Editor’s note: This text-based course is a transcript of the webinar, Anaphylaxis Management: More than Just an Epi-Pen!, presented by Nancy Nathenson, BS, RRT.
Learning Outcomes
- After this course, participants will be able to:
- identify individuals at risk for anaphylaxis.
- recognize anaphylaxis symptoms and those that are a precursor to upper airway obstruction.
- explain the key components in the diagnosis and management of food allergies.
- describe anaphylaxis symptom progressions and the first line of treatment.
Introduction
I am delighted to be with you and be part of the Continued Education Team and present to my RT colleagues. As we progress through the presentation, I think you will all see that there is much to do, consider, and be mindful of as we try to manage anaphylactic reactions.
What is Anaphylaxis?
- Anaphylaxis is a sudden, severe, potentially fatal systemic allergic reaction that can involve various areas of the body
What is anaphylaxis? Anaphylaxis is a sudden, severe, and potentially fatal systemic reaction involving various body areas, as noted in Figure 1.
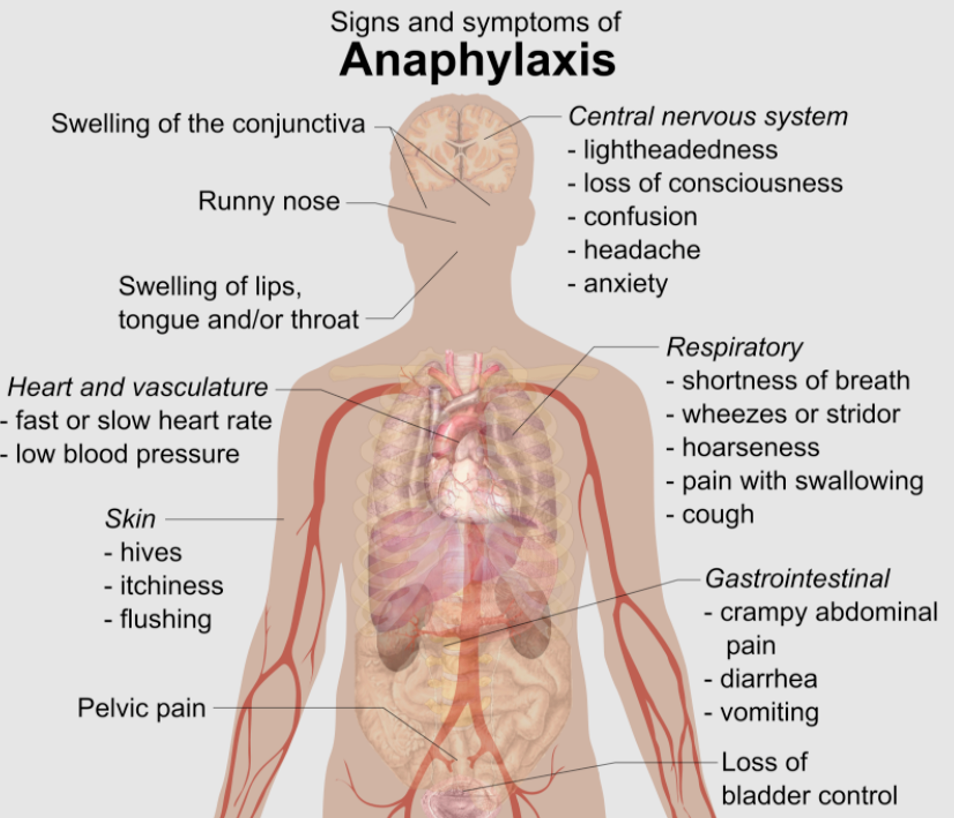
Figure 1. Signs and symptoms of anaphylaxis (Mikael Häggström, CC0, via Wikimedia Commons).
The skin, heart, stomach, mouth, and lungs can be involved in an anaphylactic reaction.
Anaphylaxis Symptoms
- Skin:
- Itching, redness, swelling
- Mouth:
- Itching, swelling lips, tongue, metallic taste
- Stomach:
- Vomiting, diarrhea, cramping
- Lungs:
- SOB, wheezing, coughing, chest pain
- Heart:
- Weak pulse, dizziness, faintness
- Headache
- Nasal congestion
- Watery eyes
- Sweating
- Confusion
- Impending doom
- Loss of consciousness
The one area of the body that is most concerning is the mouth. Anytime there is itching or swelling of the lips, and the tongue or a metallic taste noticed in the tongue or the mouth, there is a possibility of airway obstruction. Be very mindful of those symptoms. Not everyone will experience some other symptoms, like a rash or swelling of the eyes, watery eyes, and shortness of breath or wheezing. Again, be very mindful of the mouth symptoms as this is potentially very serious.
Patients at Risk
- Prior history of anaphylaxis
- Asthma
- Food allergies
- Pollen/food allergies
**Patients/parents who do not perceive the above as risk factors**
The patients at risk are the ones that have had a prior history of anaphylaxis, asthma, food allergies, and those with both pollen and food allergies. An additional risk is when parents and patients do not perceive that the above are risk factors. This can be tough when you have a parent or a patient that are in denial that this type of situation or condition exists.
Anaphylaxis Categories
- Food allergies
- Insect/bee/wasp stings
- Exercise-induced Anaphylaxis
- Latex
- Medications
The categories of anaphylaxis are food allergies, insect, bee, wasp stings, exercise-induced anaphylaxis, latex, and medications. It turns out that only about 20% of cases of anaphylaxis have skin manifestations. Also, children have a greater incidence of food-related anaphylaxis. There is a greater incidence of reactions to antibiotics, anesthesia agents, contrast media, and insect stings in adults.
Statistics
When we are talking about anaphylaxis, it is good to know the statistics in the United States, as noted in Figure 2.
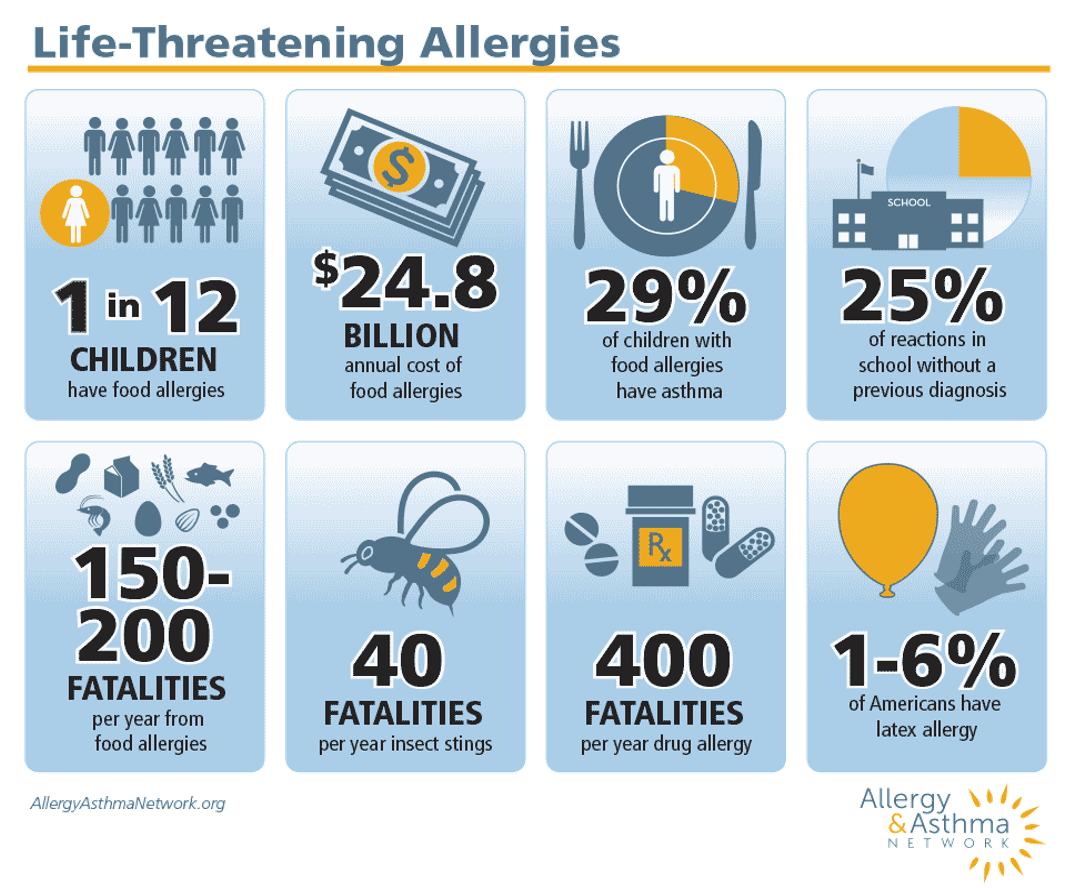
Figure 2. Statistics on life-threatening allergies (from the Allergy & Asthma Network).
One in 12 children has a food allergy. It costs 24.8 billion annually to manage that. Additionally, 29% of children with food allergies have asthma. Twenty-five percent of reactions in school occur without a previous diagnosis. It is essential for communities to be aware of and to use their voice to legislate for having Epi-Pens available in all schools regardless of if they have individuals with prior anaphylactic reactions or not. Per year in the U.S., there are 150 to 200 fatalities from food allergies, 40 fatalities for insect stings, and 400 fatalities from drug allergies. Lastly, 1-6% of Americans have a latex allergy.
Anaphylaxis or Asthma?
- Individuals with asthma are at greater risk for anaphylaxis
- Combine asthma with food allergies
- Difficult to identify the cause
- Confusion can cause a delay in proper treatment
- With the sudden onset of asthma symptoms after food ingestion, use Epi-Pen
What happens when you have anaphylaxis and asthma together? Individuals with asthma are at greater risk for anaphylaxis, as I mentioned. When you combine asthma with food allergy, sometimes it is difficult to identify the true cause. This confusion can delay the proper treatment, like an Epinephrine pen. After food is ingested with a sudden onset of asthma symptoms, always reach for an Epinephrine auto-injector.
Case One
- A 37 y/o male w/ long history of allergic rhinitis and mild intermittent asthma; develops acute urticaria and shortness of breath 30 minutes after eating pecans.
- The patient was treated in the ER w/ an albuterol inhalation and 50 mg of Benadryl® IM. Symptoms resolved within 90 minutes
Here is a case study. This is a 37-year-old male with a long history of allergic rhinitis and mild intermittent asthma. He developed acute urticaria or rash and shortness of breath 30 minutes after eating pecans. The patient was treated in the emergency room with an albuterol inhalation and 50 milligrams of intramuscular Benadryl. His symptoms resolved within 90 minutes. He was okay after about an hour and a half.
Was this patient treated appropriately in your view? Yes or no? The answer is no; he was not. Any time allergic reactions occur in an asthmatic patient after eating food, you want to use an Epi-Pen immediately.
Idiopathic Anaphylaxis
- Testing:
- A variety of foods
- Skin tests, Blood tests
- Underlying diseases that mimic anaphylaxis
- Treatment:
- 6 episodes or > /year- Daily antihistamines or short course oral corticosteroids
- <5 episodes/year-No daily medications
Idiopathic anaphylaxis is when the cause of a reaction is not obvious or apparent. It can sometimes take a while to drill down and determine what is causing these anaphylactic reactions in individuals. If there is a reaction, the individual needs to document all foods, meds, and drinks. Documenting these areas is very important to determine the cause of a reaction. This documentation should include a detailed list of the ingredients in the food consumed, the symptoms, and when they occurred. These should also be shared with an allergist. Allergy testing may take several visits.
When you test for idiopathic anaphylaxis, it is much like testing for food allergies. You might do skin prick testing or blood tests. You would check for underlying diseases that mimic anaphylaxis. These conditions are things like generalized rashes or urticaria and acute angioedema, which is acute swelling of the skin's subcutaneous tissue. As an example, asthma exacerbations can mimic anaphylaxis based on the symptoms and the struggle to breathe. Additionally, syncope or fainting can also mimic anaphylaxis and panic attacks. Keep that in mind.
For individuals with anaphylactic episodes, six episodes or greater per year, the doctor may prescribe daily antihistamines or a short course of oral corticosteroids. Individuals that have less than five episodes per year may not be on any daily medications. However, this is going to depend on what types of reactions they have had in the past.
Top 8 Food Allergens (Sesame?)
Here are the top eight food allergens right now in the United States.
- Tree nuts
- Peanuts
- Eggs
- Fish
- Dairy
- Wheat
- Soy
- Shellfish
They are tree nuts, peanuts, eggs, fish, dairy, wheat, soy, and shellfish. Sesame might be the ninth food allergen because it has been on the rise in the United States. You can find sesame in foods like Asian, Middle Eastern, and Indian cuisine. It is also found in hummus, granola bars, salad dressing, and even hamburger buns.
Red Meat Allergy
- Causes:
- Triggered mostly Beef, Pork, and Lamb
- Also called “alpha-gal”
- Associated with tick bites
- Hunters and gardeners at > risk
- Itching, hives cramping, heartburn, diarrhea after eating
- Anaphylaxis
- Dx: Blood Testing
- Not life long
There is a red meat allergy, but it is not very common and quite rare. It is triggered by mostly beef, pork, and lamb. It is also called alpha-gal because of the blood carbohydrate called alpha-gal associated with tick bites. You can imagine that hunters and gardeners are at greater risk because they are exposed more often to ticks. The symptoms are itching, particularly the hands and the feet, hives, cramping, heartburn, and diarrhea after eating. Of course, anaphylaxis is the worst symptom of all.
It is diagnosed with blood testing to assess the IgE levels. The good news is that a red meat allergy is not a lifelong condition and typically disappears within a couple of years. With a red meat allergy and any type of anaphylactic reaction, an Epi-Pen is a proper treatment. And, you always want to carry two Epi-Pens. We will talk about why that is important a little bit later.
Diagnosing Food Allergies
- Start with a diary
- Food allergy testing
- Skin prick testing
- Stable vs. Unstable proteins
- Blood testing
- IgE antibodies
- Oral food challenge test
- Most accurate
How do we diagnose food allergies? We can start with documentation and a diary. Food allergy testing and skin prick testing most likely would be the next steps. With this, we can test for stable or unstable proteins. Blood testing may be the test of choice for some individuals to check for the IgE antibodies. Individuals with skin conditions or even medication interference with skin prick testing might opt for the blood test. There are also real food challenge tests and are the most accurate. However, you should never do an oral food challenge test at home.
Allergy Testing Key Points
- No one-size-fits-all
- Immune system changes
- Repeat testing
- Move locations
- New symptoms
- New allergens
What are the key points when testing for allergies? There is no one-size-fits-all approach, and no particular test is perfect for each individual. There can be immune system changes. When those occur, the individual would want to proceed with allergy testing. They would also want to repeat testing when moving locations. This makes sense because they are exposing themselves to a different environment with new allergens. An example would be new cuisines in a different geographic location.
Managing Food Allergies
- Keep a food diary
- Allergy Testing
- Skin
- Blood
- Oral food challenges
- Written Anaphylaxis Emergency Plan
How do we manage food allergies? These are the key components of managing food allergies: keep a food diary, allergy testing (skin or blood), and oral food challenges. A written Anaphylaxis Emergency Plan is also integral. These are like the asthma action plans. These plans can be very comforting for the individuals and caregivers for what to do in certain situations.
Conquering Anxiety with Anaphylaxis
- Make a plan
- Investigate
- Reassure and Repeat
- “We carry our Epi-Pens everywhere, every day and are prepared to use them right away”
- Keep calm
- Think outside the box
- Seek help from professionals
- Empower and Build Confidence
Anxiety is a big problem, especially from a parent with a child exhibiting food allergy symptoms. First, they need to make an Anaphylaxis Action Plan (more details below) with the medical provider and share it with the school, coaches, family, whoever the child will be visiting, et cetera.
We also need to investigate how it went with the child from that perspective. How did it go today at school? What went well, and what did not go well? We need to reassure and repeat the important aspects of managing a food allergy. This quote is perfect for sharing with a child, "We carry our Epi-Pens everywhere, every day, and we are prepared to use them right away." This is a mantra that they need to repeat.
We also want them to keep calm. Parents can be controlling when they are worried about a child going to a friend's house or for a play date. It may be best not to remind the child of all they need to do and watch for when they are at their friend's house. Instead, they should contact the parent and talk to them first about the child's needs are.
Think outside the box. What are some alternatives for food rather than food? What can you do to celebrate in a classroom? They can talk to the teachers and see what they have to say. They can also seek help from professionals.
Sometimes coping with a food allergy is very difficult. It is not just difficult for the child, but it is difficult for the parent as well. Encourage them to seek mental health help when they need it.
Lastly, when we empower our children to understand their condition and take some charge, they will build their confidence. For example, when the child goes to the grocery store, they can read the labels to see what ingredients are in the particular food. This is one way to engage them in the process of managing the anaphylaxis response and allergies.
Allergy and Anaphylaxis Emergency Plan
- Allergies
- Symptoms of a reaction
- Emergency interventions
- How to administer meds
- Who to contact
The Allergy and Anaphylaxis Emergency Plan lists the allergies, symptoms, and emergency interventions. It will also detail how to administer the medications and who to contact. The other thing that is very important about this plan is that it will detail if the individual has had an anaphylaxis reaction in the past. This form also states whether the person can carry their medication with them and whether they can self-administer it. You can view the American Academy of Pediatrics Allergy and Anaphylaxis Emergency Plan here (also available through www.aap.org); it has all the key components mentioned previously.
Bullying
Bully Zone
- 30% of children and teens report being bullied
- Up to 50% in grades 6-10 (Jaffe Food Allergy Institute at Mount Sinai School of Medicine in NYC)
- Harms children’s social development and self-esteem
- Linked to underperformance in school, depression, and chronic stress
- Verbal abuse vs. Intentional Exposure (Ralph Cash, PhD)
Kids often bully each other for a variety of different reasons. Food allergies can be one of them. Up to 30% of children and teens report being bullied (Boston Children's Hospital), and up to 50% in grades six through 10 (Jaffe Food Allergy Institute). Bullying harms children's social development and their self-esteem when they are bullied for this reason. It is also linked to underperformance in school, depression, and chronic stress. There is verbal abuse in the case of bullying for allergies, but sometimes children intentionally expose a child to that irritant or that allergen.
No Bully Zone
- Good to Talk
- Check-in on lunchtime
- Did good or bad things happen at school?
- Practice responses
- See the Signs
- Many kids do not report bullying
- Reluctance or fear
- Unexplained depression/anxiety
- Changes in sleep patterns
- Weight Loss
- Full lunch box brought home from school (Jennifer LeBovidge, PhD)
What can parents do? It is good to talk with the child and check in on what happened at lunch. Most parents would say that when they tuck their kids into bed at night, they open up. This is when they might be more willing to share. They can also practice responses with their child at this time. For example, the child's friend might have said, "I'm having ice cream, and don't you wish you could have ice cream too?" The response could be, "Why would I want to eat something that's going to make me sick?"
Parents need to see the signs as many kids do not report bullying. They may not report it as they are embarrassed or fear retaliation. They also feel like they can handle it in some cases. Parents might see a reluctance or fear of the child of going to school, going to activities, or playing on a team. They may see unexplained depression or anxiety, changes in sleep patterns, or weight loss. The child may also bring their lunch home from school every day because they do not want to eat it when everyone else is having a school lunch.
Peanut Allergies
Peanut Free Equal Certainty? (Matthew Greenhawt, MD)
- Peanut Free policies may not be effective in preventing reactions
- 2008 study Univ. of Michigan nearly 20% of reactions occurred in a nut-free zone
- Residue easily cleaned
- Smelling peanut butter does not cause allergic reactions
- Peanut dust does not become airborne but may accumulate on surfaces (The Journal of Allergy and Clinical Immunology)
- Optimize proven strategies
- Examples: Hand/mouth washing, no sharing increase awareness of child’s restrictions
Matthew Greenhawt is an associate professor of pediatrics and pediatric allergist. He contributed to the "Understanding Anaphylaxis" magazine from the Allergy & Asthma Network. He shares that peanut-free policies may not be effective in preventing reactions. In a 2008 study at the University of Michigan, he noted that nearly 20% of reactions occurred in a nut-free zone. The residue of peanuts can be easily cleaned. He also shared that smelling peanut butter does not cause an allergic response. Peanut dust does not become airborne, but it can accumulate on surfaces. This is why it is important to keep those surfaces clean. He suggests that you optimize the proven strategies of hand and mouth washing and no sharing to increase the awareness of a child's restrictions. They also found that peanut allergies are misunderstood. People that have children that are not allergic feel like the rules are unfair, causing some pushback.
Avoiding Accidental Exposure (Michael Pistiner, MD)
- Goal-prevent severe allergic reactions
- “Peanut Free”
- This designation can decrease vigilance
- Training
- Identifying reactions
- Use of Epinephrine auto-injectors
- Challenges
- Preventing cross-contact
- Preschool/kindergarten vs. older students
- “Peanut Free”
How do we avoid accidental exposure? Michael Pistiner is the Pediatric Allergist and Director of Food Allergy Advocacy, Education, and Prevention for the Food Allergy Center at Mass General Hospital for Children. He says that the goal is to prevent severe allergic reactions. He also states that peanut-free zones can decrease vigilance. If you have an area designated peanut-free, sometimes people can be lax about managing that area.
He suggests that training for cafeteria workers and teachers be trained on identifying reactions and using Epinephrine auto-injectors.
There are challenges with preventing cross-contact and younger versus older students. When you try to prevent cross-contact, this might be harder to contain and keep a multipurpose area clean in a preschool. With older students, this is easier as they are in a cafeteria setting.
2006: Food Allergen Labeling and Consumer Protection Act
- Mandates clearly stated the presence of food containing Top 8 allergens
- Spice, food flavoring, coloring, processing containing Top 8 allergens
- It does not apply to meat, poultry, or some egg products
- Not required to list highly refined peanut, tree nut, or soy oils
In 2006, the Food Allergen Labeling and Consumer Protection Act was passed. It mandates that foods clearly state the presence of the top eight allergens that we discussed earlier. These can also be present in spices, food flavoring and coloring, and processing. These allergens need to be stated on those types of foods. This does not apply to poultry, or meat, or some egg products as it is not necessary. Foods are also not required to list highly refined peanut, tree nut, or soy oils. Another thing to note is that clams, oysters, mussels, scallops are not considered a major food allergen.
Reading a Food Label
- Look for “Contains”
- Avoid foods with:
- “May contain”
- “Produced in a facility that”
- “Manufactured on shared equipment with”
- Food manufacturers can change ingredients without notice
- If your unsure, do not buy or check with the manufacturer
You want to look for keywords when you are reading a food label, as in Figure 3.

Figure 3. Example of a food label.
An individual needs to look for the word "contains" (and what that states), "may contain this," and "produced in a facility that" manufactured or shared equipment with a certain allergen. These are red flags. They will need to look deeper into that and may want to avoid that product. It is important to note that food manufacturers can change ingredients without notice. If a person is unsure, they should not buy the product or check with the manufacturer.
What is in a Name?
- Dairy
- Casein
- Curds
- Ghee
- Whey
- Egg
- Albumin
- Lysozyme
- Meringue
- Peanut
- Cold-pressed peanut oil
- Legumes
- Nougat
- Marzipan
- Sesame
- Cenne
- Tahini
- Sesamol
- Sim Sim
- Soy
- Miso
- Tamari
- Tempeh
- Toya
- Wheat
- Farro
- Malt
- Spelt
- Graham flour
This makes me think of Shakespeare, "A rose by any other name would smell as sweet." If we insert dairy, egg, or peanut in that statement, dairy by any other name could be a problematic allergen. Above are some of the names under these categories of foods. There is a multitude of names for the general categories of the top food allergens.
Dining Out/Cross Contact
- Call the restaurant
- Create a reference card
- Read menus
- Ask about ingredients
Let's look at some tips for dining out. Before going out, it is important to call the restaurant ahead of time and create a reference card for that individual. You definitely want to read the menu beforehand and ask about ingredients. Many waitstaff, chefs, restaurateurs are used to having questions about the food that they prepare.
- Wash hands
- A separate shelf in the fridge
- Never share utensils or drinks
- Avoid buffets or cafeterias
- **When a Kiss Is Not Just a Kiss**
Again, cross-contact is when an allergen is in contact with foods that are safe for a person. It is important to wash hands and keep a separate shelf in the fridge to prevent cross-contact from an allergen. It is also important to never share utensils or drinks and avoid buffets and cafeterias. There are times when a kiss is not just a kiss. An individual may need to brush their teeth or rinse their mouth because allergens can stay within the saliva for hours after.
Travel Safe
- Call the airline or visit the website
- Inform flight crew
- Wipe down trays and seats
- Bring something to cover your seat
- Bring your own food
- Carry your Epi-Pens onboard
- Print out the airlines published food allergy policy
How do we travel safely? It is important to call the airline or visit the website prior. Websites will often have categories or areas for special travel needs. Other things that can be done are informing the flight crew, wiping down trays and seats, bringing something to cover the seat, and bringing your own food. Again, it is vital always to carry an Epi-Pens onboard. Do not put them in the checked baggage or the overhead compartment. One can also print out the airline's published food allergy policy to have when boarding the flight.
Insect Stings
- Yellow Jacket
- Paper Wasp
- Hornet
- Bees (Bumble & Honey)
- Fire Ant
Insect stings can be very problematic for a lot of people. There are many different culprits, as seen in Figure 4.
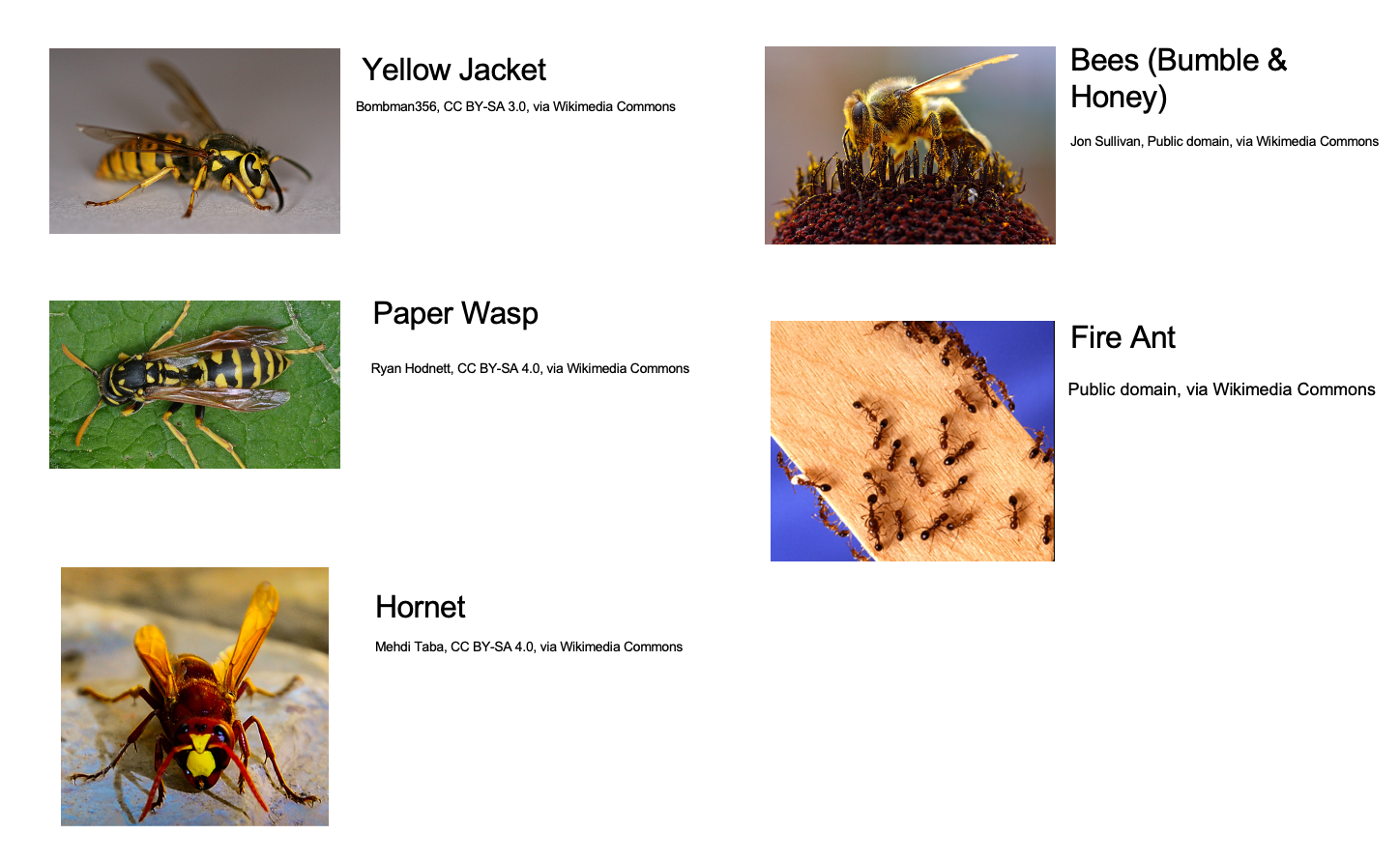
Figure 4. Types of insects that sting.
Yellow jackets are the pesky little critters that surround picnic tables and trash cans in the summer. Paper wasps are long and slim. They have nests that look like upside-down umbrellas that can be as big as a football. Bees, bumblebee, and honeybees are the ones that are going to be just hovering over flowers, clover, and things of that nature. Fire ants can be black or red. They are housed in huge domes of crumbled earth. You may not see a single ant there, but I guarantee you will be surrounded and covered with ants if you step on that.
- FLICK the insect away from the skin
- WALK don’t run
- SCRAPE stinger off with a flat surface
- ICE
- EXPECT Redness and swelling
- LOCAL vs. SYSTEMIC reaction
What do you do if you get an insect sting? First of all, you are going to flick it away from your skin. Then, walk (do not run) to find something to scrape the stinger off using a flat surface like a credit card. Do not use your fingernails or tweezers. Ice can help with a local reaction like redness, warmth, and swelling. Keep an eye out for a more systemic reaction like a rash, trouble breathing, stomach issues, dizziness, and those types of things.
Venom Immunotherapy
- David Golden, MD Johns Hopkins
- 100% protected
- 85% cured
- ID the insect
- Injections once/week 8-20 wks
- Remain in the office 20-30 min
- No strenuous exercise for several hours
- Booster shots Q1-2 month
- In 5 years, complete protection
There is hope on the horizon for venom immunotherapy, and there has been for some time now. Dr. David Golden from Johns Hopkins has developed this. Approximately 85% of the individuals that undergo immunotherapy are cured of the problem. First, the insect is identified. Then, an injection of the venom occurs once per week for eight to 20 weeks. You remain in the office for about 20 or 30 minutes after to watch for any signs of an anaphylactic reaction. There is also no strenuous exercise for several hours after. There are also booster shots, one every one to two months, and then five years for complete protection. This is great news.
Case Two
- A 16 y/o male was stung by a bee and suffered acute urticaria, shortness of breath, and dizziness
- After ER treatment w/ Epinephrine, cortisone and oxygen, he was given a prescription for two (two-pack) Epinephrine auto-injectors
- The patient’s mom gave one to her son to carry, left one at school, kept one in her purse and one at home, thinking if her son was stung, he'd be protected against a fatal anaphylactic reaction
Here is our second case study. We have a 16-year-old male stung by a bee and suffered acute urticaria, shortness of breath, and dizziness. After an emergency room treatment with Epinephrine, cortisone, and oxygen, he was given a prescription for two two-pack Epinephrine auto-injectors. The patient's mom gave one to her son to carry, left one at school, kept one in her purse and one at home, thinking if her son were stung, he would be protected against a fatal anaphylactic reaction. Is she right in this case? Yes or no? Well, the answer is no. we need to always have two Epinephrine auto-injectors with us at all times, and we will talk more about why a little later.
Components of Pollen Food Allergy Syndrome (PFAS)
- A history of symptoms consistent with PFAS
- Allergic sensitization to pollen
- Allergic sensitization to a plant food
- A known correlation between the plant food and the pollen
Now, we get into the Pollen Food Allergy Syndrome or PFAS. This occurs when a person has a history of symptoms consistent with PFAS and allergic sensitization to pollen and plant food. This is a known correlation between that plant food and that pollen.
Pollen Food Allergy Syndrome (PFAS)/Oral Allergy Syndrome (OAS)+ Systemic Reactions
- PFAS emphasizes that one may have not only oropharyngeal symptoms but systemic symptoms 2-10% of the time
- Usually, only with raw foods, cooked plant foods may provoke PFAS
- Prick-by-prick testing of fresh food is preferred for most fruits and vegetables
- Stable allergens, e.g., peanut, hazelnut, and pea, maybe best detected with commercial extracts
With a Pollen Food Allergy Syndrome, you also have an Oral Allergy Syndrome that can manifest into systemic reactions. This occurs about two to 10% of the time. This usually happens with raw foods. However, cooked plant foods may provoke PFAS. Prick-by-prick skin testing of fresh food is preferred for most fruits and vegetables when trying to identify them. Stable allergens like peanuts, hazelnuts, peas are best detected when you use a commercial extract.
PFAS: Oral Food Challenges
- PFAS patients often have multiple positive prick test for fruits & vegetables
- Positive tests do not always predict clinical symptoms upon ingestion
- The oral challenge is the only definitive method of diagnosing
**Only a board-certified allergist should administer oral food challenge**
PFAS patients often have multiple positive prick tests to fruits and vegetables, but a positive test does not always predict what clinical symptoms a person might have upon ingestion. Thus, the most definitive method is an oral food challenge. This should only be provided by a board-certified allergist and never at home.
When to do Oral Food Challenges
- A systemic reaction to mixed foods, with culprit food unknown
- Hx of reaction to specific food with negative specific IgE testing
- Following the systemic reaction, to determine tolerance to cross-reactive foods not part of the usual diet
- It is unclear if cooking eliminates the symptoms
- History is unclear, and the patient wishes to ingest the implicated food
An oral food challenge is completed when there is a systemic reaction to mixed foods (with an unknown culprit of food) or a history of a reaction to a specific food with a negative specific IgE testing. This is when a person has tested negative but still has a reaction or following a systemic reaction to determine the tolerance to any cross-reactive foods that were not part of the usual diet. You also would do an oral food challenge if it is unclear if cooking eliminates the symptoms. If the history is unclear and the patient wishes to ingest that food, they would be tested via the oral food challenge.
Fast Facts: PFAS & OAS
- The course is often benign
- Small percent experience a serious reaction
- The severity of subsequent reactions is unpredictable
- Severe reactions can occur upon the first ingestion of a food with cross-reactive allergens
- Systemic reactions to previously tolerated foods can occur
- Allergists are divided on management strategy
- NIAID guidelines, as broadly interpreted, would allow for the administration of auto-injector
Here are some of the fast facts for PFAS and OAS. The course of PFAS and OAS is often benign, with only a tiny percent of people that have a serious reaction. The severity of the subsequent reactions is unpredictable. You may have a mild case and then a severe case which is unpredictable. Severe reactions can occur upon the first ingestion of a food with cross-reactive allergens, pollen, and food. Systemic reactions to previously tolerated foods can occur. Allergists are divided on the management strategy for PFAS and OAS, but the NIAID guidelines, as broadly interpreted, would allow for the administration of an auto-injector.
Case Three
- A 15 y/o girl w/ a history of tree pollen allergy develops itching of her mouth, soft palate, and ears each time she eats apples, pears, and fresh vegetables. The reactions have worsened over the last two years and recently include a dry cough.
- Would you prescribe an Epinephrine auto-injector for this girl?
Here is case three. This 15-year-old girl with a history of a tree pollen allergy develops itching in her mouth, soft palate, and ears each time she eats apples, pears, and fresh vegetables. The reactions have worsened over the last two years and recently included a dry cough. Would you prescribe an Epinephrine auto-injector for this girl? Yes or no? The answer is yes because we know that anytime there is this itching of the mouth and soft palate, there is a possibility of a severe anaphylactic reaction. An Epi-Pen would be the proper treatment.
Allergic to Exercise
What happens if you are allergic to exercise?
Symptoms
- Extreme fatigue
- Wheezing
- Flushing
- Rash
- SOB
- Gut-wrenching stomach pain
- Need to use the restroom
The symptoms of exercise-induced anaphylaxis are extreme fatigue, wheezing, flushing, rash, shortness of breath, gut-wrenching stomach pain, and the need to use the restroom. It does not need to be all of these symptoms, but it could be several. Each individual will manifest this differently. An individual should seek a doctor or a board-certified allergist if they suspect this.
Exercise-induced Anaphylaxis
- Cause is unknown
- Possible association between eating food or taking medicines and exercising
- Quick Tips
- Rx for 2 Epi-Pens
- Wait 4-6 hours after eating or RX
- Anaphylaxis Emergency Plan
- If symptoms: STOP, Use Epi-Pen
- Exercise with a friend who understands
The cause is unknown, but there is a possible association with eating food/taking medications and then exercising. Quick tips for exercise-induced anaphylaxis are a prescription for two Epi-Pens that you would carry with you, waiting four to six hours after eating or taking a medication, using an Anaphylaxis Emergency Plan, and with symptoms, stopping the activity, using the Epi-Pen, and calling 911. It might be beneficial for the individual to exercise with a friend or a buddy who understands the condition and can be trained in using the Epi-Pen.
The Latex Files
Latex Allergy
- Reaction to protein in rubber tree plant
- Present in over 40,000 products
- The immune system responds to harmless proteins by overproducing IgE that leads to symptoms.
- Sensitization occurs
- Coughing, sneezing, watery eyes, SOB
Latex allergies are something that we have been dealing with for some time, especially in healthcare. Most healthcare facilities have restrictions on having latex, both for gloves and balloons. Instead, they use vinyl gloves or other products.
The latex allergy is a reaction to a protein in the rubber tree plant. It is present in approximately 40,000 products. The immune system responds to this harmless protein by overproducing IgE, which then leads to symptoms. When sensitization occurs with a latex allergy, the milder symptoms are coughing, sneezing, watery eyes, and shortness of breath.
Ins and Outs of Latex Allergy
- Enters the immune system
- Inhaling allergens: Powder, balloons
- Absorbing allergens externally via cuts or sores
- Absorbing allergens internally via injection ports, stoppers on medication vials
Latex can enter the immune system in several ways. The powder inside the gloves or balloons can be inhaled, can be absorbed externally through cuts or sores on the body, or those allergens can be absorbed internally by injection ports and stoppers on medication vials.
Severe Symptoms
- Feelings of impending doom
- Urticaria
- Shortness of breath
- Wheezing
- Oropharyngeal swelling
- Vomiting
- Lightheadedness
There can be severe allergy symptoms from latex with feelings of impending doom, urticaria, shortness of breath, wheezing, oropharyngeal swelling, vomiting, and lightheadedness.
Latex Allergy Facts
- Many are unsure of how the allergy developed
- 1-6% of the general population
- 10-17% of healthcare workers in the U.S. (ALAA)
- 17% of restaurant workers
- Most reactions to latex gloves due to chemicals inside, e.g., contact dermatitis (Dr. Jordan Fink, MD)
PREVENTION: Strict Avoidance
Many are unsure about how this allergy is developed. One to 6% in the general population, 10 to 17% of healthcare workers in the United States, and 17% of restaurant workers have a latex injury.
, most reactions to latex gloves are due to chemicals inside, and they will cause things such as contact dermatitis. The prevention for latex allergy is strict avoidance. Interestingly, patients with multiple surgeries like spina bifida patients are at increased risk for latex allergy due to the increased contact with products.
Latex can be found in many products (Figure 5).
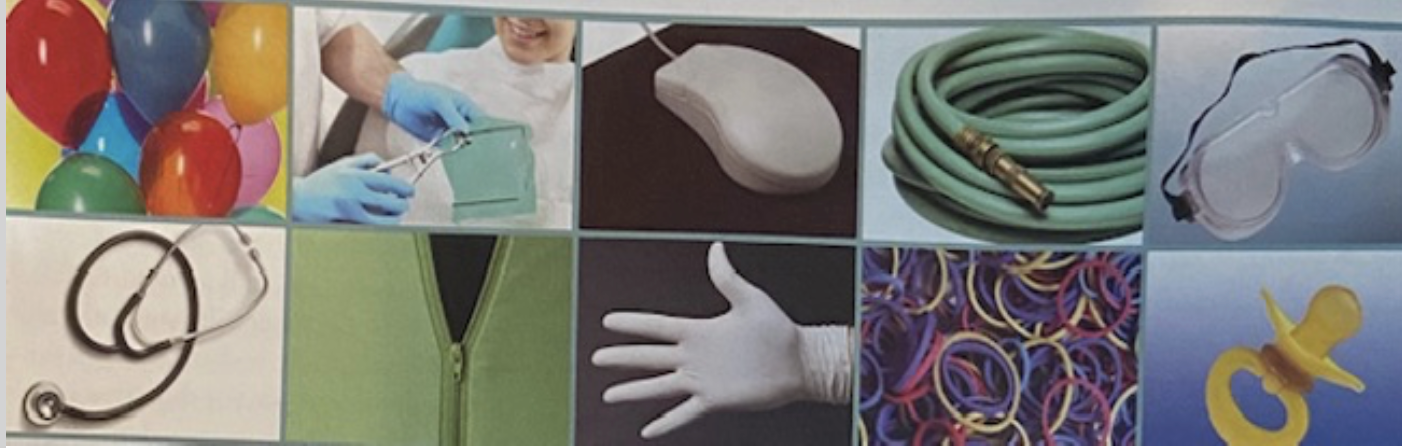
Figure 5. Examples of products with latex.
It is in our stethoscopes, computer mouses, balloons, gloves, garden hoses, goggles, pacifiers, et cetera. I mentioned 40,000 products, so latex is everywhere. If you are sensitive to it, do your best to avoid it.
Medications That Cause Anaphylaxis
Statistics
- Antibiotics-Penicillin most common
- 400 deaths/year
- May not be a lifelong condition
- Aspirin, NSAIDs
- Anesthesia Drugs
- Vaccines (especially egg-based)
- Insulin (rarely)
**Most severe IM, IV**
What medications cause anaphylaxis? Antibiotics (penicillin) are the most common. There are about 400 deaths per year from that in the United States. It may not be a lifelong condition, though. If you have an allergic reaction to penicillin once, this does not mean you will have it forever. Broad-spectrum antibiotics can be used in place of penicillin, but they tend to be less effective, more costly, and have greater side effects. This is something to consider.
Aspirin and NSAIDs also can cause anaphylaxis. Anesthesia drugs, vaccines, especially if they are egg-based, and insulin (rarely) can cause a reaction. When there is a reaction, the most severe reactions occur with a medication given intramuscularly or intravenously.
Symptoms
- Flushing, hives within moments to a few hours
- Contact your allergist
- Multi-body parts
- Hives
- Wheezing
- Stomach cramps
What are the symptoms of anaphylaxis? Flushing and hives within moments to a few hours is one sign. This does not specifically mean that a crisis is happening, but it is advisable to contact your allergist and find out what you should do. If there are multi-body parts involved like hives, wheezing, and/or stomach cramps after taking a medication, this necessitates a 911 call.
Anaphylaxis Facts/Treatments
Average Time To Respiratory or Cardiac Arrest Due to Anaphylaxis
- Food Allergy: 30 min.
- Venom Allergy: 15 min.
- Medication Allergy: 5 min.
Clinical and Experimental Allergy, Vol. 30, Issue 8
The average times for respiratory or cardiac arrest due to anaphylaxis for different allergens are listed in the above chart. This is important information to know.
Many Mediators Cause Anaphylactic Symptoms
- Leukotrienes
- Prostaglandins
- Kinins
- Platelet Activating Factor
- Interleukins
- Tumor necrosis factor
- Histamine
All of these mediators can cause anaphylactic symptoms.
- Antihistamines ONLY target Histamines
- Coughing, sneezing, watery eyes, itchy skin
Antihistamines only target histamines. When there is a histamine reaction like coughing, sneezing, watery eyes, and itchy skin, an antihistamine can be used. This is not an anaphylactic type situation.
Actions of Epinephrine: Inhibit the Effects of All Mediators
Epinephrine inhibits the effects of every single mediator that I just listed.
- Epinephrine Targets
- a1-adrenergic receptor
- increased vasoconstriction
- increased peripheral vascular resistance
- decreased mucosal adema
- a2- adrenergic receptor
- insulin release
- ß1- adrenergic receptor
- increased inotropy
- increased chronotropy
- ß2- adrenergic receptor
- increased bronchodilation
- increased vasodilation
- increased glycogenolysis
- decreased mediator release
- a1-adrenergic receptor
(Simons KJ, Simons FER. Curr Opin Allergy Clin Immunol. 2010;10:354-361).
These mediators, when they are ramped up in the body, are going to put the body in crisis with vasoconstriction, peripheral vascular resistance, edema, insulin release, dumping insulin, inotropy, and chronotropy. Inotropy is when the heart contracts more vigorously and violently. Chronotropy is when the heart races and speeds up. And then, of course, bronchodilation, vasodilation, glycogenolysis, all of those mediators are releasing in the body, and the only thing that can turn that around is Epinephrine.
Epinephrine IM: Time to Onset
When using Epinephrine intramuscularly, the time to the onset of reducing symptoms is shown in Figure 6.
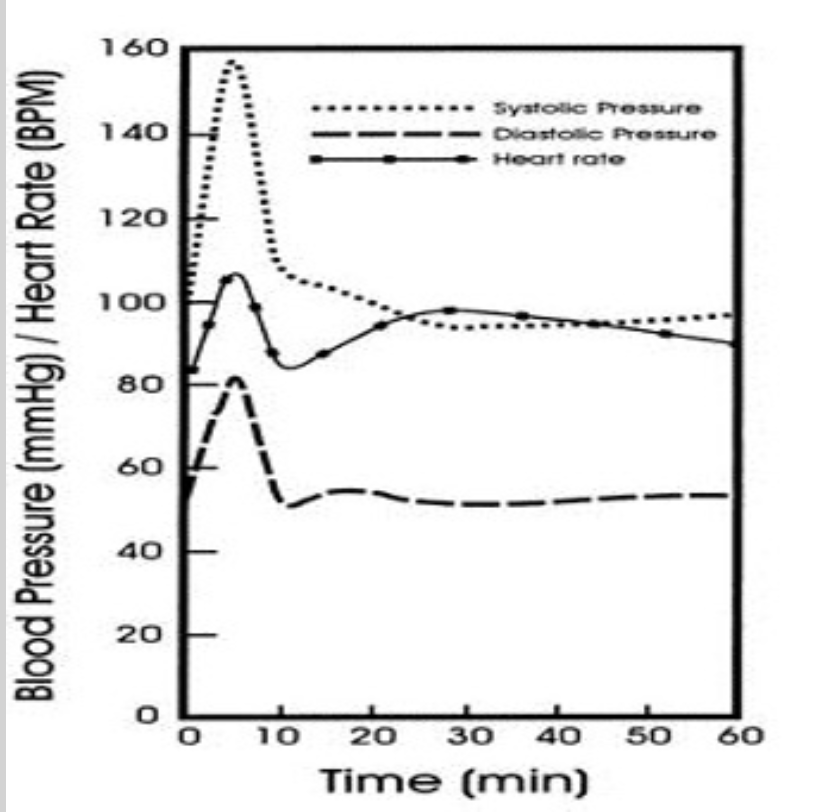
Figure 6. Time to reduce symptoms after Epinephrine.
In this chart, you can see the systolic and the diastolic blood pressure and the heart rate were back to homeostasis in less than a 10-minute timeframe. The reaction and turnaround are swift.
Antihistamines: Time to Suppression
This chart in Figure 7 looks at antihistamines and how long it takes for suppression of symptoms. For example, fexofenadine is an antihistamine, and it takes 101.2 minutes to suppress acute urticaria or rash.
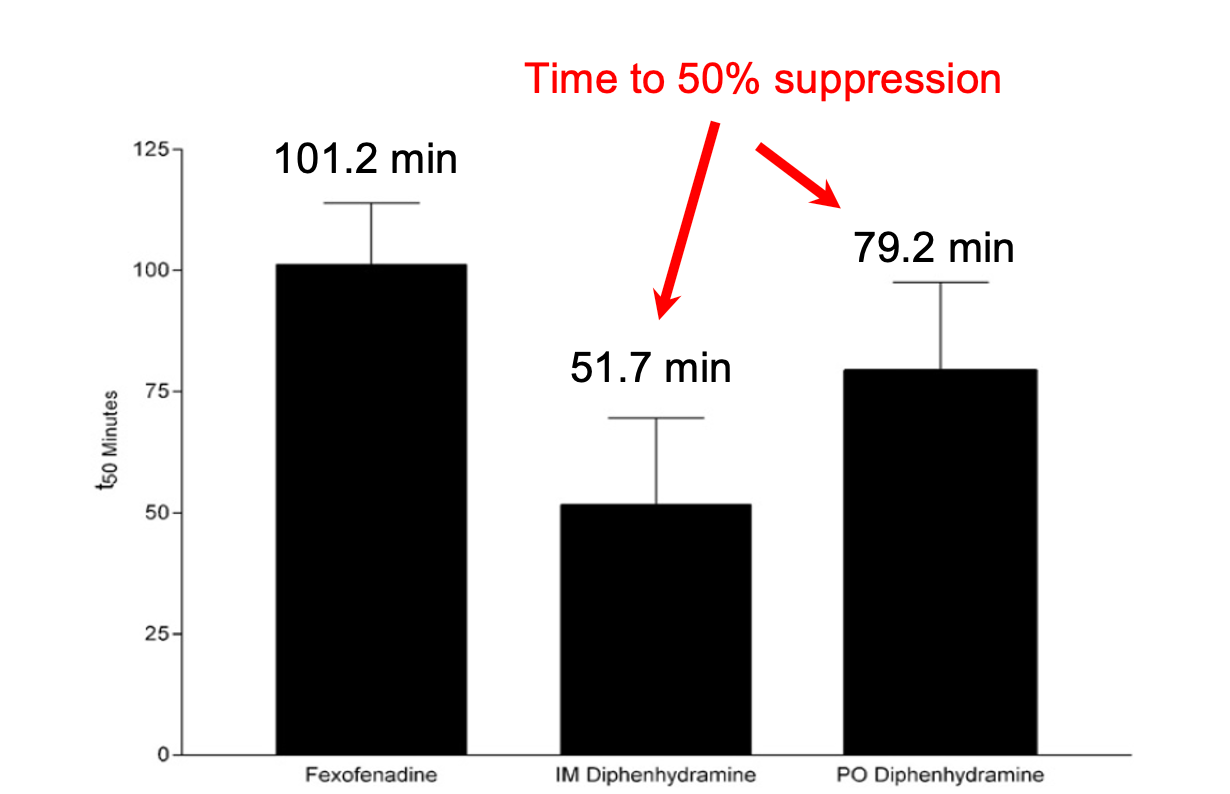
Figure 7. Time to suppress symptoms using antihistamines.
You can also see that it took IM intramuscular diphenhydramine 51 minutes before resolving, and then PO diphenhydramine almost 80 minutes.
FAST Facts
- Early signs and symptoms may not be outwardly apparent
- Anaphylaxis can progress rapidly w/ death occurring in minutes
- Epinephrine is rapid-acting and inhibits the effects of all mediators
- Antihistamine does not act fast enough and antagonizes only the effects of histamine
- Epinephrine is the first line of treatment for anaphylaxis
- Up to 30% of patients require more than one epinephrine auto-injector
Here are some fast facts. The early signs and symptoms may not be outwardly apparent, and they can progress rapidly, with death occurring within minutes. Epinephrine is rapid-acting and inhibits the effects of every mediator. Antihistamine does not act fast enough, and it antagonizes the effects of histamine. Thus, Epinephrine is the first-line treatment for anaphylaxis. Up to 30% of patients require more than one Epinephrine auto-injector. This means that approximately 70% require only one dose, and 30% require two.
Epinephrine- No Contraindication
Epinephrine is the only medication that has no contraindication. You can give Epinephrine even with mild symptoms. It is never going to hurt someone, so never hold back in delivering it.
Patterns of Anaphylaxis
- Uniphasic
- Symptoms resolve within minutes or hours after treatment and do not reoccur
- Biphasic
- Symptoms reoccur 1-72 hours after initial resolution of symptoms
- Protracted
- Symptoms continue for hours or days
The progression patterns of anaphylaxis are uniphasic, biphasic, and protracted. Uniphasic is when you have symptoms, are treated with an Epinephrine auto-injector, and within minutes or hours after treatment, the symptoms do not reoccur. Biphasic is a whole different story and is represented in Figure 8.
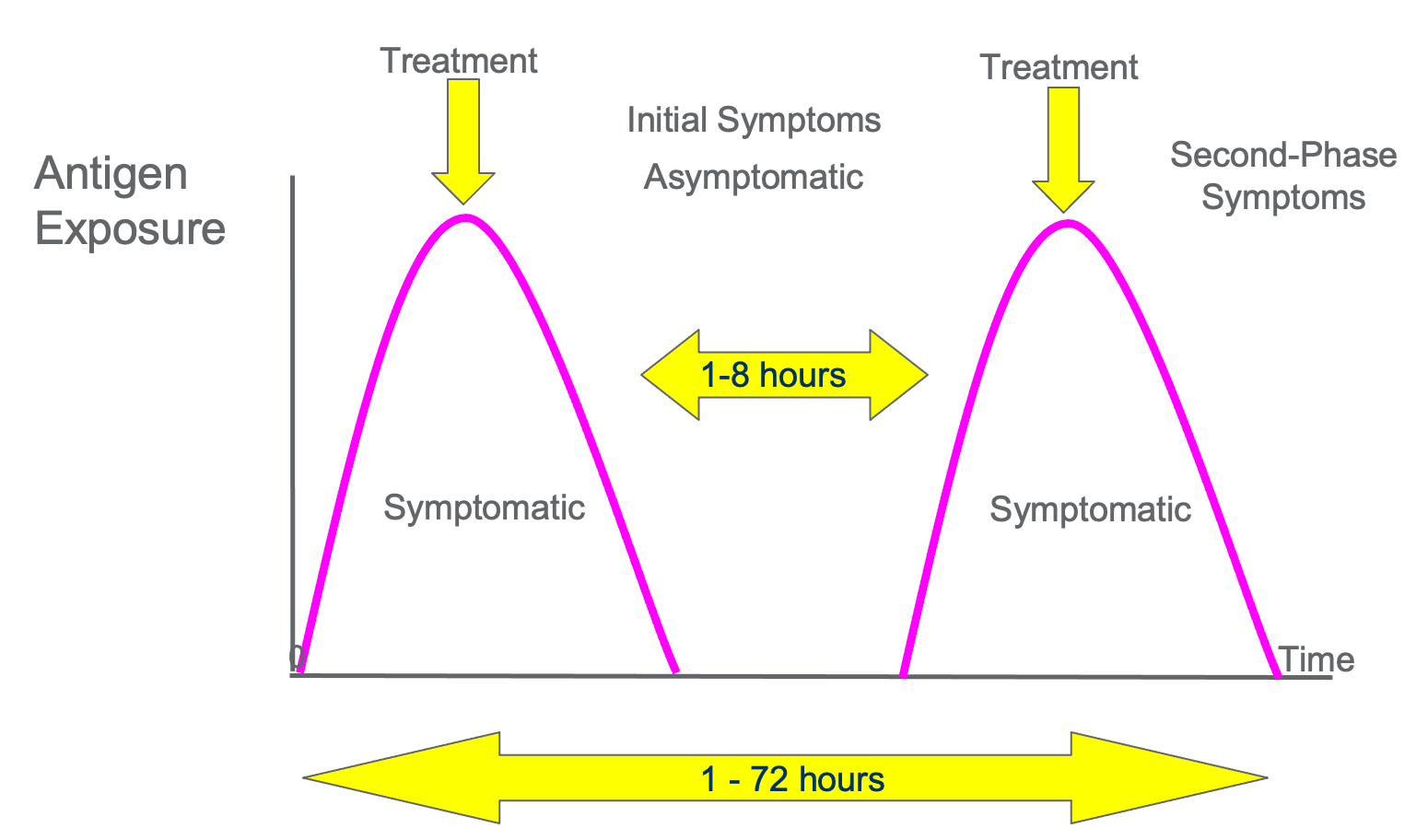
Figure 8. A biphasic pattern of anaphylaxis.
Biphasic is when you have symptoms that reoccur after you are completely asymptomatic for some time. The resurgence of symptoms can occur between one and 72 hours after the initial resolution of symptoms.
A protracted pattern or progression is when symptoms continue for hours or even days.
Epinephrine
Two Doses Are Readier Than One
- Episode severity, duration is not predictable
- The episode may respond to initial treatment, but symptoms return minutes or hours later (biphasic)
- The need for more than one dose occurs in up to 30% of episodes
Two doses are readier than one. The episode severity and duration of the anaphylactic reaction are not predictable for anyone anywhere. The episodes may respond to initial treatment, but symptoms return minutes or hours later as in biphasic progression. The need for more than one dose occurs, as I mentioned, in up to 50% of episodes.

Figure 9. Examples of Epi-Pens.
Epi-Pen Use
- PULL OFF THE SAFETY CAP
- Firmly swing and push the tip into the outer thigh
- HOLD in place 10 seconds
- Massage the injection site for 10 seconds
- SEEK EMERGENCY MEDICAL ATTENTION
- Side effects
- Uncontrolled shaking, twitching, feelings of panic and anxiety
The way you use the Epi-Pen is you pull off the safety cap with intention, firmly push the tip into the outer thigh of any individual, no matter young or old, and hold it in place for 10 seconds. This is depicted in Figure 10.

Figure 10. Demo of using an Epi-Pen.
You want to make sure the leg is immobilized and the Epinephrine auto-injector is held in place for 10 seconds. If it comes out, the needle retracts and can not be given again. You can also massage the injection site for about 10 seconds. The person must seek emergency medical attention right away. After giving the Epinephrine, the individual may have uncontrolled shaking, twitching, and feelings of panic and anxiety. Again, to use the Epi-Pen, pull off the safety cap, firmly swing and push the tip into the outer thigh, and hold in place for 10 seconds. Massage the injection site for 10 seconds. Seek emergency medical attention immediately by dialing 911.
Maintenance
- Store at room temperature
- Extreme heat and cold will render the epinephrine ineffective or cause the injector to malfunction
- Avoid direct sunlight as oxidation will occur
- Medication will appear dark or have heavy particles
- Oxidation over time
- Check the expiration dates on all devices
Epinephrine auto-injectors need to be stored at room temperature. There was a study (not cited in the references) where the Epinephrine pens were stored at between 80 and 85 degrees. That is not terrible. However, if you have them stored in extreme heat and cold, it could render the Epinephrine ineffective or cause the injector to malfunction. For example, if it is left in a cold car, it might not work right. Also, we want to avoid direct sunlight because oxidation can occur, and the medication can appear dark or have heavy particles. It is important to check the expiration dates on all of the devices. If many people have an Epi-Pen like a coach, grandma, et cetera, the individual should document these and know the expiration dates. However, if there is an emergency and an Epinephrine auto-injector is needed, even if the medication has expired and you do not have another dose, it is important to go ahead and give that dose.
Auvi-Q Auto-injector
The Auvi-Q auto-injector is nice because it is like an AED. It is shown in Figure 11.

Figure 11. Example of an Auvi Q auto-injector.
It has voice prompts and audio and visual cues. There is also only a five-second hold time versus a ten-second with the Epi-Pen. There is a retractable needle, which is a nice mechanism to have, but it cannot come out before its time. Again, you are going to use it with intention.
Epinephrine First/Epinephrine Fast
- All 50 states guarantee the right to carry and self-administer
- Most states allow or require schools to stock epi-pens
- Check your state: www.Allergyasthmanetwork.org/stock-epinephrine
All 50 states guarantee the right to carry and self-administer Epinephrine. Most states allow or require schools to stock Epinephrine pens, but not every state. You can check your state at the link above.
Publications
The "Anaphylaxis Management" magazine from the Allergy & Asthma Network has a great resource on Epinephrine pens and the auto-injectors. The chart will tell you important things like, does the Epinephrine auto-injector have a voice prompt? Does it have an automatic, retractable needle? Some do not. It also has pediatric and adult medications listed. Listed at the bottom, it has some financial resources because Epinephrine pens can be costly. There are generic brands, but they are still expensive. My EpiPen Savings, the Mylan company, and the Impax company also have resources to help pay.
There are a couple of publications from the Allergy & Asthma Network that are free. Contact them and get these booklets as resources for you at your facility. You can share these with individuals. There is also a poster that is included in the magazine showing and overview of anaphylaxis.
Myth Busters
Let's go ahead and just wrap up the program with myth busters.
- MYTH: Children younger than 3 years old cannot be tested for food allergies.
- TRUTH: There is no specific age limit for food allergy testing. If you think your child has a food allergy, contact an allergist who will evaluate history, symptoms, and recommend options for testing.
If you think your child has a food allergy, contact an allergist. They will evaluate the history and the symptoms and recommend what the options for testing are.
- MYTH: Children with an egg allergy should NOT get the flu shot.
- TRUTH: Children with mild reactions to eggs, such as hives, may receive the regular flu shot. The CDC recommends they be monitored in a physician or pharmacist’s office for 30 minutes after receiving the injection.
Our next myth is about egg allergies. The CDC recommends that an individual with an egg allergy be monitored in a physician or pharmacist's office for about 30 minutes after receiving an injection.
- MYTH: Gluten is a food allergen, and eliminating it from my diet will help me feel better.
- TRUTH: Gluten is not a food allergen. It is a protein composite found in wheat, barley, and rye. GI problems from gluten are experiencing an intolerance, not an allergy.
The truth is gluten is not a food allergen. If you have gastrointestinal problems with gluten, you are experiencing a gluten intolerance, not an allergy. The other thing I want to mention is that by going on a gluten-free diet, you are eliminating foods that are high in fiber, vitamin B, zinc, and iron. Be sure you talk to your doctor before you eliminate gluten from your diet.
- MYTH: I experience only mild itchiness when wearing latex gloves, so I am not seriously allergic.
- TRUTH: Many individuals with a latex allergy will experience only a hand rash when wearing latex gloves. BUT this can be a progressive condition. Reactions to latex can become more severe with repeated exposure.
Many individuals with a latex allergy will experience mild symptoms like a hand rash when they wear gloves. However, this can be a progressive condition. We often don and doff gloves throughout the workday. A reaction to latex could be much more severe with repeated exposure.
- MYTH: I am allergic to shellfish. Since shellfish contain iodine, that must mean I am allergic to iodine-based surgical scrubs, radiocontrast solutions used for x-rays, and CT scans.
- TRUTH: Iodine is not an allergen. It is present in our bodies, in our thyroid hormones, amino acids, and is essential to our health. There is no cross-reactivity with iodine-based preps or radiocontrast.
Here is our final myth buster. Iodine is not an allergen. It is present in
