Editor’s note: This text-based course is an edited transcript of the webinar, Burned Out: How to Heal and Protect Our Mental Health at Work, presented by Sophie Nathenson, Ph.D., Medical Sociology.
Learning Outcomes
After this course, participants will be able to:
- Describe the three main components of burnout and its physical and psychological effects
- Identify the environmental and individual factors in burnout
- Explain practices for coping with stress and stressors to enhance wellbeing
Defining Mental Health
This is a topic that I am sure you are hearing maybe way too much about. As I was reflecting on why even listen to a talk on something that a lot of you have probably experienced yourself, I want to say. Sometimes, creating some definitions and context for words we are hearing much about can help bring the conversation down to something we can start to relate to and learn more from. I am a medical sociologist. I know it sounds like I do not have a lot of credibility with respiratory. My mother is a respiratory therapist, and my father is a nurse. I grew up around healthcare, especially in rehabilitation settings. My job is to study the societal and community-level factors in our collective well-being. Unlike a health professional that may be addressing the health of a person, I am studying the health of the collective of a group of people, the context for this talk as we talk about burnout and as it relates to mental health.
Even though we talk about the individual, we are taking a big-picture perspective to define mental health so that we are all on the same page. It is our emotional, our psychological, and our social well-being. A common theme as we are talking about mental health is that in our society and in many societies, we tend not to see mental health in the same way we see physical health. Physical health is oftentimes more apparent physically. It is something we can more easily describe and talk about, and we can treat it, of course. What I want us to think about together today is similarly thinking about mental health. Meaning there are symptoms. You can have an illness like a cold and get over it quickly. It can be more of a chronic illness that you have to manage. It is separate from the core of your personality. Signs of poor mental health might include feeling low energy which most of us feel from time to time—unusually upset or worried, feeling helpless and hopeless, feeling numb where you do not know what you feel. Having mood swings, having thoughts of harming yourself or others. These are all the symptoms. Specific illnesses include depression, anxiety, bipolar disorders, schizophrenia, eating disorders, paranoia, and many more. Regarding our mental health, like physical health, biological, situational, and family-based factors are at play here.
Mental Health in America
How are we doing as a society? This might make you laugh, roll your eyes, or feel bad because our collective, as we found through the pandemic, Americans have many underlying conditions. We have a lot of underlying chronic physical illnesses. We have a lot of underlying economic issues, financial constraints, and social troubles as far as how we interact with each other and how different groups interact. Additionally, we have mental health issues as a collective. Now it is very common for us to look at the research pre-COVID, during the pandemic, and potentially post-pandemic on how things have changed. Pre-COVID, about one in five adults were experiencing mental illness, which is probably a low estimate because these are the people reporting it. It is very common. Considering something that is an extreme symptom, or at least it seems like it is, suicidal ideation is rising yearly, with about 4.6% of adults having serious thoughts of suicide. Looking from the perspective of our thoughts, we may feel we are creating, but it is also happening to us. It is a very interesting dynamic but having these thoughts can be considered a symptom of a mental illness. This is an important point that we will come to later as well.
Regarding people in the working world, eight in ten employees across the work sector said the pandemic negatively impacted their mental health. Again, this is one of those things where it is like, "Oh, of course, that is obvious." Because it is obvious and makes total sense, it does not mean it is not a serious issue affecting people's lives. Looking at healthcare workers who have experienced higher levels of poor mental health, we will talk about why that is. As a side note, medical sociologists study the healthcare system as its society. It is an outsider's perspective of what is going on here. You all have an insider perspective. We can blend those paradigms.
What I got from it as I started to look at the high percentages of people that have these mental illnesses, one of the common threads is that people that are experiencing these illnesses are not necessarily getting help, and that goes back to this paradigm of, for whatever reason, if you have got diabetes and you need insulin shots, it is more familiar to us that type of a dynamic versus having thoughts of self-harm and needing XYZ treatment for it. It is not as much in our common lexicon. This ends up being a tough situation for us that are struggling with mental health issues.
Measuring Mental Health
- Beck Depression Scale/CESD
- General Anxiety (GAD-7) • Maslach Burnout Inventory
- WHO-5 Wellbeing Index
- These measures help to keep track of prevalence of mental illnesses and get people the appropriate types of treatment, as well as supporting research
Measuring mental health becomes important when looking at the research. Again, I think about this all the time, like why is it important or interesting or relevant or even an added value to learning about the research on a topic if you are dealing with it daily? Our communities are built around the individual and getting self-help versus research about large groups of people. You have probably heard of psychology and do not hear about sociology very much in wider society, but it is all about measuring large groups of people. These scales that we have, the depression scale and general anxiety, are used. They are tested and used repeatedly to ensure people interpret the questions on these scales. They are little surveys in a similar way that we can see the prevalence in these larger groups. Why do that? Part of the reason is to brainstorm what we can do to improve some of these issues. Like in public health, that sector is designed to prevent or reduce the spread of disease. That is one way. We can also learn about other factors affecting mental health beyond the individual.
What is Burnout?
- “a combination of exhaustion, cynicism, and perceived inefficacy resulting from long term job stress”*
- Especially common among deeply dedicated
- Linked to dishonest behavior, decreased altruism, and alcohol abuse
- Detrimental to patient care, mortality, law suits
- 50% of physicians, 43% nurses, 79% of RTs in Covid
Burnout is one of these terms we have heard, which ultimately is a good thing. If there is one thing that we can get from the pandemic and how much stress it created in our communities, it also did shine a light on a lot of issues that were already there, but they are rising to the surface as far as the awareness level. It is always the first step to addressing any issue related to health and well-being on the social scale or at the individual scale. Burnout may be recognized as a term that has been used to talk about drug addicts that have done many drugs. They are burnt out. Their brains do not work as well. That is actually where the term came from. A psychologist was studying people who worked at an addiction center, not those suffering from addiction, but those who worked there in New York City. This was in the '70s. He was observing and studying them and noticed this ailment, the phenomenon happening to these people. They were dedicated to their work. They were working long hours, working more and more and more, and starting to get exhausted, getting more cynical about the whole situation, both the individual people they were working with, the system, and all of that.
They were starting to feel like they were not being effective, but they were also starting to stay at work even when they did not have to because they did not have anything to say, "go home to." That paints a pretty dark picture of where this term originated, these very deeply dedicated people that were in a people-serving profession. You are health professionals, educators, and people working in social services and nonprofits. There are lots of people serving fields. It draws people who want to help others, and the dynamics around burnout affect everything. The person, family, friends, and any social situations. It is also been linked to dishonest behavior, decreased altruism, alcohol abuse, and abuse of other substances. It is detrimental to patient care and to mortality. It is linked to lawsuits, and it is very common. According to these definitions, about half of the physicians, 43% of nurses, and 79% of RTs in the COVID pandemic said they experienced burnout. You may have experienced it yourself. I am now hearing people talk about how you cannot recover from burnout. What is meant by that statement is that it is the idea of getting to the point where you essentially do not want to do your job anymore. Now seeing this trend of great resignation and people that can leave, want to leave, and leave their jobs, we are talking about being unable to recover. You can recover, and it can be prevented. It can be healed. There are all sorts of things that we can do, it is a holistic approach. It shows that it is prevalent does not mean it is something that everybody will deal with, and it should be normalized. It is something that is a major concern.
Measuring Burnout
- Emotional Exhaustion (EE): feeling maxed out and not able to offer emotional support
- Depersonalization (DP): negative/cynical attitude towards/of the patient
- Personal Accomplishment (PA): is reduced, plus escapism
The three components of measuring burnout are these three aspects, and you can reflect if you have had these before. I know I have had burnout and a long recovery process to recover. Emotional exhaustion is the feeling of being maxed out and how you know you get to that point where you cannot offer emotional support to other people. It is the concept of not having a full cup to offer others. Depersonalization is this negative or cynical attitude towards the patient. Take a moment and consider that if you have had a day where you come home, and complain about this patient that is not taking care of themselves, is being rude to you, why does it even matter? The system is messed up anyway, and these people are not improving. Or it is insane at work and this spiraling negative attitude. Consider for a moment that it may not be about your core attitudes, character, demeanor, and disposition that it could be a symptom of burnout. Decoupling is important because it can be scary thinking about any mental illness. Like this is what I am like now, this is me, and it will always be like this, which is scary.
Looking at these measures as symptoms are things that can "come and go," are part of this thing that we can catch like a cold, and it can be persistent, but it is not part of our core. Your feeling of personal accomplishment is reduced. Add to that escapism which is very common, and a lot of this stuff talking about the research and the patterns is textbook. It almost decouples it from something "wrong with you." These are patterns that are observed in people over time. This idea of personal accomplishment is huge. This is also related to workload, and I work with many people with many goals, part of the healing process is to reduce those goals by about 99% to start building that sense of accomplishment. We will talk about the external and workplace factors that we cannot control that are pressing on all of us. These are the three pieces of burnout as far as how it is measured from almost a clinical standpoint. We talked about filling your cup and being able to offer that to others. We did not talk about how to fill your cup. We will get to that.
Burnout’s Impact on Empathy
How burnout then affects empathy? Again, if anything, you can take from getting this potentially different perspective on burnout is that it is not you, right? It is like asthma or diabetes, it is not me. It is a separate issue that we can address. Burnout impacts empathy, and there is a negative association between burnout and empathy. Burnout includes physical depletion, feelings of helplessness, and negative self-concept. Once your negative self-concept is triggered, whether you are aware of it or not, that triggers something else. The negative attitudes about work, about life, about other people, and you can see how this affects other people. The thing about mental illness, possibly even more than physical illness, is that it affects other people. Empathy, the textbook definition, includes your emotions, how you think about things, cognitive, behavioral, and moral components at the core, and being able to communicate your understanding of another person's perspective. For example, the patient and the relationship between burnout and empathy, how there is such an if-then correlation here helps to explain what we see when we look at how it affects patient outcomes.
Stigma
Stigma is one of the biggest barriers to addressing mental health. Again, think about a physical illness in that you have these symptoms. Let's say you have a common cold. Imagine having this and not doing anything about it. You are continuing to do all of your work and all of your physical activity. You are not drinking fluids, and you are not getting rest. You are not doing any self-care that we associate with recovering from the common cold. It could turn into something worse or linger more, which is how mental health is. When there is a stigma that it is a character flaw, you are crazy, weird, unable to manage your emotions, or dangerous. There are many stereotypes about mental illness preventing treatment. There is also a self-stigma that can prevent getting treatment. Most physical health concerns have less stigma. There are physical health issues that have had a heavy stigma. At one point, cancer was very stigmatized, and people did not want to go near people with cancer, as was the AIDS virus and mental health.
Healthcare & Mental Health
- Research shows a relationship between the healthcare professions and mental health conditions, suggesting there are aspects of healthcare work that impact our mental health, such as:
- Working conditions
- Others before self
- Stigma
Turning our attention now to healthcare and mental health and looking specifically in those areas of society in healthcare organizations where you all likely work. The research does show a relationship between the healthcare professions and many mental health conditions. In sociology, we are comparing groups. We are not comparing individuals. I also have a background in psychology and take all that into account. The more perspectives, the better because you get more angles on an issue. Psychology looks more at individual factors and individual differences. In sociology, we are looking at this environment versus that environment, this group versus that group. When we see groups with a significantly different prevalence of anything related to health or behaviors, that is a tip-off that there might be something about that environment. It could be randomly. All of these people have mental health conditions, and they happen to work in healthcare. When it is that significant, we know something is up with that. Working conditions, placing others before yourself to the potential of personal detriment, and stigma are the top three reasons we might see more mental health issues in healthcare. This is at the group level. This is not to say that you have ever had any problems with mental health or burnout. It is not something that applies to every single person. We are thinking about this as a group.
The Covid Context
Within the COVID context, I have been studying these types of social and psychological determinants for about 20 years. There are decades and decades of research on society and health and the environment and health. What aspects of our culture relate to anxiety and stress, depression, inequality, and social injustice? The differences between groups on how much social power they have. I do not know if we had seen before how much this type of research was in the public eye looking at the television and seeing inequalities and health outcomes by race. I have never seen that before. It shed massive light on healthcare and working conditions. Now, healthcare professionals continue to work for the most part. Many other people had a break from work. They either lost their jobs, got laid off, there was a shutdown, they could not work, or they had to work from home. Everything was mixed up, and huge societal changes happened. If you look at it from the perspective of a social experiment where these massive changes in what we would call independent variables, like changing all these conditions and then looking at dependent variables, the outcomes, what were the outcomes in terms of people's health and happiness and physical health there were massive changes. While health professionals continued to work, others essentially had a break. I mean, they are completely taken out of their work environment. That is a perspective shift.
Meanwhile, we have folks in healthcare who had the pressure cooker increase, increase, and increase. Things like staffing issues, working long hours, not having enough breaks, the hierarchy, and the conflicts between different groups within healthcare. The stress of dealing with patients and families is likely going through one of the most stressful situations. Add on top of that this political context and the economic context. People do not have enough in their bank accounts for an emergency, then an emergency hits every single person at once, creating a shaky foundation in our communities and in our families. Then to show up at work and have all of these pressures and differences of opinion where identities are tied to health issues that affect respiratory therapists. It all culminates there. You are experiencing this stuff on the job, and it is the tip of the iceberg, but it is also the most dramatic manifestation when it is a life-or-death situation. Meanwhile, these issues are connected to patient and family interactions. I cannot imagine more external stress that could be exerted on a profession such as respiratory therapy.
The fact that you lived through that is phenomenal. Take into account that extreme stress, if you are doing great right now, is something where you might think about sharing what you did with other people if you could cope with it mentally, physically, emotionally, and socially. Most of us have some form of post-traumatic stress disorder (PTSD), which we are decompressing now. It is interesting, I have noticed that my students during COVID were in survival mode. It was figuring out Zoom, figuring everything out, and trying to survive. When it was not an emergency anymore, and it started to recede, They started freaking out about stuff, and it was like they finally had a chance to feel these feelings and emotions from what had happened. It is extreme stress. It is technically an opportunity to address some of these issues because they are not hidden under the surface. It is not something where you can say, "I have burnout." I mean, we all know that it is happening now.
Research on Healthcare Workers’ Mental Health During Covid
- In a survey of health professionals during the pandemic found that 42% of nurses had PTSD, 83% of EMS workers had depression symptoms and 24% thought about suicide or self harm
- Another survey found 93% of health care workers were experiencing stress, 86% reported experiencing anxiety, 77% reported frustration, 76% reported exhaustion and burnout, and 75% said they were overwhelmed
- Other themes including not getting enough emotional support (39%), emotional exhaustion (82%), questioning career path (55%) and compassion fatigue (52%)
Looking more into research on healthcare workers' mental health during COVID, 42% of nurses had PTSD, and 83% of EMS workers had depression symptoms. That is a huge percentage. These are clinical depression symptoms. About one in four thought about suicide or self-harm. If we treat this as "those people that may be crazy," it is impossible to pinpoint this on individual factors when we see such a common and very dramatic situation of this suicidality. Another survey found that 93% of healthcare workers were experiencing stress, and 86% were experiencing anxiety. Other themes included feeling like you do not have enough emotional support, emotional exhaustion, questioning your career path if any of you have done that, and compassion fatigue.
Survey Says
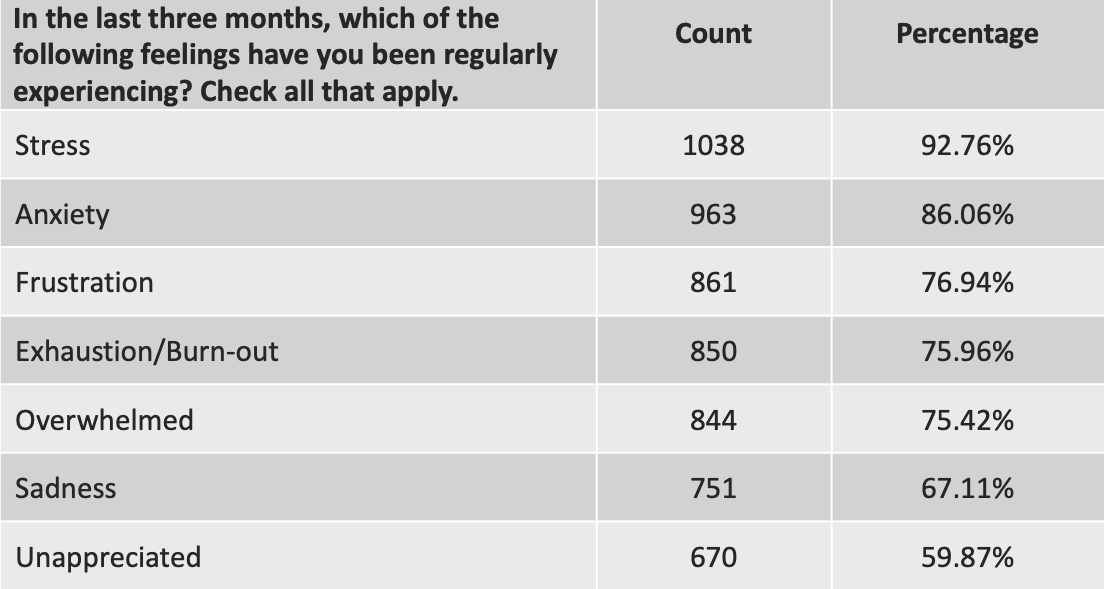
Figure 1. Survey topics.

Figure 2. Survey topics.
Here are some other topics investigated in this survey in Figures 1 and 2. How many people experienced this in the survey? Look at how high the percentages are. All of these symptoms that many people are experiencing. Anger and feeling disconnected were about half of the people. You are feeling disconnected. When people surround you, you are at work and go home. Maybe you live alone, maybe you live with your family, but half feel disconnected. We have to look at this. Why is this happening?
Respiratory Therapists’ Mental Health
Regarding respiratory therapists, some very interesting research on health professionals, in general, is focused on doctors and nurses. It is a little bit annoying that there is not as much on respiratory therapists and other professionals. A study was done in nine ICUs at five different hospitals and found that RTs had a lower burnout scale but still a high percentage compared to the other ICU workers. Burnout rates correlated highly with leadership, attitude, behavior, and work conditions. Right off the bat, if you have had a situation where you had this leadership and then a change in leadership, and I know from my experience, too, it is interesting how the attitudes of the people running things can affect them. It is like we are all in this Petri dish. Putting a toxin in the mix can affect how burnt out people get. It is interesting how affected we are by our environment and other people. The majority of this study worked more than 50 hours a week. Probably not a surprise to you all, and previous studies have reported a 25% severe burnout rate. It pretty much doubled during the pandemic.
Individual Factors
- Lack of self-esteem
- Lack of social support
- Poor work controls
- Baseline mental health
- Physical health
- Addictions and codependency
- Ability to express, identify, and cope with emotions
We are getting into the factors related to burnout and mental health issues—lack of self-esteem. We want to build this in our children and our girls. Self-esteem is not cockiness. It is not thinking that you are better than others. It is tough to pinpoint your self-esteem and where you are getting it from. A lack of social support is another factor. Linking it back to society as I often do, we are not trained or taught in our general education system about our emotions and how to identify them and express them. This is a huge gap in our education. You may have learned this and even learned this in school, but as a whole, this is something that we, unfortunately, are forced to figure out on our own, like many things interpersonally. Poor work controls and this is something that is been studied a lot. One of the most beneficial aspects of the working world is controlling your actions. When you are doing things, autonomy is huge. It affects your baseline mental health, physical health, and any addictions or codependency issues you may struggle with. The ability to express, identify, and cope with emotions.
Workplace Factors
- Feeling unsupported at work
- Demoralization • Leadership
- Misinformation or unclear protocols
- Community sentiments
- Facing death on a daily basis
- Job scope and time • Bureaucracy
- Organizational culture
- Relationships at work
Workplace factors probably are not a surprise, but feeling unsupported at work, not feeling appreciated, demoralization, the leadership, and misinformation were huge in the pandemic. Unclear protocols that are a little bit crazy in the making. When you are told to do one thing, and the community does not agree with it, the community sentiments create a lot of stress—facing death daily. Your job scope, having to go above and beyond, the time you have, and the breaks you have. Bureaucracy, if you want to make any changes, all the layers. Organizational culture. Is it a culture of do not complain and work hard? Is it a culture where there is a lot of gossiping? What are your relationships like at work? What are relationships like at work in general? Those are all factors related to burnout.
How Stressors Affect Health
- Stress vs. Stressors: the difference is important
- Stressors activate the stress response
- External stressors- work, finances, discrimination
- Internal stressors- body image, self-criticism, bad memories
- Stress is the physiological (and neurological) changes designed to help you survive
How stressors affect health, decoupling stress and stressors. Stressors are what activate the stress response. Work, finances, and discrimination on the internal level. Things like body image, self-criticism, and bad memories. Stress is the physiological and neurological stuff that happens designed to help you, but when it continues over time. It can wear down your physical body. Now, what is in our control? What is not in our control? If you can separate what is in and out of your control, you can start to take your energy back that may be tied up in something out of your control. When you are in the workplace, sometimes there is an illusion that you can change something that may have a lot of other factors and be difficult to change. On the other hand, you may think your thoughts are not in your control because you are having repetitive negative thoughts. By getting on board with this paradigm, at least you can start to manage your energy in potentially a different way, and this can be a long process.
The Stress Response
- Cytokine storm
- Inflammation response
- Heartbeat quickens, diminished sensitivity to pain, endorphins, epinephrine, digestion slows, immune function shifts
- If chronic, it is breaking down your body, making you vulnerable
Back to that physical stress response, cytokine storm that is happening, the inflammation response, your heartbeat, you have diminished pain sensitivity. Remember, it is designed to help you in dangerous situations, but if it is chronic, it breaks down your body and makes you vulnerable to other things. I am coming from the perspective of social and interpersonal situations as stressors, not physical ones. You have the stressor, the stress response, and then if you can deal with the stressor.
The Stress Cycle
In caveman times, if a lion is chasing you and you kill the lion, bring it back to the community and eat it for dinner, you complete that cycle. Animals do this when they get a shock or a trauma. They will often shake. There is an interesting video of a polar bear that gets shot with a dart, is traumatized, wakes up, and shakes. Animals will get that stress out of them, and then they will be good to go. Oftentimes we are not completing that cycle. For many of these, some of the stressors may not go away. You may not be able to "flight" or "fight." You cannot beat up your boss, and safety may prevent you from dealing with the stressor. As is the case, if you get into a dangerous situation with another person trying to harm you, you may be stuck and freeze.
Gender
- “One class of people, the “human givers,” are expected to offer their time, attention, affection, and bodies willingly, placidly, to the other class of people, the “human beings” (Philosopher Kate Manne)
Many social factors relate to this topic of stress response, and gender is a huge social factor. This is an interesting quote by a modern-day philosopher, Dr. Manne, who talks about how there are human givers and that females are expected to give, give and give. There are a lot of messages around doing things for ourselves. This applies to men and women and non-binary folks, it is not females, but it brings to light this issue of the idea of giving and some of the mental barriers we may have with truly addressing our well-being and what that means. I have not talked much about self-care yet, but we will get there.
Signs You Are Not Completing The Stress Cycle
Signs that you are not completing the stress cycle. Now, there is a book that I am currently reading called "Burnout." It is about this stress cycle, which is interesting because it focuses on how to discharge this stress. If you are not completing that cycle, these are some signs. You might be doing something over and over. You may have a burst of pain disproportionate to what happened. Like you are waiting in line at the post office, you lose it over something relatively minor. You could feel like your body is out of whack, something is not healing properly, you are hiding, you are isolating. Again, do not think this is how I am, and this is how my life is now. No, it could be that you have this stress build-up.
How Can We Complete The Cycle?
How can we complete the cycle? Positive social interaction is one way. Physical activity is another way. It does not have to be going on a run or going to the gym. It can be shaking. It can be dancing. That is hugely beneficial. It can be breathing, laughter, or affection if you do a 20-second hug. Your body is telling your brain that there is no threat because otherwise, you would not be in contact with this person for this long. That can help our physiology.
Coping with Stress
Drug and alcohol use
- Social isolation
- Overeating
- Procrastination
- Withdrawal
- Self-harm
- Aggression
Other ways to cope with stress are using drugs and alcohol. Socially isolating is many people's drug of choice. Overeating, procrastination, withdrawing from social activities, self-harm, and aggression. Looking at these things instead of saying they are bad habits but recognizing that these are ways that people are trying to cope with stress takes the moral issue out of it and looks at these signs of stress.
Addiction
Addictions are a huge part of our collective well-being in America. We have a lot of addiction. Some even say that we are an addicted society. You may not depend on drugs, alcohol, or smoking, but many people may be addicted to shopping, gambling, sex, food, and drugs. People have codependent behaviors. Addiction is doing the same thing over and over and not being able to stop if you want to, and it is starting to affect your life negatively, and you are still doing it. It is something that there is a big stigma around, like you are doing something stupid because you are doing something that is harming you over and over. Why would you do that? It is one of those things where you will have a different paradigm having experienced it versus not having experienced it. It is not to say that people cannot learn about how it works, but it is one of those things why 12-step programs are very powerful because you are in a room with people that have a similar situation where they may try to quit, not be able to, and there is a very strong dynamic going on psychologically and physiologically. Extreme stressors can accelerate the trajectory of addiction.
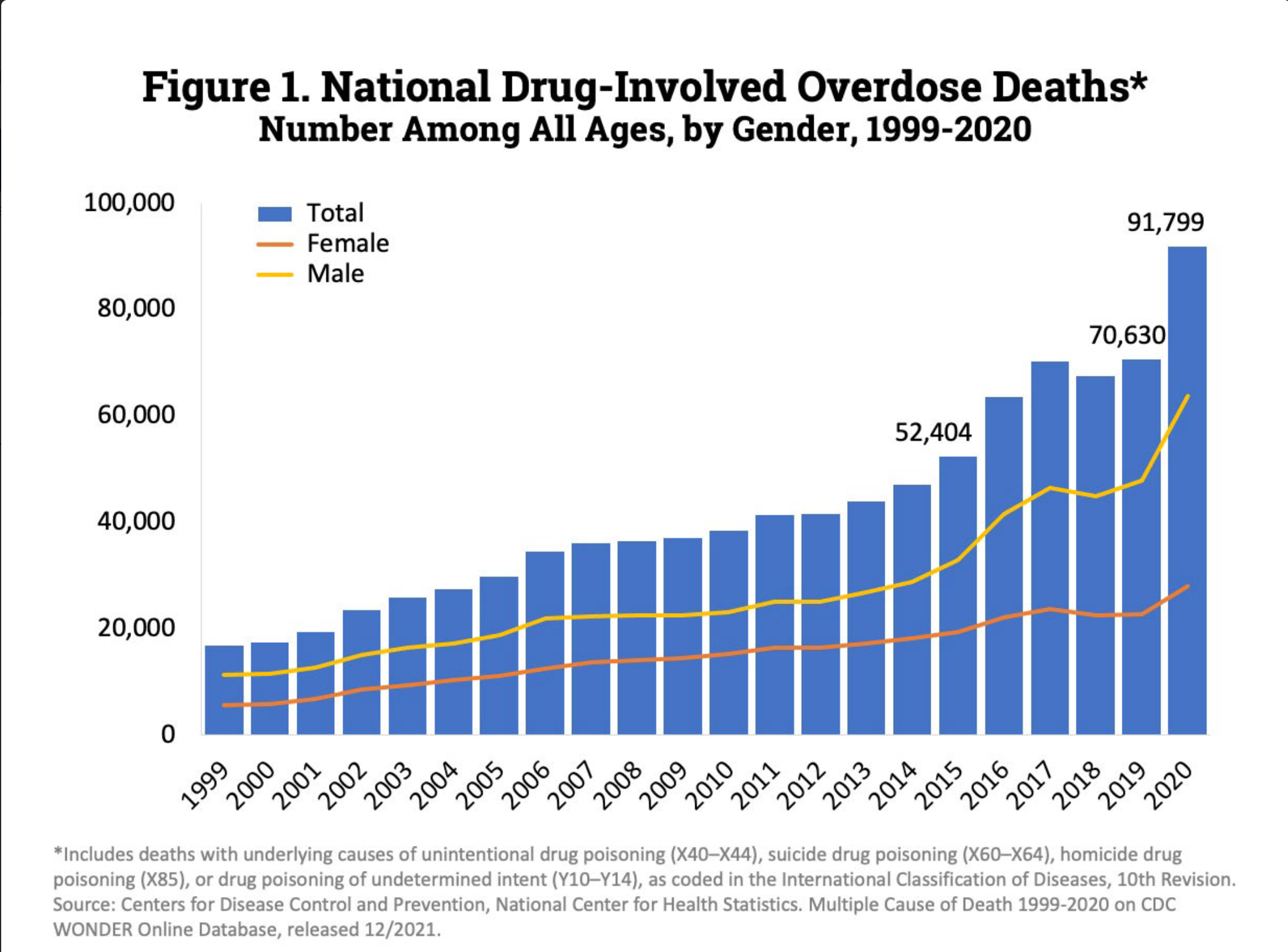
Figure 3. Graph of drug-related overdose deaths.
Figure 3 shows the trajectory of drug-related overdose deaths. You can see that it is been on an upward trajectory and the pandemic skyrocketed.
Codependency
Codependency is a pattern of behaviors. Within this topic of codependency, there are many, many, many patterns and behaviors. It is like a list of 200 things or something like that. Most of us can relate to at least one of them. It is that over-emphasis where your attention is overly focused on other people. That creates a situation where you may not know what you are feeling. You may be doing more than your fair share. You may have a hard time identifying what is going on with you or a hard time saying no to that thing. It can leave you feeling extremely burned out with an inability to create boundaries, and creating boundaries is another one of those things that we do not tend to learn in school.
Self Care: Critical ...& Not a Cure-all
Doing a self-assessment of your self-care routine, meaning what you are doing towards your health, is a good way to start addressing your well-being, and this can be tough. You know, and many times people say they do not have time for self-care, but it is not necessarily something you even have to dedicate time to. It could be something that focuses on the messages you are telling yourself. That does take awareness and potentially getting help from other people. Self-care is critical. It is very important. It is not a cure-all. We have organizational changes that need to happen societal changes that need to happen if we were to change the tide and start to reduce the prevalence of mental health as a whole. To do that, we would need better access to psychiatric treatment. That is an absolute must, including sick leave and outreach to people. We would have to emphasize a major emphasis on protecting workers' health, a necessary step. The basics are paying people a livable wage, addressing labor shortages, honest and transparent communication, and addressing racism and sexism. That is at the basic level of your workplace.
It is creating a workplace where people can be well there. Clear communication on safety measures from political and healthcare leaders would reduce health professionals' distress. it is a huge and complex problem, but I often say, because I am often asked, what is the solution to this? it is complex. The solutions are not... it is not rocket science. It is not trying to figure out what things would work. It is getting the powers that be to do these things. If you were paid a good wage and worked several hours that were reasonable for your physical and mental health, that would work. However, we have got lots of research to show that, but it does not always get done.
Covid-Time Interventions: Mental Health at Work
There have been some studies on COVID interventions regarding mental health but not a lot. There is very impactful peer mentorship. Doing online assessments, I mean, there are programs in other countries, but not a lot. There was a program in Italy that was the only program found in this study that looked at mental health and burnout from an occupational medicine perspective. As this is affecting healthcare delivery, we need to address it.
Relational Tools for the Workplace Toolbox
Regarding getting along better at work and relational tools, if you are into relationship dynamics and psychology, definitely check out Ester Perel. There was a book that I recently read about relational life therapy that was very interesting, almost like a pop psychologist that works with a lot of celebrities. It struck me that he kept driving home to the point that there is no objective reality when relating to people. Not that there is no objective reality, but getting into arguments where it is to be relational is tabling who's right and instead learning how to be relational more. It is about what works. No human is better or less than any human. This is the idea that if you are on track to thinking that you are better or worse, it is causing you emotional pain. The research has found that it takes skill to get along with people. It is not something that necessarily naturally happens.
Workplace Strategies to Protect Mental Heath
Regarding what can be done in the workplace, these are tips according to the literature. First off, accepting that people cope in different ways. It is respecting the importance of emotional well-being. This is tough. When people are emotional, it is not normal to show emotions. How are they received? Are people saying, "Oh my gosh, get me away from this person." What is the culture around that is an important part of health? Attend to other aspects of health holistically. Peer mentorships are great outreach calls, calling people, and checking in. Suppose you have a spiritual practice, inspiring quotes. Yes, it can seem corny, but on the other hand, having that mentality to go about your day can change how you interpret things cognitively if your perspective is changed. It changes how your body interprets it and reacts to it physiologically. I am not saying it is easy to change your perspective, but I am saying that if you can get that perspective shift, it is hugely impactful. It is not a mental thing, and it is a physical thing as well.
Healing & Prevention: Organizational Level
At the organizational level, if we were to have the goal to reduce burnout and improve the conditions for better mental health. We want to manage workload, give people autonomy, reward and recognize people, be fair, have shared values, have a purpose above and beyond generating revenue, and have a sense of community and belonging.
For Leaders
For leaders, there is a significant effect on many aspects of work life—your leadership style. There is a thing now called a chief wellness officer, and some places have one. They are identifying what employees want. There is much in the media about a ping pong table at work or a gym membership discount. That may be what people want at a certain organization, but some basic things people want are a managed workload. They want to get paid what they are worth. They want childcare. They want healthcare. That is what people want in general. All these extra things, not to say they do not do anything, but the important thing here is taking this step to identify what people want is a great way to be more effective in whatever initiative you are starting to improve mental health and reduce burnout—having humility, empathy, servant leadership, inclusive environments, and nurturing environments versus focusing on the problem. The problem is how we can alter our working conditions to improve well-being.
Healing & Prevention: Individual Level
At the individual level, self-care is finally up here. This is your basic, your sleep, your eating, your stress level, wellness, physical activity, mindfulness, meaning being able to self-soothe. Having a spiritual perspective is helpful for many people. You have social support and mental healthcare. What is the harm if you can access a counselor to check in? Only you know.
Emotional Regulation & Expression
Emotional regulation is also critical. I mentioned identifying emotions. For many of us, this is difficult, but it is learnable and teachable. That mindfulness aspect is being able to train yourself to be less reactive and to give yourself time. Also, more practically, we often feel like we have to get back to people immediately. I know there are certain work situations where you have to respond very quickly, but there are other situations where you do not have to respond very quickly. You can take 24 hours. It is a tool that has helped me a lot. I do not have to respond right away to everything. That will allow me to figure out where I am and how to communicate it—checking in, journaling, doing art activities, singing, yelling, and staying connected. This is tough, being vulnerable and developing connections where you have emotional intimacy—staying connected when you may want to isolate due to shame if you feel certain emotions.
The Feels
The feels are also out of the "Burnout" book. It is a common catchphrase in the new generation tool of the feels. This is the idea that you may have an outburst of emotion or be feeling an emotion. Next time you feel a very strong emotion connected to the situation, consider that the situation may be there to bring the emotion out of you. There is a lot of research on emotions trapped in the body that they are looking for a reason to come out. That goes back to the stress cycle and flushing that out of your system so that you do not have chronic stress, a chronic buildup of emotions. You may need to do something related to the situation, but it might be about being irritated, frustrated, anxious, or shut down. Releasing emotion is part of completing the stress cycle, which is a good thing.
Being Your Own Caregiver...
Now on this practical level, I developed some questions to get you started thinking about being your caregiver. This was a different way to phrase it. Self-care is used much, and I feel like there are a lot of associations our brains make with that. To table that concept and think about the caregiving aspect of it, how would you rate your physical, mental, emotional, and social health? What areas do you receive external validation in? Do you need that external validation? Who are you without your work identity and your family identities? Do you often say yes when you want to say no? How often are you bothered by somebody else's behavior? What is your go-to strategy when you are stressed? How do you know when you are stressed? What are you feeling right now? How do you feel right now? Not everybody can answer that. It is tough. What activity did you use to love but do not do anymore? This often comes up with people I work with who are high achievers. They need to do all these things, and sometimes they have things that used to help them that they do not do anymore. They do not think they have time, but then they may spend time doing something else, like obsessing over something. Is there a substance or a behavior that you have wanted to quit but have not been able to? Those are check-in questions.
Book Club Reading List
This is an idea to throw out there, having a book club. I know many people do not have time, but it is an interesting way to discuss mental health and burnout and share personal experiences without blurting them out. It can be a container to connect with people and share, and there is a container for that—a couple of book recommendations. There are many things that I want to share with you, but I appreciate your time and attention and your service to yourself and others. I am super grateful to be here with you. I am also grateful to have gone through this burnout process and have my mental health issues for which I have gotten treatment to get to the point of sharing and digesting everything that has happened to me. The research integrates all of that. I am very grateful for that.
Questions and Answers
I love how you provided some great examples of strategies and how to change that perspective shift to help with burnout and healing because you nailed it when it is not something that happens overnight. it is something that you have to think about where to start, how to get started, and then slowly progress and work on yourself.
It is a very long process, but changes happen, and I think that one thing I like to repeat is that it is not like you are like this forever. You can heal from it. As you said, it is not overnight, and for a lot of this, it does involve working with others. it is not something that is purely a self-help thing. Making those connections with people is a critical part of the recipe.
I have not worked for several months, which has been an ongoing battle. How can we overcome this?
Thanks for sharing that. You bring up an important point that removing yourself from a stressful situation does not heal you. It is like in the addiction sciences. Getting sober does not fix all of your problems. You are taking away the stressor, but you still have that stress to deal with and potentially PTSD, potentially mental health issues. Being able to do that self-assessment and take a step to explore different resources, get over that stigma. What is the harm in getting resources? That can be a big part of it. Thank you for sharing that.
References
Burghi, G., Lambert, J., Chaize, M., Goinheix, K., Quiroga, C., Fariña, G., ... & Azoulay, E. (2014). Prevalence, risk factors and consequences of severe burnout syndrome in ICU. Intensive care medicine, 40(11), 1785.
Chivato Pérez T, Campos Andreu A, Negro Alvarez JM, Caballero Martínez F. Professional burnout and work satisfaction in spanish allergists: analysis of working conditions in the specialty. J Investig Allergol Clin Immunol. 2011;21(1):13–21
Greenberg, N., Weston, D., Hall, C., Caulfield, T., Williamson, V., & Fong, K. (2021). Mental health of staff working in intensive care during Covid-19. Occupational Medicine, 71(2), 62-67.
Guntupalli KK, Fromm REJr. Burnout in the internist--intensivist. Intensive Care Med. 1996 Jul;22(7):625-630. doi: 10.1007/ BF01709737. PMID: 8844225
Hendrickson, R. C., Slevin, R. A., Hoerster, K. D., Chang, B. P., Sano, E., McCall, C. A., ... & Raskind, M. A. (2022). The impact of the COVID-19 pandemic on mental health, occupational functioning, and professional retention among health care workers and first responders. Journal of general internal medicine, 37(2), 397-408.
Holmes, E. A., O'Connor, R. C., Perry, V. H., Tracey, I., Wessely, S., Arseneault, L., ... & Bullmore, E. (2020). Multidisciplinary research priorities for the COVID-19 pandemic: a call for action for mental health science. The Lancet Psychiatry, 7(6), 547-560.
Mental Health America, “The Mental Health of Healthcare Workers in Covid-19”, https://mhanational.org/mental-health-healthcare- workers-covid-19
Murat, M., Köse, S., & Savaşer, S. (2021). Determination of stress, depression and burnout levels of front-line nurses during the COVID-19 pandemic. International journal of mental health nursing, 30(2), 533-543.
National Insittuite for Occupational Safety and Health, Centers for Disease Control and Prevention;
https://www.cdc.gov/niosh/topics/healthcare/workstress.html
Omar, A. S., Hanoura, S., Labib, A., Kaddoura, R., Rahhal, A., Al-Zubi, M. M., ... & Alumlla, A. (2022). Burnout among Respiratory Therapists and Perception of Leadership: A Cross Sectional Survey Over Eight Intensive Care Units. Journal of Intensive Care Medicine, 08850666221086208.
O'Kelly, F., Manecksha, R. P., Quinlan, D. M., Reid, A., Joyce, A., O'Flynn, K., ... & Thornhill, J. A. (2016). Rates of self-reported ‘burnout’and causative factors amongst urologists in Ireland and the UK: a comparative cross-sectional study. BJU international, 117(2), 363-372.
Pedersen, A. F., Andersen, C. M., Olesen, F., & Vedsted, P. (2013). Risk of burnout in Danish GPs and exploration of factors associated with development of burnout: a two-wave panel study. International journal of family medicine, 2013.
Pilgrim, J. L., Dorward, R., & Drummer, O. H. (2017). Drug-caused deaths in Australian medical practitioners and health-care professionals. Addiction, 112(3), 486-493.
Citation
Nathenson, S. (2022). Burned out: how to heal and protect our mental health at work. Continued.com - Respiratory Therapy, Article 161. Available at www.continued.com/respiratory-therapy
