Editor’s note: This text-based course is a transcript of the webinar, Acute Non-Invasive Ventilation, presented by Rena Laliberte, BS, RRT, Clinical Education/Emergency Medicine Specialist.
Learning Outcomes
After this course, participants will be able to:
- Discuss the primary reasons NPPV fails despite its strong evidence-based research
- Recognize patient selection criteria and response to therapy
- Identify modes and parameter selection when using BiPAP or CPAP
- List potential complications and titration strategies for weaning
- Discuss the differences between HHFNC, and other available equipment
Introduction
This has been a passion of mine for a very long time. I am looking forward to teaching you something that is very near and dear to my heart.
Non-Invasive Positive Pressure Ventilation (NPPV)
- Non-Invasive Positive Pressure Ventilation (the absence of an artificial airway, utilizing a mask or other interface) has been used since the 1980s
- Since then, it has been the subject of numerous randomized clinical trials and its use in Acute Hypercapnic Respiratory and Hypoxemia Failure has been well documented.
- For the purposes of this lecture, we will focus on the acute aspects of the use of NIV.
- Despite the most current evidence with supporting clinical practice updates and guidelines, NIV remains a technically difficult therapy to truly learn well enough to utilize to its fullest potential for success in our patients.
- Knowledgeable Respiratory Therapists and other Licensed Healthcare providers can be instrumental in proper patient selection, initiation, and management of Acute NIV.
Non-invasive positive pressure ventilation has been around for a long time, since the 1980s. Since then, there have been numerous randomized clinical trials and research projects, primarily regarding hypercapnic and hypoxemic respiratory failure. All of these studies and trials have been extremely well-documented.
For the purposes of this lecture, we are going to focus on the acute aspects of non-invasive ventilation, not the chronic aspects like obstructive sleep apnea. Despite the most current evidence and support for its use, this type of ventilation remains very technically difficult for people. People have a difficult time learning it. Due to this, it is not used to its full potential and not used very successfully.
Knowledgeable respiratory therapists and other licensed healthcare providers can be very instrumental in proper patient selection, initiation, and management of acute non-invasive ventilation.
Why Does NPPV Fail?
Why does non-invasive positive pressure ventilation fail? I have given this talk, or a version of it, numerous times over the past 10 to 15 years. I personally already know the answer to this question, but for the purposes of this talk today, I wanted to do a quick Google Scholar search and share the results. I just typed in, "lack of knowledge in non-invasive ventilation."
- Articles (Google Scholar search for “lack of knowledge in Non-Invasive Ventilation”)
- About 85,600 results (0.08 sec)
What does the evidence show?
I received almost 86,000 results in 8/10s of a second. What does the evidence show? Here are some studies I found.
Utilization of Noninvasive Ventilation in Acute Care Hospitals: A Regional Survey Chest (Maheshwari et al., 2006)
- Results
- We obtained responses from 71 of the 82 hospitals (88%)
- The overall utilization rate for NPPV was 20% of ventilator starts, but we found enormous variation in the estimated utilization rates among different hospitals, from none to > 50%
- The top two reasons given for lower utilization rates were a lack of physician knowledge and inadequate equipment
- In the 19 hospitals that provided detailed information, COPD and congestive heart failure constituted 82% of the diagnoses of patients receiving NPPV, but NPPV was still used in only 33% of patients with these diagnoses receiving any form of mechanical ventilation
The particular article that I pulled up was a regional survey that was done by Dr. Maheshwari entitled, "Utilization of Non-Invasive Ventilation in Acute Care Hospitals." He sent out a survey to 82 hospitals and got responses back from 71, or 88% of hospitals responded.
They were looking at the overall utilization rate for non-invasive positive pressure ventilation. In all ventilator starts, only 20% of those were non-invasive positive pressure ventilation. And even amongst those, he found an enormous variation in the utilization rates between different hospitals, ranging everywhere from not at all up to 50%.
The top two reasons given in this survey for the low utilization rates were lack of physician knowledge of non-invasive ventilation and inadequate equipment. Nineteen of those hospitals provided very detailed information about the use of non-invasive positive pressure ventilation, and COPD and congestive heart failure constituted 82% of the diagnoses of patients receiving it. However, non-invasive positive pressure ventilation was still only used in 33% of those patients needing any form of mechanical ventilation.
What that means and what the doctor mentioned in this paper is that if the hospital did not understand non-invasive positive pressure ventilation, these patients were placed right away on invasive mechanical ventilation. Instead of even trying non-invasive positive pressure ventilation, these doctors were intubating these patients.
Evidence-based Utilization of Noninvasive Ventilation and Patient Outcomes (Mehta et al., 2017)
The results of this study are summarized as follows:
- Among 22,706 hospitalizations with NIV as the initial ventilatory strategy, 6,820 (30.0%) had SECs.
- Patients with SECs had a lower risk of NIV failure than patients with weak evidence conditions (8.1 vs. 18.2%, P < 0.0001).
- Regardless of underlying diagnosis, patients admitted to hospitals with greater use of NIV for SECs had a lower risk of NIV failure (Quartile 4 vs. Quartile 1 adjusted odds ratio = 0.62; 95% CI = 0.49–0.80).
- Even patients without an SEC benefited from admission to hospitals that used NIV more often for patients with SECs (Quartile 4 vs. Quartile 1 adjusted odds ratio for NIV failure = 0.68; 95% CI = 0.52–0.88)
I really like this paper, "Evidence-based Utilization of Noninvasive Ventilation and Patient Outcomes," and have used it quite a bit. This was written by Dr. Mehta in 2017. This is a huge study where they looked at almost 23,000 hospitalizations retrospectively. Of those hospitalizations, 6,800 people that were put on non-invasive ventilation as the initial strategy had strong evidence conditions (SEC). These patients with SEC also had a very low risk of failure as compared to patients that were perhaps chosen, for whatever reason, were placed on non-invasive ventilation to increase the work of breathing. However, regardless of any underlying condition, patients who were admitted to hospitals that used non-invasive ventilation a good majority of the time did better and had a very low risk of failure. This was even true in the clients without a strong evidence condition and did not meet the initial criteria. I am going to talk about that in one second.
The conclusions are as follows:
- Most patients who received NIV did not have conditions with strong supporting evidence for its use with wide institutional variation in patient selection for NIV.
- Surprisingly, we found that all patients, even those without an SEC, benefited from admission to hospitals with greater evidence-based utilization of NIV, suggesting a “hospital effect” that is synergistic with patient selection
Evidence-based utilization of non-invasive ventilation in these patients showed that most patients who received non-invasive ventilation did not have conditions with strong supporting evidence for its use with wide institutional variation in patient selection. Surprisingly, they found again that in those hospitals without a strong evidence condition, people benefited from admissions to hospitals with greater evidence-based utilization of the non-invasive method, which suggested a hospital effect that is synergistic with that patient selection. In particular, hospitals, where they had a very strong knowledge base of non-invasive ventilation, tried it. The clients may have presented with an extreme work of breathing, an unknown code status, or no intubation information in the chart. Regardless of the reason why they chose non-invasive ventilation, the health professionals gave it a try based on their existing knowledge. And, if these patients were not going to fare well, they knew when to call it quits. They knew when to intubate. I still believe that these institutions had a strong knowledge base going in, and that is why these patients did so well.
The patient outcomes are as follows:
- Overall, 15.2% of patients failed initial treatment with NIV and subsequently required IMV
- Patients with SECs had significantly lower risks for NIV failure (8.1 vs. 18.2%; adjusted OR [aOR] = 0.21; 95% CI = 0.14–0.32)
- A patient’s risk of NIV failure was lower when admitted to hospitals with higher NIV-SEC rates (Quartile 4 vs. Quartile 1 aOR = 0.65; 95% CI = 0.50–0.83)
- In a subgroup analysis, patients without an SEC also had a lower risk of NIV failure when admitted to hospitals with higher NIV-SEC rates (Quartile 4 vs. Quartile 1 aOR = 0.68; 95% CI = 0.52–0.88)
Previously, I mentioned that 30% of the time non-invasive ventilation was used. Here it is saying that 15.2% of the patients failed initial treatments with non-invasive ventilation and subsequently required invasive mechanical ventilation or IMV. That sounds a little depressing, but that is about average. If this was used properly from the start, I think that you would see that this number would not be so bad and would actually drop off. The failure rate is lower in hospitals that utilize non-invasive ventilation and use it as it should be used with strong evidence conditions.
They also performed subgroup analysis where they looked at clients without a strong evidence condition. When they were admitted to hospitals that utilized non-invasive ventilation to its full potential, the patients ultimately did much better.
- Mortality among patients who suffered NIV failure was higher than those treated initially with IMV (39.4 vs. 31.0%; aOR = 1.49; 95% CI = 1.38–1.62)
- Among patients who failed initial NIV treatment, those with SECs had lower hospital mortality compared with patients with conditions with weak evidence for NIV use (11.1 vs. 28.7%; aOR = 0.44; 95% CI = 0.29–0.65)
- Patients who received NIV at hospitals with higher NIV-SEC rates tended to have lower hospital mortality rates than patients receiving NIV at low NIV-SEC rate hospitals (Quartile 4 vs. Quartile 1 aOR = 0.83; 95% CI = 0.68–1.00)
Mortality among patients who had a non-invasive ventilation failure was higher than patients that were initially treated with invasive ventilation (IMV). And among patients who failed initial non-invasive ventilation, those with a strong evidence condition had a lower risk of mortality as compared with patients that had weak evidence conditions for non-invasive ventilation use. So, if you are choosing the right patients and those patients are doing well on non-invasive ventilation because you are using the right criteria for patient selection, those patients' mortalities are going to be a lot less than if you are choosing to put a patient on with very weak evidence. Thus, depending on your patient population, you may have some failures despite your best efforts. But, if you are choosing the right patients at the right time, you are going to see those mortality rates drop off.
In this bottom statement, patients who receive non-invasive ventilation at hospitals with higher non-invasive ventilation/strong evidence condition rates tended to have lower hospital mortalities than patients at another facility that may not be using it properly. I know a lot of these numbers are a little complicated and if you are not used to reading research or understanding what quartiles are, it can be confusing. The bottom line is that those hospitals, that understand how to utilize non-invasive ventilation to its full potential compared to those hospitals that may be smaller or where the providers are not digging in and using non-invasive ventilation to its fullest potential, are going to do better. It just makes sense. Unfortunately, they may not fare well at other facilities that do not either have enough exposure, enough patients, or enough education regarding non-invasive ventilation.
Patient Selection
Key points on patient selection are as follows:
- Best Evidence (Strong Evidence Condition)
- Exacerbation of COPD (Impending Respiratory Failure, hypercapnia, respiratory acidosis)
- Congestive Heart Failure
- Post extubation support
- Obesity and obesity hyperventilation syndrome
- Chest wall abnormalities and Neuromuscular diseases, Palliative Care, DNI patients
- Low Level of Evidence
- Hypoxemic Failure (**Covid 19)
- Sepsis
- Pneumonia
- Asthma
There is a ton of information on patient selection. I have managed to condense some of this information for you. The best evidence or the best strong evidence condition that I have been talking about is the exacerbation of COPD. These are the clients with impending respiratory failure, hypercapnia, and present in respiratory acidosis. Another strong evidence condition is congestive heart failure. Once we extubate a patient off of a ventilator, this is somebody that either has a known lung condition or somebody that has been on mechanical ventilation and just needs a little bit of extra support post-extubation. This is very well documented. Obesity and obesity hyperventilation syndrome are others. Finally, the strong evidence conditions include anybody that has a chest wall abnormality. These are patients that present with scoliosis or kyphoscoliosis, have neuromuscular diseases such as ALS, Guillain-Barre, on palliative care, or patients that have a "do not intubate" order on their file. For all of these patients, there is a ton of evidence for using non-invasive ventilation.
As we are at the one-year anniversary of COVID-19, I will mention with a couple of asterisks that hypoxemic failure in COVID-19 is an area where the evidence is growing towards this use. Physicians are still in the middle of doing their research and evidence regarding these patients. Stay tuned on that one. I think as time goes on, you are going to see more evidence towards the use of non-invasive ventilation in COVID-19. For patients that have sepsis, pneumonia, and severe asthma, there is still not good evidence regarding its use, mainly because you are not going to be fixing something in a matter of a few hours, and sometimes not even a few days.
Absolute contraindications are:
- Shock
- Hemodynamic instability/cardiac ischemia/arrhythmias
- Multi-organ failure
- ARDS
- Severe Hypoxemia
- Recent Upper Airway or GI surgery
- Impaired Swallow
- Unable to protect the airway
- Unable to tolerate therapy
Contraindications for non-invasive ventilation would be patients that are suffering from shock, patients that have hemodynamic instability, multi-organ failure, and acute respiratory distress syndrome (ARDS). Other issues that are contraindicated are severe refractory hypoxemia, any recent upper airway or GI surgery, and an impaired swallow. Patients who are unable to protect their airway or tolerate the ventilation. I am going to spend some more time talking about those types of patients as well.
Important Considerations Before Choosing Mask Non-Invasive Ventilation
- Patient's level of consciousness
- Must be able to remove mask unassisted
- Must be able to control secretions
- The use of restraints should be an absolute contraindication
- There is no true “apnea” ventilation – Only a backup rate (explained later in presentation)
- You should not “mask” ventilate patients – For this situation, intubation and IMV should be considered
- The condition should be treatable and reversible within hours or a couple of days
- Vomiting, overwhelming pulmonary edema, or coughing up blood are all considered contraindications and put patients at risk for aspiration
- The patient must be able to tolerate therapy (claustrophobia and anxiety may be an issue)
There are some other important considerations before choosing mask non-invasive ventilation. One is the patient's level of consciousness. Sometimes we get asked to place patients on non-invasive ventilation, and I like to call them "opey-dopey." They are sleepy and lethargic, and sometimes they are very confused. If a patient has an altered level of consciousness and not really awake, they may not be able to understand what to do or be able to protect their airway.
They must be able to remove their mask unassisted if they get into any trouble. I instruct my patients how to put on a mask and remove it if I need to step away and they need to cough, feel nauseated, or need to throw up. They have to be able to do that, and if they are not awake or alert enough, this might not be the thing for them. They need to be able to also control their secretions.
We should never use restraints, and it should be an absolute contraindication. Policies can be different between facilities. I can only speak for myself and my institution. However, if a patient is confused or does not understand necessitating the need for restraints, this is not safe.
Most of the equipment that we use for non-invasive ventilation does not have true apnea ventilation. It only has a backup rate that I am going to be talking about later. Apnea ventilation is a big one. If your patient stops breathing, there is no true apnea backup so that has to be a consideration.
We should not be mask ventilating our patients. I should not be putting a mask on a patient, treating them acutely, setting a rate, and expecting a rate to be doing my job. We only usually use backup rates for those patients that are using non-invasive ventilation for neuromuscular things like ALS. If we are trying to correct a blood gas or something like that, setting a backup rate and mask ventilating these patients is not the best idea.
Any condition that we are treating should be reversible, if not within a few hours, at least within a day or two. For many of these patients, once we start treating them, we can give them little trials off. As their condition improves over a few days, they may be going on and off and on and off which is fine.
Vomiting, overwhelming pulmonary edema, or coughing up blood are considered contraindications and put our patients at great risk for aspiration. We should not be using it on those patients.
And again, the patient has to be able to tolerate it. They may have feelings of claustrophobia and extreme anxiety which can become an issue. We have to really work harder with those patients.
BiPAP Versus CPAP
- CPAP
- Continuous positive airway pressure consisting of some level of PEEP and a FI02
- The choice for Hypoxemic or “Fluid Events” as in Congestive Heart Failure/ Similar presentation in patients who have missed hemodialysis
- BiPAP
- Bi (two) positive airway pressures, EPAP (PEEP) end positive airway pressure and IPAP inspiratory positive airway pressure
- The Delta pressure between IPAP and EPAP is the level of pressure support that augments tidal volume/minute ventilation
- The choice for hypercapnia, when Tidal Volume is LOW, RR High and needs to be augmented as in COPD exacerbations
When we are using non-invasive ventilation, there are two modes that are used primarily, BiPAP and CPAP.
CPAP is continuous positive airway pressure. We are setting some level of PEEP, or the positive end expiratory pressure. This is the term that we primarily use in a mechanical ventilator for invasive ventilation. This is continuous positive airway pressure over time with some level of positive end expiratory pressure and a FiO2, a fraction of inspired oxygen. CPAP would be the choice for hypoxemic respiratory failure or fluid events as you would see in congestive heart failure, flash pulmonary edema, or someone who has missed hemodialysis. These patients can be extremely fluid-overloaded, and this is a great adjunct to treat shortness of breath in these patients that are suffering from that.
BiPAP is two positive airway pressures. You have expiratory positive airway pressure (EPAP) and inspiratory positive airway pressure (IPAP). I am going to show you this represented in a graph later on. The delta pressure between the inspiratory and expiratory pressures is the level of pressure support that is augmenting your tidal volume or minute ventilation. This would be the choice for a hypercapnic patient.
When you have a COPD patient that is presenting with acute failure, they have a very low tidal volume and a very high respiratory rate. Taking those two things, tidal volume times respiratory rate gives us minute ventilation. Patients present with high minute ventilation, and they cannot continue to breathe like that for an extended period of time.
What do we do? We need to augment that. We need to give them a higher volume, lower their rate, and lower their minute ventilation to treat the hypercapnia. Let the patient rest, and let them breathe more normally. This is what we do for COPD exacerbations, and I am going to talk about that when I focus on BiPAP by itself.
CPAP (Continuous Positive Airway Pressure)
Airway Pressure on CPAP
On this slide, I am showing you graphically what it looks like when a patient is on CPAP (Figure 1).
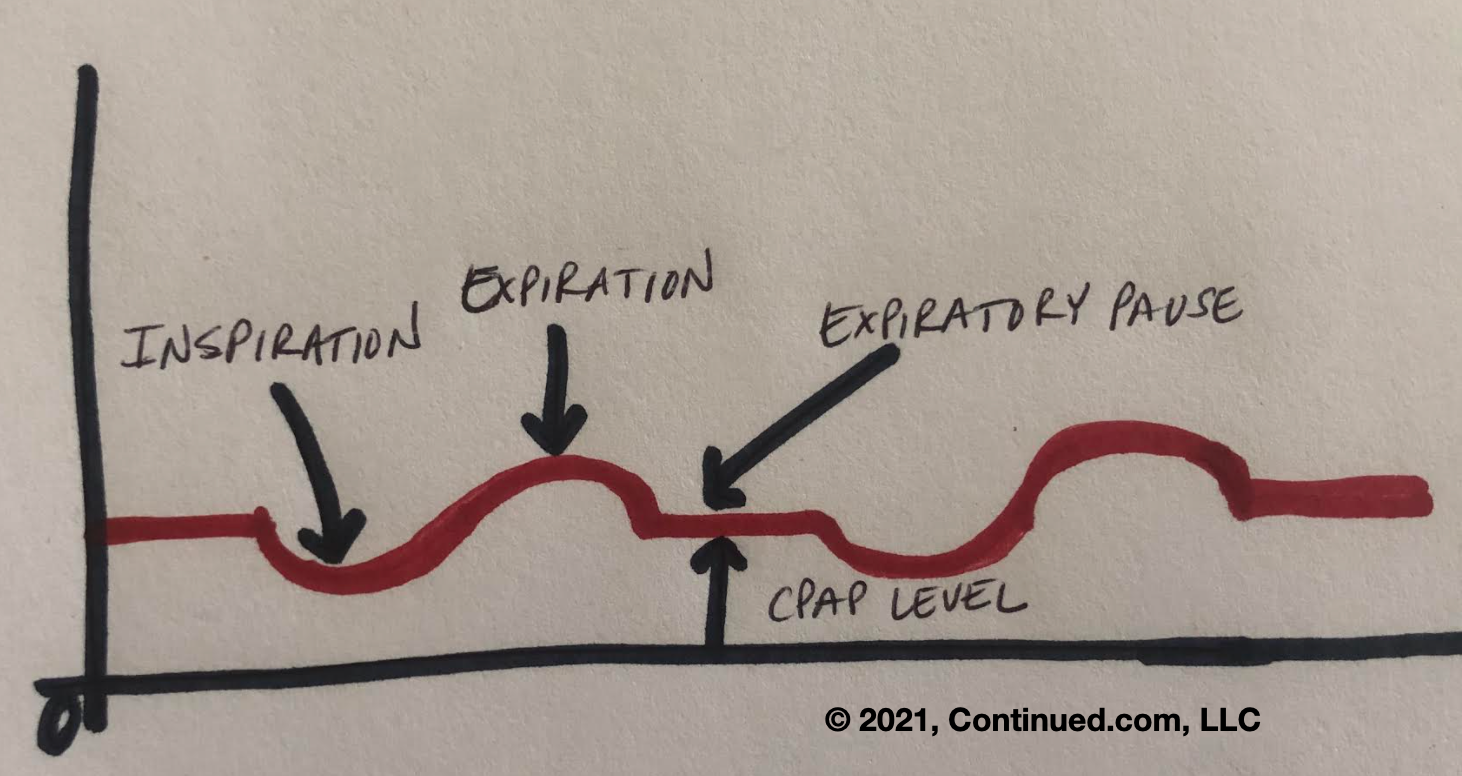
Figure 1. Airway pressure support on CPAP (Adapted from from Pillai, 2009).
With this, a patient is breathing in and out with contiguous pressure. It is like sitting in front of a fan or driving down the freeway with your head out the window. You have the constant pressure of the air coming at you. The higher it is, the stronger you are going to feel that flow and pressure. Imagine putting a mask on your client, strapping it around their head, and then increasing and decreasing this pressure depending on what they need. When you see them inspire, you are going to see a little dip in that pressure-time scalar. The only time you really see that big hump is during expiration is if the patient is actively exhaling or pushing against that pressure. It is not usually so pronounced as the graph. Ultimately, this is just a graphical presentation or explanation of what is happening. Whether the patient is inhaling or exhaling, that pressure is always going to be there. It never lets up.
Decision to Choose CPAP
- The decision to choose CPAP ventilation is based on evidence and patient presentation
- Specific pathology, patient assessment, and clinical criteria can all be used in decision making
- Most patients requiring CPAP are those patients who present with acute hypoxemic failure with minimal or poor response to continuous oxygen therapy (COT), and long with the following:
- Orthopnea
- Pulmonary Congestion on X-ray or CT
- Elevated BNP
- Congested (crackles) lung auscultation
- PaO2/FI02<300mmHg
- Pa02 <60mmHg ( Normal or Alkalotic PH)
The decision to choose CPAP is based on not only the evidence but your patient. You have to look at your patient and see how they are presenting when they come into your facility. They can be in the emergency room, the ICU, or even on a general floor with an acute change in their ventilatory status. Most patients, as I said, present with acute hypoxemic failure or may have minimal or a very poor response to continuous oxygen therapy. They may be desaturating and you first try them on a nasal cannula. If they do not get any better, you may go to a non-rebreather with a little bit of improvement but their saturations are still not where you would like them to be. You may see that the patient still has trouble breathing and look uncomfortable. If you feel like they are not progressing and are having this poor response to conventional oxygen therapy, you have to start thinking about something else. You have to rely on the presentation of the patient because it takes time to get these other clinical signs and reports such as the results of a chest X-ray, CAT scan, or lab work. And, if you see an elevated BNP, you would question whether they have congestive heart failure. You could auscultate breath sounds to hear if they have fluid onboard. Are you hearing crackles or coarse rhonchi? The P/F ratio in these patients is usually less than 300, and if I take a blood gas, venous or arterial, they are going to have a low PO2. The interesting thing about these patients is the pH of those gases is either going to be within your normal limits, or they may be on the alkalotic side because these patients are not retaining CO2. They can be very tachypneic, as you would see with a PCO2 that is lower and more on the alkalotic side. If we determine that our patient meets our strong evidence-based criteria and choose CPAP, we are going to want to use mask ventilation on these patients and the mode is CPAP.
CPAP Parameters
- Mode is Chosen, Where Do We Start?
- Always best to begin at tolerable pressures and titrated to need
- Begin at 100% and 5-8cmH20
- As FI02 is weaned down – if saturation begins to drop, increase the CPAP level in 2cm H20 increments
- Continue until FI02 is <60%
- Avoid hyperoxia
- Monitor patients closely for responsiveness to all therapy
- RT assesses for tolerance and synchrony
- All patients should be assessed every hour for the first 3 hours. If the patient is not responding to therapy and continues to deteriorate, do not delay in moving to IMV.
It is always best to begin at a tolerable pressure, and then titrate as needed. This is one of the things that I am going to tell you right now and where knowledge is a problem. I may see a patient that is struggling. Think about what your patients look like. Are they hypoxemic or diaphoretic? If they are afraid, they can be very hypoxemic. They may be telling you, "I can't breathe. I am not going to make it." You have to gain their trust and put a mask on this patient. It is going to blowing air all over the place, and they are not going to like it. While I know ultimately I am going to need a higher pressure, I am not going to start there.
We are going to start off at low tolerable pressure and at 100%. You do not want to put the patient on too much oxygen, but you also do not want them to have hyperoxia. You want to start out at 100% at low pressure. As you wean down the oxygen, you are going to slowly increase the CPAP level. You want to get to the level that your provider sets like a saturation greater than 92%. You want to continue to wean until your patient not only looks better but is getting some decent numbers. You want to see that their heart rate is going down, their blood pressure looks good, their saturation is good, and that they look comfortable. You have to get that buy-in and explain to them what is going to happen. In order to do that, you have to give them time, get them comfortable, and most importantly, monitor them closely for responsiveness to all therapy.
Then, we have to look for tolerance and synchrony. All patients should be assessed at least every hour. Check them frequently. You cannot set them up and leave. You have to stay on top of these patients, and it can be a lot of work. If you see that there is no real change and the patient continues to deteriorate, you need to be right there to make adjustments. Sometimes, despite our best effort, these patients continue to deteriorate. If that is the case, we need to alert the provider of the need to move to more invasive mechanical ventilation.
CPAP Treatment
- Work of breathing in these patients is directly correlated to the length of time and degree of hypoxemia
- Correction of hypoxemia usually will correct work of breathing
- BiPAP has been used, however, if VENTILATION is excessive in these patients, they are at risk for self-induced lung injury (SILI)
- On minimal settings, tidal volumes can easily exceed > 800ml and have been noted as well over 1 Liter, which places these patients in the high risk of failure group
The work of breathing in these patients is usually directly correlated to how long they have been hypoxic. Sometimes, patients know that if they are not feeling well and go to the hospital, they are going to be admitted. Due to this, they will stay at home and come in very late. We have to be cognizant of that.
We also get requests, because of the work of breathing, to put these patients on BiPAP, not CPAP. This may not be the best choice. The providers want to address the work of breathing in these patients due to this hypoxemia and give these patients pressure support. Even on the most minimal settings on BiPAP, tidal volumes in these patients can exceed over 800 ml to over a liter. Not only does this put these patients at risk for a self-induced lung injury but also in a high risk of failure group. We have to be very careful with that. You never want to see a patient on a tidal volume this high.
- Patients can be combative with very high anxiety, Ativan or other medications can be considered; however, they can cause adverse effects including hypoventilation and nausea.
- Heated High Flow Nasal Cannula can also be considered for ‘comfort” (no mask) and the ability to use high FI02 and flow rates up to 60L/M (device dependent)
- Patient also maintains the ability to cough and clear secretions in the event pulmonary edema are overwhelming
Patients can also be very combative and high anxiety. You may want to talk to the provider to see if they have an existing order for Ativan or something to relax them as long as it is not making those patients hypoventilate or nauseated. Once in a while, I resort to medications, but most of the time, I can talk them down. "It's you and me together. I'm going to help you. You have to trust me." You have to talk to them on layman's terms. You cannot use medical jargon to communicate with these patients. You have to keep it as simple as possible.
If they still cannot tolerate it, you can try a heated high-flow nasal cannula. I will discuss this a little later. You have to know all the tools in your toolbox and what other things you can utilize to help these particular patients out. If you do use a heated high-flow nasal cannula, one of the great things, especially with clients that have pulmonary edema, their mouth is clear so they are able to cough and clear secretions. Many times, the pressure, that we are giving with CPAP and non-invasive ventilation, helps push that fluid out of the parenchyma, and the patients stop producing so many secretions. It depends on the level of pressure that you are using. A heated high-flow may be a good choice for those patients.
CPAP Weaning
The decision to wean a patient from CPAP is determined by the following:
- Improvement in hemodynamics
- Positive response to diuretics (or completion of dialysis)
- Improvement in breath sounds
- Resolution of productive cough
- Successful weaning of FI02, CPAP level or both
- Ability to tolerate a trial off mask ventilation without a significant increase in work of breathing or recurrence of hypoxia
When we wean a patient, we have to monitor them. Do they look better? Are they doing better? Is there considerable improvement from when they first came in? Has their hemodynamics improved? If it is congestive heart failure or pulmonary edema and they have been receiving Lasix, have they had a positive response to that? Did they receive their dialysis? How are their breath sounds? What are you seeing as far as their productivity with their cough? Has that pulmonary edema gone down quite a bit? Were we able to successfully wean our CPAP and FiO2 down? Are we down below 50%, 40%, 30%? Can we now manage them off of non-invasive ventilation with standard oxygen therapy? Ultimately, it is important to give them a trial off and see how they do. Sometimes, they do really well. We can then just put them on a cannula. The other thing is that once a patient starts asking me for things to eat and drink, I know I have done my job. However, they may be off for a little while and you may see issues coming back. At that point, go ahead and put them back on as they are not quite ready. Patient assessment is instrumental.
BiPAP (Two Levels of Positive Airway Pressure)
Definition
- Like CPAP patient selection is based on the strongest evidence
- Acute Exacerbation of COPD
- Acute Respiratory Failure with PH <7.35, PaC02 >45mmHg
Now, let's talk about BiPAP. We are going back to our pressure-time scalar so you can see that there are two levels of support. You have the EPAP or the expiratory positive airway pressure, and the IPAP, inspiratory positive airway pressure.
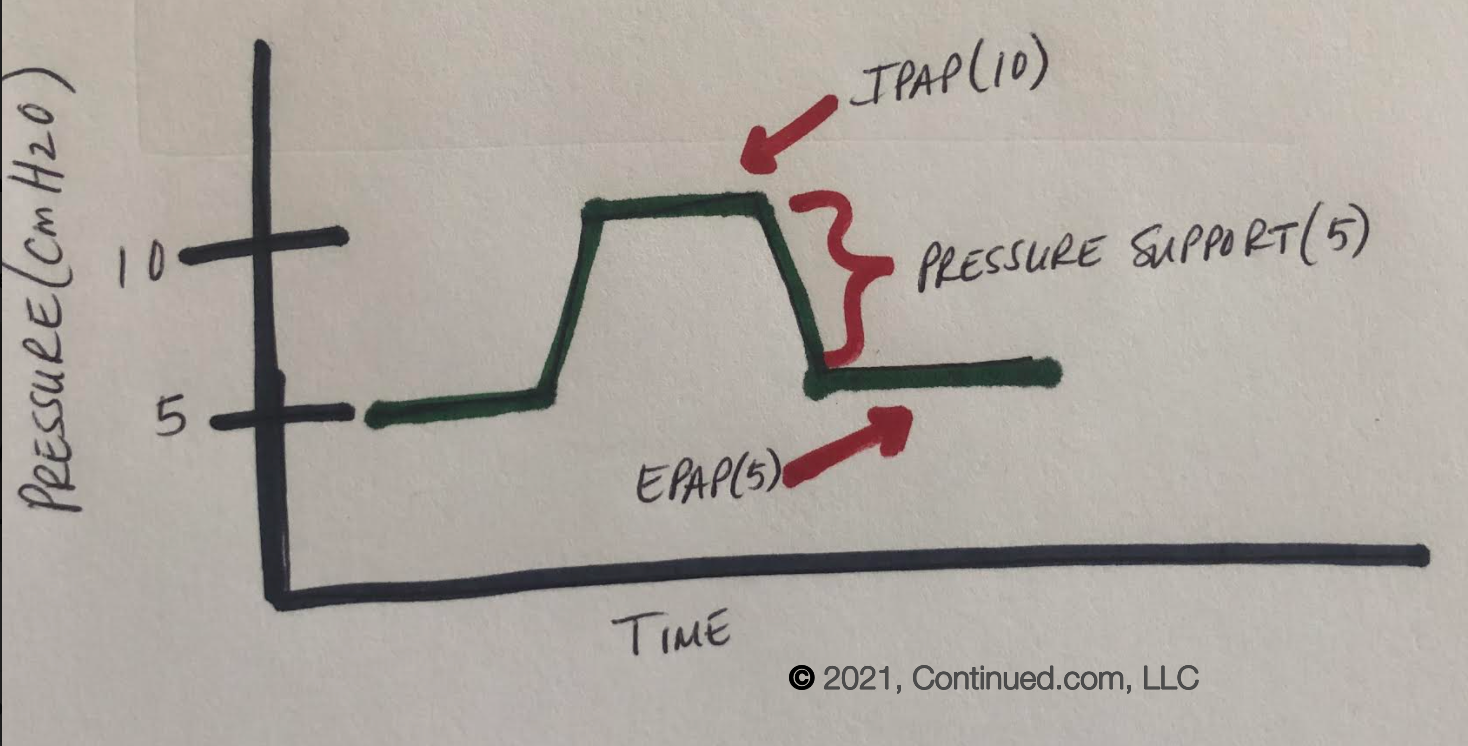
Figure 2. Airway pressure support with BiPAP. (Adapted from Britt, 2017).
For BiPAP, providers order eight over four, 10 over five, 12 over six, or whatever. For example (as shown in Figure 2) if the max pressure is 10 and the minimum is five, the difference between the two is the level of pressure support. In this example, I would have pressure support of 5 for this particular patient. Every time the patient takes an inspiratory effort, you go up to your IPAP level of 10, then when the patient spontaneously exhales, they do not go any lower than five. The pressure support is there every time. Remember, this is a spontaneous inspiratory effort. We are not mask ventilating nor are we setting a rate. Every time the patient takes a spontaneous breath, up to 10, they are getting the five of pressure support. They are never falling below that five on their EPAP. As with CPAP patients, the selection is based on strong evidence. This shows that the best pathology to use for BiPAP is an acute exacerbation of COPD. These are patients that are presenting with acute respiratory failure and usually have a pH of less than 7.3 and a PCO2 greater than 45.
- Patients with PH <7.25 should still be considered to avoid ETI (endotracheal intubation) these patients are at greater risk for failure if not monitored closely
- NIV (BiPAP) is NOT recommended for acute exacerbation of COPD who present with hypercapnia without acidosis
- Target should be a lower oxygen saturation (88-92%) as Hyperoxia in this patient population can be the catalyst for acidosis and elevation of PC02 above the patient's “normal” range
Even patients with a very low pH, 7.25 should still be considered to avoid endotracheal intubation at they are at greater risk for failure if you do not monitor them closely. For example, let's look at a COPD patient that has frequent exacerbations and has been on non-invasive ventilation. Every time we intubate them, they run the risk of not being extubatable. We need to give them a chance.
Non-invasive ventilation BiPAP is not recommended for an acute exacerbation with hypercapnia without an acidosis. You can have a patient that comes in with a COPD exacerbation, but when you draw a blood gas on that patient, they may have a high CO2, but they are corrected. If the pH is within a normal range, you can look at their bicarb. This would be a fully compensated patient. We do not want to now uncompensate them and put them on a machine that is going to change where they live normally. We can address their work of breathing and add bronchodilators, but they may not necessarily need non-invasive ventilation. If their condition changes, their CO2 starts going up, and now the pH is becoming acidotic, then we can consider non-invasive ventilation. These patients often have a hypoxic drive and can tolerate a lower saturation. Thus, we do not want to give these patients more oxygen than what they need because this can be a catalyst for acidosis and elevate their PCO2 if we take them out of their normal range.
BiPAP Treatment
- Work of breathing in these patients is directly related to the degree of obstruction, air trapping, and the amount of time of accessory muscle usage from the onset of exacerbation
- Decreasing work of breathing
- Increasing Tidal Volumes and decreasing respiratory rate while correcting hypercapnia and “normalizing” pH
- Patient comfort and synchrony
- The use of anti-anxiety medications should not be discouraged provided they do not suppress respiration
- Patients must be closely monitored for signs of improvement or deterioration
- Aggressive alternative therapeutics must be also considered if signs of infection are present
- For example Solumedrol, bronchodilators, antibiotics
The work of breathing in these patients is directly related to the degree of obstruction and air trapping. They have a lot of accessory muscle usage, right from the onset of that exacerbation. Our goal is that we want to decrease this work of breathing. We want to increase their tidal volume, decrease their spontaneous rate, and correct that hypercapnia while normalizing their pH. Remember, we do not want to make it normal per our normal; we want to make it normal for that particular patient. Anti-anxiety medications should not be discouraged in a patient that already uses anti-anxiety medications, but we do not want the medication to suppress respiration. Patients should be closely monitored. Keep your eyes on these patients. We also want to aggressively treat them with any therapeutics, like Solu-Medrol, bronchodilators, and antibiotics. You have to hit them and hit them with these treatments because we want to get them turned around. We do not want to leave them on non-invasive for a long period of time.
BiPAP Parameters
Mode is Chosen, Where Do We Start?
- Like CPAP it is always best to start out with lower pressures and low delta and quickly titrate as the patient acclimates to therapy
- Typical BEGINNING pressures 8/4, 10/5, 12/6 (minimum Delta P is 4cmH20)
- Avoid hyperoxia, especially in exacerbations that lack hypoxemia
- EPAP levels are titrated to assist with airway patency elimination of trapped air, not necessarily oxygenation
Where do we start? It is no different from CPAP. You have to start out with lower pressures and titrate up. You have to look at the equipment that you use and your manufacturer. The minimum delta pressure is four centimeters of water. Between that IPAP and that EPAP, that minimum delta should be four. Start out low, and we are going to titrate up. You should be titrating immediately. If you started at eight over four and the patient does not look any better and there is no big change in their minute ventilation, you can start titrating up right away. What you want to see is a respiratory rate that comes down, a tidal volume that goes up, and a resolution of that minute ventilation. You want to see everything look better and you want to see them start to relax. That is the key. Again, we are going to avoid hyperoxia, especially in patients in an exacerbation that are not hypoxemic. We can titrate EPAP levels to assist not only with airway patency but also the elimination of that trapped air. You want to open up those airways and get some of that trapped gas out.
- IPAP levels are titrated to adequate (lung protective) tidal volumes, decreasing respiratory rate and work of breathing while maintaining adequate minute ventilation for correction of PC02
- Blanket orders for these patients are not appropriate and titration must be performed on every patient based on need/response to therapy
- If a patient does not appear significantly improved after initiation and titration of NIV, assess the need for pharmacologic therapy, further adjustments in settings, address synchrony, or anxiety.
- If the patient condition does not improve or continues to decline, do not delay in initiation of IMV
IPAP levels are titrated. You have to keep the lung-protective strategies in mind. We want to increase tidal volume, decrease that rate, and again, maintain adequate minimum ventilation for clearance of that CO2. Blanket orders in these patients are not ever appropriate. This is where the knowledge level of the provider is important as they have to give you an order. We cannot do things without orders unless you have a protocol that states you can. Ultimately, we are going back to our providers and telling them where our patients are and what we have set them on. They may tell you to put a client on BiPAP and then just pull some numbers out of the sky because they have to write something. They may say, "Start the patient on 12 over five, and let's get a gas in an hour and see how they do." Well, if I start a patient on 12 over five, and the patient does not look any better than they did before I put that mask on them, what do you think is going to happen in an hour? They are going to still be breathing exactly the same as they did before. Their minute ventilation will be out of control with a horrible tidal volume. I am going to get a blood gas measurement in an hour, and they are going to say that non-invasive ventilation failed. They are then going to want to intubate the patient. They had to write an order and come up with something. However, if a clinician puts a patient on non-invasive ventilation, and they do not look any better after an hour, that is not enough. They have to titrate those patients up by increasing IPAP to get a better tidal volume and do all those things I told you to do before. Pay attention to the patient. How do they look? When they start looking better, smiling, and giving you the thumbs up, then you know you have done your job. You cannot (and should not) with good conscience put a patient on a blanket order and walk away.
If they do not appear significantly improved after initiation, you have to do something more. Give them their treatments and titrate those pressures. If there are synchrony issues or anxiety, you have to address all of those things before you step away. If the patient's condition does not improve, we have to be the ones to go to the provider and say we are not going to win this one. We cannot delay the initiation of invasive mechanical ventilation if that is what that patient truly needs.
- Patients are closely monitored
- Mask fit, comfort, and patient synchrony are crucial for success
- Respiratory rate and inspiratory time are “settings” but only backup rates – They are not “synchronized” to spontaneous breaths, not guaranteed and are only active if the patient's spontaneous breaths taken by the patient fall below set parameters.
- For example:
- The set rate is 8, the patient’s spontaneous rate is 10 – ZERO breaths are “delivered by the ventilator
- The set rate is 8 patient’s spontaneous rate is now 4, there are 4 additional “breaths” delivered by the ventilator
- For example:
Mask fit, comfort, and synchrony are all crucial for success. If any of these fail, your patient is not going to do well. On some equipment, there are respiratory rates and inspiratory time settings, but these are only for backup rates. They are not synchronized like on a ventilator to any spontaneous breaths and are not guaranteed. They are only active if your patient stops breathing. For example, if I set a rate of eight and the patient's spontaneous rate is 10, no breaths are delivered by the ventilator. They are all patient spontaneous breaths. However, if I set a rate to eight and the patient has episodes of apnea with a spontaneous rate of four, four of those breaths are going to be delivered by the ventilator and four are going to be the patient's spontaneous breaths. Is this a good thing? No, and you should be doing something about that. You have to understand every piece of equipment to use it properly.
- If the patient is not improving within the first 1-3 hours or becomes less responsive, initiate NIV
- Titrations may include changes in EPAP for oxygenation issues or attempts to open airways
- Tidal volume titrations are the resultant of IPAP increases (Delta P)
- In the event of EPAP increases, IPAP needs to be increased in the same increments if Delta P is adequate (Decreasing the Delta P would result in a decrease in Tidal Volume)
If your patients are not improving within the first one to three hours and they become less responsive, then we have to consider invasive mechanical ventilation. Titrations that you will make may include changes in EPAP for oxygenation or attempts to keep those airways patent. Tidal volume titrations are a result of that delta pressure. If you are increasing or decreasing the other parameters, but want to maintain that delta pressure, you have to remember that you have to increase either your IPAP or EPAP levels in the same increments. For example, if you like where your delta pressure is and increase EPAP by two, you may need to go up on the IPAP by two to maintain that delta pressure between the two of them.
Closed Loop Ventilation
- AVAPS = average volume assured pressure support (Phillips V60 ventilator)
- A positive pressure mode with a volume target
- Pressure limits are set (high and low limits) with an average tidal volume “target”
- Primary use ALS, neuromuscular patients, patients with normal/near normal lung compliance, also used in COPD exacerbations.
- Cautionary usage in patients with low lung compliance. Patients with decrease compliance where upper pressure limitations have been reached, LOSE tidal volume that can no longer be guaranteed
- Other examples of Closed Loop Ventilation include:
- Proportional Assist, NAVA, MCC, Intellivent ASV, Smart Care
- There is no supporting evidence for the use of closed loop ventilation in acute NIV
Some facilities use an automated mode. One of them is on the Phillips V60 ventilator called average volume-assured pressure or AVAPS. It is a pressure mode with a volume target. You are setting high and low-pressure limits, and you are telling the machine the volumes you would like to get (e.g. 415 ml). The machine will titrate the pressures up and down to guarantee you a certain tidal volume. Its primary use is for ALS and neuromuscular patients. I would use it with caution in these patients because a COPD patient in exacerbation has very low lung compliance. Depending on where you are setting your upper pressure limit, if the patient's lung compliance changes or gets worse and you hit that upper pressure limit, you are no longer guaranteed that volume. And, if you have stepped away or have not seen that patient in a while, you may have lost that tidal volume (unless you have set an alarm on that piece of equipment). You may lose the tidal volume, and your patient might not be doing as well as you thought they were. I would caution usage in automated modes.
There are other things on ventilators besides closed loop. There are proportional assist, NAVA, MCC, Intellivent ASV, and Smart Care. This is all for another lecture. We are going to stick primarily to CPAP and BiPAP. I just wanted to mention it for informational purposes. There really is no supporting evidence out there right now for the use of these automated modes in acute non-invasive ventilation.
BiPAP Weaning
Key points:
- Improvement in ventilation
- Improvement in breath sounds (increase in aeration, may or may not hear more pronounced wheezing, but will hear improved airflow)
- Improvement in blood gases
- Improvement in use of accessory muscles
- If tidal volumes have increased, IPAP and EPAP pressures need to be titrated down or the patient is given a trial off
- If the patient still requires BiPAP (needs more time) titrate pressures down and continue therapy, monitoring frequently
How do we wean? The same way we wean CPAP. Does your patient look better? Is there an improvement in ventilation, breath sounds, or blood gases? How is their accessory muscle usage? If all looks good, give them a trial off. You can either wean them down on their pressures or just pop the patient off and look at them. Ask them how they feel. How are you feeling? Are you feeling better? Do you want some of those Lorna Doones in that snack pack? You may know it as soon as you take them off for a trial, or you may need to check on them in a half-hour to an hour to see how they are doing. Frequently, they may need to go on and off, but that is okay. You are still making progress.
Caution! Do not allow patients to over ventilate or overcorrect blood gases!
- COPD patients present with compensated respiratory acidosis (elevated PC02 and HC03 with normal PH)
- When overcorrected COPD patients may have apnea episodes or drop their spontaneous rate (less triggering)
- Assess patients to make sure they remain rousable, if so- wean settings or trial off. If not, prepare for intubation and IMV
Do not allow these patients to over ventilate. We can over-correct their blood gases and when we do. A COPD patient absolutely loves to not have to work to breathe. As they improve, remember, they are on non-invasive ventilation and we are supporting them. If I have a tidal volume that was averaging around 450 and I see they are moving toward 6,700 ml of volume, I know they are doing a lot better. However, I do not want them to continue breathing like that because I am going to over-correct their CO2 and may head toward the alkalotic side. When a COPD patient does that, they start going into apnea. They have little apnea episodes, and they now are sleeping like babies. They love it. If you go back to your patient and they are snoring away, but you are seeing high volumes, you have to make sure those patients remain rousable. Every time you assess your patient, give them a little shake. If they wake up right away, they are still rousable, then I know that I have over-corrected and it is time to wean or give them a trial off. If I am rousing the patient and they are not waking up, they may have gotten worse. Now, I have to think about preparing to intubate that patient. Over-ventilation is not good either, and they are pretty acute at that point. They get disappointed then when I tell them that they have to go back to breathing on their own.
Synchrony Adjuncts
- Rise time/slope – can be adjusted to patient comfort
- How fast or slow pressure is achieved during the patient's spontaneous breath
- E Cycle, % Inspiratory Flow Termination, Cycle Off
- Ventilators are preset to terminate inspiratory flow at 75% (25% remaining) of PIF (peak inspiratory flow) can be adjusted based on each patient
Many ventilators for non-invasive protocols have synchrony adjuncts with rise times/slope that can be adjusted for patient comfort. Typically, a COPD patient likes to feel the air going in very rapidly. You can adjust that rise time as to how fast or how slow that ventilator is going to reach that pressure during a patient's spontaneous breath. The other thing is the E cycle or the percent of inspiratory flow termination or cycling off can be adjusted based on each patient.
- Easily identified in Pressure/Time Scalars as a “peak” and pressure overshoot at the beginning of exhalation.
- V60 ventilator has a C flex option for CPAP
- A deceleration of flow and slight “dip” in CPAP pressure of 1, 2, or 3cmH20 during exhalation
- Ramp option
- Should not be used in acute NIV, reserved for slow, timed, “ramp” to pressure while a chronic NIV patient falls asleep (in some equipment ramp times are up to 45 minutes)
This is a free article where you can see a pressure-time scalar (Gentile, 2011). I am not looking at the inspiratory portion of the breath, but rather I am looking at the expiratory. You can see a little pressure overshoot in the graphic in Figure 3.
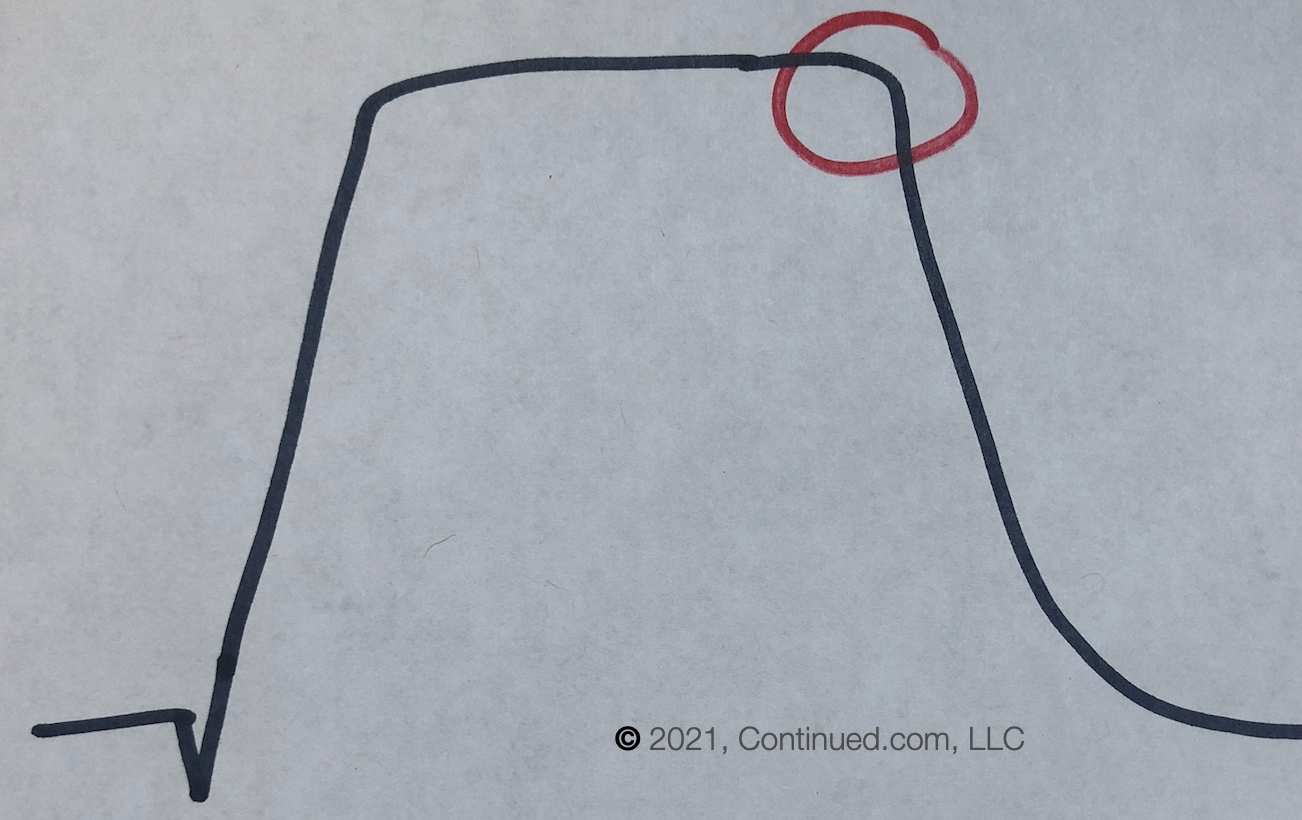
Figure 3. Asynchrony at the transition to expiration (Adapted from Gentile, 2011).
When that pressure overshoots at the end of the breath, that means the patient is actively exhaling or pushing against that flow that is contiguous. You can change that as you do not want your patients actively exhaling.
The V60 ventilator has something called a C-Flex option for CPAP, so that decelerates the flow and gives a little dip in that CPAP pressure of either one, two, or three centimeters of pressure, only during exhalation. It decreases a little bit and dips into that CPAP. You can choose one, two, or three, and it allows that patient to more passively exhale to get a little break from that constant flow.
On some equipment, you are going to see an option called ramp. This is used for chronic patients to ramp up pressure for 45 minutes while the patient is falling asleep. It starts out very low and over 45 minutes, it gradually goes up to their ultimate therapy pressure that was prescribed by the sleep doctor. You never want to use this ramp option in an acute patient. It that option is there, ignore it.
There is a graph in the above-referenced article where you would see that pressure overshoot on the E cycle. This is where the ventilator now is transitioning flow into exhalation. In the chart, you can see at 10% that the breath is essentially over. Then, you have exhalation at 25% and at 50%. You can change that based on where your patient is and matching that to what the patient is doing. If you see that pressure overshoot or active exhalation, sometimes I put my hand on my patient's abdomen to see if I can feel their diaphragm contracting during exhalation or to feel if they are bearing down (pushing against that flow trying to exhale). If you have this option and activate it, you can examine your graph to see if you need to make any further adjustments to get them to relax. Ultimately, you do not want to feel active exhalation in these patients. It is a sweet feature on your equipment if you have it and are able to utilize it.
Figure 4 shows a graph of what C-Flex looks like on a piece of equipment. It shows you the flow and pressure dip that you are able to adjust.
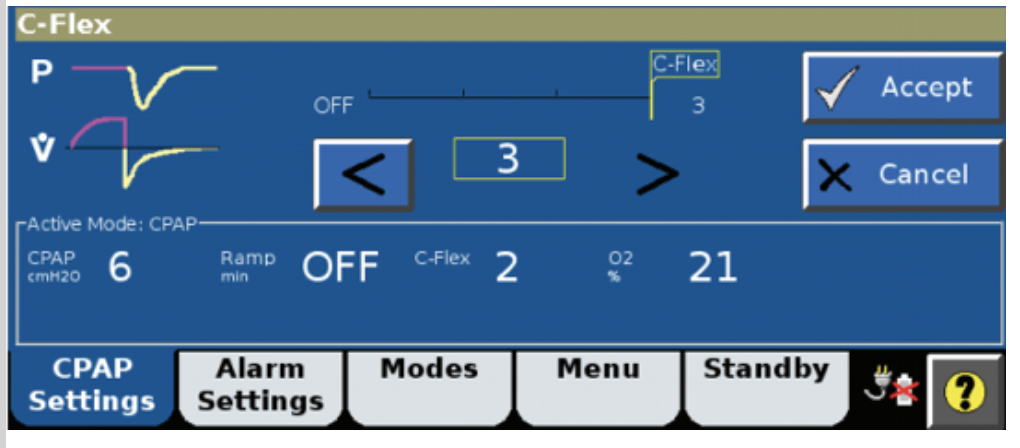
Figure 4. C-Flex option on a monitor.
Equipment
Acute vs. Chronic Non-Invasive Ventilators
There are a ton of different equipment out there (Figure 5).

Figure 5. Types of non-invasive ventilators.
Some are meant for more chronic use. The devices over on the right-hand side are for chronic obstructive sleep apnea patients; whereas, there are a few acute ventilators that are typically only used in hospital ICUs. Not all are appropriate for use in acute non-invasive ventilation, but now many ICU ventilators now are absolutely terrific. They have great leak compensation and non-invasive modes.
Invasive Ventilators
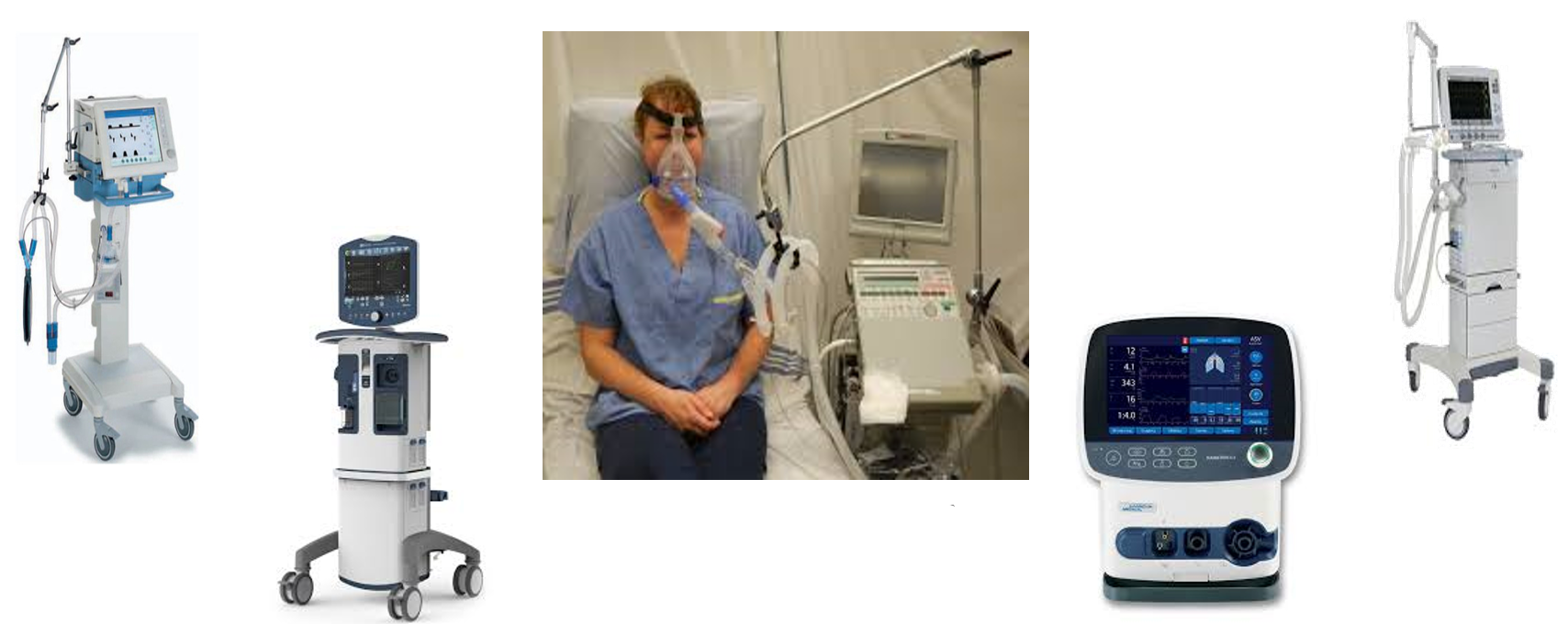
Figure 6. Examples of invasive ventilators.
ICU ventilators for mask ventilation work tremendously well. All of the ones shown on the screen are pieces of equipment that I have at my facility. They all have that percent of inspiratory termination where I am able to do make adjustments during the expiratory cycle.
When we are choosing masks for non-invasive ventilation, they are meant to leak so stop over-tightening them. If you are using a mask and the leaking does not seem to be appropriate, it may not be sized appropriately or the right type. You are running a risk of failure in these particular patients if not fitted appropriately. Each manufacturer and every different mask has different sizing charts so make sure you know that you are fitting your patients properly.
Mask fitting should be an essential part of departmental orientation and instruction. When you are teaching new therapists or providers about non-invasive ventilation, you need to show them how to appropriately size and fit a mask. We should not be using nasal masks or nasal pillows to treat an acute patient as there is too much air escaping through the patient's mouth, even if you are using chin straps. With leaks, the tidal volume and minute ventilation variables are too great. Unfortunately, for acute non-invasive ventilation, you want to stick to a full face mask. If your patient is going to be on non-invasive for a longer length of time, you have to monitor their skin integrity. And if your patient cannot tolerate a full face mask, you can try to use a heated high-flow nasal cannula.
Mask Choices
- When treating patients for acute hypoxic or hypercapnic failure you should only use full face or total face masks.
- The goal is to have a minimal leak and to maintain both pressures and volume
- Each manufacturer has different sizing charts and proper mask “fit” should be part of departmental orientation and instructed for each type of mask available
- Nasal masks or nasal pillows allow to much air to escape through the patient’s mouth, even when chin straps are used. This leakage makes tidal volume/minute ventilation too variable
- If
