding of asthma, including their families. We want to improve their self-treatment skills, such as taking their MDIs with the valve holding chamber. Make sure that they take them on time and that they take their nebulizer properly.
We also want to enhance their outcomes and their satisfaction with how we are caring for them. We want to boost patient confidence in their treatment. With more knowledge, patient anxiety will be relieved, especially when they know and understand their disease and know that it can be treated and they can be cared for safely.
We want to increase patient and family adherence to the treatment program. We can do that by educating them and making sure that they understand what is important. We also want to participate in shared decision-making. That means it is not just the healthcare provider making the decisions for our asthma patients, it is our asthma patient and family along with the healthcare provider. When we are making those decisions, we want to make sure that the treatment that is being suggested or prescribed aligns with the patient's preferences. A simple example would be the patient prefers a nebulizer instead of an inhaler.
There may be cultural values that are preventing a patient from embracing the type of regimen that the provider is suggesting or prescribing. We want to build trusting relationships with our patients as well.
Understanding Asthma: Building Blocks for Better Breathing
Understanding Asthma: Building Blocks for Better Breathing is a magazine published in 2019 by the Allergy and Asthma Network. It has so much great information about asthma described in lay terms so it is easy to understand. It includes myths of asthma, how you diagnose it, how you treat it, the types of medications, the Asthma Action Plan, and everything I am discussing with you today. You can download it for free from the Allergy and Asthma Network.
In my community education, I have provided these booklets to the schools, assisted living facilities, and childcare providers. It is a good go-to because you know that it is trusted information and easily explained.
Essential Patient Teachings
We need to teach and reinforce with patients at every opportunity every single time we see them. This is true even if they are frequent flyers and we see them all the time.
Basic asthma facts. We still want to make sure that they understand the abnormal and normal conditions of asthma. They also need to understand the role of inflammation and what role it plays in asthma, as well as what happens during an asthma attack.
Role of medications. It is also important to make sure patients understand the role of quick-relief rescue and controller or maintenance medication. That is where in my community teaching, and even in the hospital, patients would get confused. They didn’t know which one to take every day and which one to take only when they needed it. That is something that we have to continue to hammer home every single time we see our patients.
Patient skills. At every opportunity, we are going to assess if they are taking their meds correctly at the right time, including inhalers, spacers, and nebulizers. Are they taking their inhaler with a valve holding chamber or spacer? Are they taking their nebulizer properly? Are they cleaning the nebulizer as they need to?
We want to make sure that they can identify and avoid any of their asthma triggers. We want them to perform self-monitoring to assess their control. We need to monitor the utilization of the Asthma Action Plan. We need to teach these things, and if they cannot demonstrate how to use the inhaler within a valve holding chamber or demonstrate how they take their nebulizer treatment, then you have them explain it to them. That is the way that you can assess them if they are unable to demonstrate it for you.
Also available in Understanding Asthma: Building Blocks for Better Breathing is a visual aid of respiratory treatments available. The Respiratory Treatment Poster is also available for download from their website. This is a great visual to show patients the different kinds of treatments and how they are different.
The thing that can be overwhelming for our patients is every one of these inhalers is proprietary so they all may work just a little bit differently. It is important for patients to understand the maintenance that you do. Some inhalers may not need to be taken daily. They may not need to take them all the time. Sometimes you have to release the medication and activate a dose here and there once a week or once every two weeks if you are not using it to make sure that you are getting an accurate dosage when you do need the inhaler.
Self-Management Training
The outcome we are looking for is to reduce morbidity in asthma. We want to decrease the use of healthcare providers. We want patients to stay home and not have to go to the emergency room or doctor multiple times during the season that affects them the most. Studies show the greatest benefit is when a written self-management asthma action plan was used. There are action plans for many different diseases, including CHF, COPD, and anaphylaxis. They are very helpful.
Asthma Action Plan
What are the key components of an asthma action plan?
- What medicines to take
- When to take them
- How much to take
- When to get help
- Share your plan
- Update every 3-6 months with your healthcare provider
This plan is going to let the patient and others know what medicines to take, when to take them, how much to take, and when they need to get help. It is very important for a parent to share their child’s asthma action plan with coaches, the school, and Grandma and Grandpa, or other caregivers around the child. They need to make sure that that asthma action plan goes with the child and that everyone, including the child if they are old enough, knows what to do when their asthma begins to get worse.
Healthcare providers should work with the patient to update this asthma action plan every three to six months. Because we know that symptoms can come and go, and there could be a time where maybe the patient is on an inhaled corticosteroid and they are doing fine, they may be able to wean off that inhaled corticosteroid. This is especially true if it is not the season where they have difficulty. The asthma action plan is a very important part of managing asthma. You can see examples of an asthma action plan in Understanding Asthma: Building Blocks for Better Breathing and at www.nhlbi.nih.gov.
Symptoms
An asthma action plan can be based on symptoms, such as coughing or a runny nose. For example, let’s say Mom and Dad know that every time Billy starts coughing at night they end up in the ER a couple of days later. Or maybe it is Sally has a runny nose and every time Sally has a runny nose, they end up in the ER a couple of days later.
The asthma action plan that is based on symptoms, for example for Billy and Sally, is that as soon as Billy starts coughing at night or Sally starts with a runny nose, then the parents know that they need to activate the medication regimen that the physician has prescribed.
Peak Flow Monitoring
The asthma action plan can also be based on peak flow monitoring. Peak flow measures the amount and rate of air that is forcefully exhaled from the lungs in liters per minute after a maximum inhalation. There are indicators for red, yellow, and green zone on the peak flow meters.
The personal best peak flow is part of the asthma action plan and is a key component for individuals that are able to perform this maneuver. Personal best is the highest measurement your patient can reach during a two-week period when they feel their best and are free of asthma symptoms. To get their personal best, they will take their readings when they wake up and when they go to sleep for two weeks. They will also take readings before and after they take their inhaled medications, whether it is a nebulizer treatment or an inhaler.
The 3 Zone System
Next, we calculate the red, green, and yellow zones. If your patient's personal best peak flow reading was 400, the asthma action plan will look at 80 to 100% of that ideal number for the green zone, which is 320 to 400. A peak flow reading in that range signals all clear. If they are in the green zone, they follow whatever the green zone indicates for them. For example, if it is a severe asthmatic, the green zone means that they are probably taking their inhaled corticosteroid and they are taking their short-acting bronchodilator when they need it.
If they fall down in their peak flow reading they are likely creeping into the yellow zone. The yellow zone is 50 to 79% of that personal best and signals caution. The asthma action plan is going to tell you what to do in the case you finding yourself in the yellow zone, whether it is for symptoms or for peak flow dropping. The asthma action plan is trying to prevent anybody from ever going into the red zone.
If someone ends up in the red zone, that is less than 50% of their ideal number. That means is a medical alert. The patient should take their quick-relief medication and call their doctor or 911. Sometimes the physician will say to take the inhaler every three minutes until 911 arrives. Physicians will individualize instructions for each person as they enter into these zones to make sure that they stay safe.
Asthma Treatments
Metered Dose Inhaler (MDI)
Let’s take a minute to review all of these steps when a patient is using the metered-dose inhaler (MDI).
- Use a “spacer” or valved holding chamber that delivers medication more effectively and safely
- Sit up or stand
- Shake well
- Exhale completely
- Activate the dose
- Inhale SLOWLY and deeply
- Hold breath up to 10 seconds
- Wait 1 minute between inhalations
Make sure they use a valve holding chamber. Those can be expensive but you can look around and likely find some at a lesser cost. Oftentimes inhalers are ordered by the physician but never include a valve holding chamber or a spacer. Patients usually do not know to ask about that so you might check with your patients to make sure that they have a valve holding chamber.
They will need to sit up or stand, shake it well, exhale, activate the dose, then inhale slowly and deeply and hold their breath up to 10 seconds if they can. Sometimes that is impossible for people to do. But any kind of breath-hold is going to be good because you can tell your patients that if they breath-hold and then they wait a minute between their inhalations, especially if they are taking a quick-relief medication, then that next dose is going to be more therapeutic because already that first dose is relaxing the tiny muscles and opening up their lungs so that next dose is truly then more therapeutic.
The Allergy and Asthma Network also talks about respiratory tools on their website. There are a variety of different valve-holding chambers and spacers. Spacers are less expensive, but patients using spacers need to keep in mind they need to keep their lips really tight around the mouthpiece to make sure that that medication does not escape.
The In-Check Dial Inspiratory Flow Meter is a handheld device with a dial to test the ability of patients to inspire the proper amount at the proper negative pressure to activate different types of inhalers, whether it is DPI or a metered dose inhaler. This reinforces that the patient has the proper MDI or DPI to take and that they have the strength to do it.
Dry Powder Inhaler (DPI)
- Sit up or stand
- Load dose of medication
- Hold the device level
- Exhale completely
- Put mouth tightly around the mouthpiece
- Inhale QUICKLY and DEEPLY
- Hold the breath for 5-10 seconds
- Do not exhale in the device, shake it or wash it
- If steroid component rinse mouth
For dry powder inhalers, remind patients to sit up or stand, load the dose, hold the device level, and exhale completely then do a quick and deep breath in. They should also hold their breath for 5-10 seconds. Even though it is dry and deposits itself on the warm, moist lung, we still do a breath-hold. They will not exhale in the device and we do not want them to shake it or wash it. They should always rinse their mouth if there is a steroid component.
Sometimes we think the patient may not have gotten the full dose. If that is the case, let them inhale deeply and quickly again. The same thing goes for the metered-dose inhaler with a child with a mask valve holding chamber. Let them take more than one breath if they need to or if they are unable to take that big, deep breath with the breath-hold.
Delivering an Aerosol Treatment
Aerosol treatments change the liquid medication into a fine mist. The best way to deliver an aerosol treatment is with a mouthpiece. I always tell my patients in the community, family members, and others I am teaching to take it with a mouthpiece if at all possible. They should be watching the mist disappear every time the patient takes a breath in. This lets you know it is getting in the lungs. Children and elderly people will hold it in their mouth and breathe through their nose and they will not get the medicine. If you have to, you can use an aerosol mask to deliver the treatment, but it will be blowing in their face and it is not as effective. Always remind your patients to take slow, deep breaths with an aerosol treatment. They also should cough and clear any loosened secretions before and after the treatment.
To properly clean and store the equipment, take it apart and rinse it after each use, then let it air dry. Once a week, soak it in vinegar water then let it air dry. Always remind patients of that. There are many portable nebulizer machines now. DME companies and insurance companies generally are very good at supporting that type of equipment.
Asthma Triggers
Asthma patients must know their triggers. We want to teach our patients about asthma triggers because in this case, knowledge is power. Especially if they are a young child they need to know that chalk dust is a hard thing for them. When lawns get mowed, mowed grass can be a trigger. With asthma, it is important not only to know what the triggers are but to also be able to mitigate those triggers. The 2020 asthma guidelines stated that you cannot just do one step in mitigating a trigger. Here is a list of asthma triggers.
- Tobacco smoke, wood-burning
- Mold and mildew
- Pollutants resulting from poor ventilation
- Pets with fur or feathers
- Cockroach or mouse droppings
- Strong odors (chemicals, cleaning agents, paint, air fresheners, perfumes, dry erase markers, magic markers, glue/paste, fumes from soldering or welding)
- Hormonal changes
- Cold/damp weather
- Exercise
- Extreme emotional expression (stress, anxiety, anger or crying)
- Mechanical responses such as prolonged sneezing, yelling or laughing
- Common cold, influenza, or other respiratory infections
- Certain foods – peanuts, milk, soy, shellfish, eggs
This is a pretty complete list of asthma triggers. My mom was allergic to everything, including mold and mildew. My dad actually smoked for a while. The only thing that really did not bother my mom on this list was she never had asthma issues with extreme emotional expression (stress, anxiety, anger, crying), and hormonal changes never bothered her. She was not allergic to a single food. She just had highly allergic asthma to just about everything else. Even sneezing, yelling, and laughing did not bother her.
Let’s take a look at an example. There are a husband and wife who have been married for several years. They have a new baby who is exhibiting asthma symptoms. They are just not sure what it is. They have a dog and a cat, but are not sure what is causing the asthma symptoms. When you identify what the interventions are or the mitigation strategies for a trigger, you can begin to rule out what that might be.
Reducing Asthma Triggers
Back to our family with the new baby who is having asthma issues. They have been to the doctor and they have been treated.
Animal Dander
They do have a dog and a cat, so what can they do? They can keep the furred or feathered pet out of the home. If the pet has always been an indoor pet, what do you do? Keep the patient or the pet out of the sleeping area of the child and keep the door closed.
Cover air vents with a heavy material to filter the air because the animal dander gets around. In addition, the saliva of cats and dogs also gets on the material. That can also be an irritant, not just the dander.
Remove carpets and furniture with cloth covering. If the child has multiple issues and it is still not helping to have the dog out of the bedroom, then the parents need to think about putting the dog or cat out of the house or finding a new home for it. They could also do more of these interventions. The 2020 guidelines recommend a wide spectrum of mitigation strategies, not just one.
Now the child is a toddler and is having issues at night with awakenings and wheezing and trips to the doctor.
Dust Mites
Dust mites are little critters that we cannot see that build up in our bed linens and feed on our dead skin cells. We want to make sure that we can totally get rid of them. To reduce dust mites, encase the mattress, and pillow if there is one, in a dustproof cover. Wash bed linens in either hot water or cold water with bleach. That is the only thing that is going to kill dust mites.
Another thing to reduce dust mites is to reduce humidity in your house to less than 60% because dust mites like it warm and humid. Remove carpets from bedrooms, because they like to find their little home in carpets. Keep stuffed toys out of the bed, and wash or freeze them weekly, for 8-12 hours to get rid of dust mites.
Thinking back to the family, the toddler is still having issues at night. The dog is out of the room and they are washing the linens and encasing the mattress, but there are 12 stuffed animals lining the crib that have never been washed. The parents need to continue to search for the cause and try to rule things out, so they should put the stuffed toys in the freezer and change the pillowcase every night.
Cockroaches/Mice
The problem with cockroaches and mice is that they poop. Keep food and garbage in closed containers to help keep them away. Use poison baits, powders, and gels if needed, but always keep them away from children and pets. If a spray is used, make sure you stay out of the room until the odor clears.
Indoor Mold
Indoor mold is pretty sneaky because you do not always check under the hot water heater for mold. If mold is an issue for this individual, you are going to want to be a real detective. Even in places we do not always look, such as under the refrigerator or vanity, there could be dripping water or mold under there. Fix leaky faucets and pipes to help prevent mold.
Make sure that you clean moldy surfaces with bleach cleaners or non-toxic cleaners. For example, when vinegar and baking soda are mixed it effervesces. That combination can clean and disinfect any area just as well as bleach. Vinegar and baking soda are what kids use in science experiments to make the volcano erupt.
The other thing about indoor mold is it can be in other areas that you do not notice such as up by the light in the shower, down by the drain, or along the baseboards on the floors. Another strategy in bathrooms is to have a rug that does not have a rubber backing because when you get out of the tub or the shower, that water and wetness can grow mold there too.
Pollen and Outdoor Mold
Pollen and outdoor mold can be a real issue. Thinking about our family, the toddler is still having problems at night. The parents have done everything they could so far. Another strategy is to keep the windows closed. Staying indoors with the windows closed from late morning to afternoon when pollen counts are highest is also helpful. That is true in the spring with the flowers and the trees, and in the fall with the tall grasses and mold.
It can also be helpful to take a shower before bed. If there is a bed partner, they should shower too. Thinking about the child, now a curly-headed toddler who goes out and plays, they may not get a shower or a shampoo every day. They may still be exhibiting symptoms. We want to make sure that we are trying all the ways to reduce triggers for the child. Also, for individuals that have allergic asthma and the seasons are a big problem for them, it is important to begin the anti-inflammatory medication before the first buds of spring or before the fall grasses bloom.
Tobacco Smoke
If you smoke, ask your doctor about ways to quit. Ask family members to quit, too. When I was a respiratory therapist in the early 80s we smoked in the cafeteria. The thought of that now makes me cringe. Do not allow smoking in your home or your car. Secondhand smoke is highly toxic and can get into your bloodstream. Third-hand smoke is a heavy odor on clothing, curtains, and furniture that is also harmful.
Our toddler is still having issues. Mom and Dad do not smoke in the house when the child is there and they do not smoke in the car when they are in the car, but they still have third-hand smoke on their clothing and in the car. They hold their child and he is still having symptoms. Third-hand smoke could be a trigger for the child.
Smoke, Strong Odors, and Sprays
Things like wood-burning stoves, fireplaces, or kerosene heaters can also be very irritating to certain individuals. Try to stay away from those things and any other items that have strong odors.
Vacuum Cleaning
If you have asthma, then vacuum cleaning can be tough for you. You might be able to get someone to vacuum for you once or twice a week. If you have an individual that has asthma, you want them completely out of the room during vacuuming and for a short while after. You want to wait for all the dust and particles to settle. Think about when you vacuum and the sun shines through and you see everything in the atmosphere. If you are an individual with asthma and you are vacuuming, use a dust mask and a vacuum cleaner with a double-layered or microfilter vacuum bag or a vacuum with a HEP filter.
Sulfites in Foods and Beverages
There are sulfites in foods and beverages. They are primarily in things like shrimp, fruit, and processed potatoes. Beer and wine also have sulfites. Sometimes when children are introduced to new foods, they may not have a reaction right away. It may take some time for them to eat those foods multiple times before they develop a reaction. It is important to keep your eye out for any reactions to foods.
Cold Air
Cold air is also an asthma trigger. Tell patients to cover their nose and mouth with a scarf. We know that the first dry snap and the cold snap of air can make anyone have a coughing fit when they breathe in.
Electronic Cigarettes
There are many types of electronic cigarettes. In 2014, there were 460 brands of e-cigarettes on the market. They are filled with liquid, have a heating device, and are battery-operated. The problem is they are not subject to regulation. Some states have banned sales to minors, but you can get them online, so it does not really stop people from getting them even if they are minors. They have unknown health effects.
A study by Rigotti in 2015 found that those that used e-cigarettes by the time they are in the ninth grade are more likely to start smoking traditional cigarettes&
