Introduction
The coronavirus, COVID-19, is presenting new unique challenges to our workforce. We are all navigating unchartered waters making it important for all of us to find new ways to work and interact all the while taking care of our own mental health and well-being. Many of us are teleworking for the first time. We are isolated from coworkers, friends, and family. Even if you are going into a community and working, let's be honest, our daily living routines are disrupted. This causes anxiety, stress, and strain physically, mentally, and financially.
What to Expect
- Anxiety, worry, or fear about your health or the health of others
- Resentment by you or family/friends
- Worry about time away from work, loss of income, job security
- Worry about the challenges of securing things you need
- Concern
- Uncertainty
- Loneliness
- Anger
- Boredom
- Frustration
- Symptoms of depression
We are talking about COVID-19 right now, but this could apply to any sort of serious health crisis or infectious disease outbreak. Obviously, during this period, everyone is going to react differently to social distancing, quarantine, and isolation. You might feel anxious, worried, stressed, and have fear related to your own health or the health status of those who you may have exposed to a disease. You may have to deal with the resentment of your friends and family that feel that they need to go into quarantine as a result of contact with you. The experience of monitoring yourself or being monitored by others for signs and symptoms of the disease is not comfortable. How fun is it to have your temperature taken every time you go into work? You may be concerned about time off from work or the potential loss of income and job security. There also may be challenges with securing things that you need like groceries and personal care items or concerns about how to effectively care for your children or others. There can be uncertainty and frustration. How long are we going to need to remain in this situation? What does the future look like? There can be loneliness associated with just feeling cut off from the world and loved ones. You may experience anger if you think you were exposed to the disease because of someone else's negligence. There can be boredom and frustration because we cannot engage in our regular day-to-day activities. You may have a desire to use alcohol or drugs or even overeating to cope. We can experience symptoms of depression, helplessness, sleeping too little or too much, and changes in appetite. This may be a little out of the scope of this, but trauma-informed care may apply here as well because we are going to see symptoms of post-traumatic stress disorder (PTSD), intrusive memories, flashbacks, nightmares, etc.
Quarantine
During the coronavirus outbreak, quarantine has been used as a public health strategy to reduce disease transmission. The efforts have ranged everywhere from the mass quarantine of entire cities, for example, in China, to isolation in government-run facilities, to our own self-isolation at home. And while it broadly serves a public good, it is also associated with psychological challenges.
- Stressors during quarantine include:
- Frustration and boredom related to the isolation of quarantine, which involves loss of one’s usual routine and limited social and physical contact with others
- Inadequate supplies and access to services
- Insufficient information
- Longer durations of quarantine
- Fears about becoming infected and/or infecting others
We already touched on some of these. There can be frustration and boredom due to the loss of our normal routines and limited social and physical contact with other people. Inadequate supplies and access to regular medical care can be stressful. Medical care has changed with many of us seeking medical care via telehealth or some sort of virtual appointment. We may have inadequate supplies such as food and water. Medical supplies and personal protective equipment (PPE) have been in short supply as we know, but it also may be difficult to secure other supplies such as prescriptions and thermometers. I do not know if anybody has tried to get a thermometer during this time, but it is very difficult. There can also be insufficient or delayed information from public health authorities. Guidance can be unclear. I think the flip side is also true. While there is insufficient information on one side, there can also be too much information on the other side. There is a lot of negative news, and you really have to dig and search for some of those positive stories. There is a lot of fear and uncertainty raising many questions. How much longer is it going to be? Will it be extended? Finally, there are fears about becoming infected and infecting others. This can be heightened in certain populations like pregnant women, parents of young children, and those living with the elderly.
- Stressors following quarantine include:
- Financial loss
- Stigma from others
- Getting back to one’s “normal” routine
The quarantine will be over at some point in time, but most likely there will be stressors following the quarantine as well. If you are furloughed or have been laid off, there can be financial stress and loss that will extend past the quarantine. There can be increased health care costs and unanticipated financial burdens can all impact our stress. There can be stigmatization and rejection by neighbors, coworkers, friends, and family members. You might be treated with fear and suspicion. You might be excluded from things like leisure, work, or social activities and that can be exacerbated particularly if quarantined individuals are members of a particular ethnic or religious group. Getting "back to normal" could take several days, weeks, or months. And, getting back to that normal can be met with concern, anxiety, and frustration. I think a lot of people think, "We are going to just flip the switch and go back to normal," but that is not the case. I think it really depends on how disrupted your life has been. For example, if you have always worked from home, maybe you do not feel so disrupted. However, if you are working on the front lines, that is very different. Getting back to normal will take a little bit more time.
- Well-being during quarantine:
- Use communication as an intervention
- Facilitate communication with loved ones
- Prepare for quarantine
- Reduce boredom and isolation
- Take care of yourself
What can you do for your well-being during quarantine? Use communication as an intervention. The more we can communicate, the better our behavioral adherence is to quarantine. This is not just with the patients that you are working with, but this includes your family, other staff, and your children. It is important that other people understand why we are doing what we are doing. Additionally, if you know your loved ones are safe and healthy, this will also reduce your stress. If at all possible, before you go into a full-blown lockdown quarantine, give people time to make arrangements, reassure loved ones, and make sure that everything is in order. And of course, during the quarantine, facilitate the use of technology and other ways to stay connected. As we are in the throes of this, we can still figure out what is available, who is delivering, who is open, and who has special hours maybe for healthcare workers or for the elderly. Again, to reduce boredom and isolation, look for activities via the Internet or social media but use it with caution. If we expose ourselves too much, it can actually increase stress when inundated 24/7. Now is the time to tap into your hobbies, find activities, keep your mind sharp, stay busy, and take care of yourself. We will talk more about this, but make sure that your own basic needs are met: eating, drinking, sleeping, and taking breaks. I think you need to also take the time to talk to your family and your children to educate them about the risk and the steps that you are taking. You might help them to reduce their stress as well.
Understand the Risk
- Stay up to date on what is happening, but limit media exposure
- Avoid watching or listening to news reports 24/7 since this tends to trigger or elevate anxiety, stress, panic, and worry
We need to understand the risks of harm to yourself and others around you. Media coverage may create the impression that everyone is in immediate danger when really the risk for infection may be lower. Or, it can be the opposite. It may be portrayed as everything is ok when it is not. Get the facts. Knowledge is power, and it is good to stay up-to-date. However, avoid watching or listening to the news 24/7 because it can trigger or elevate anxiety, stress, panic, and worry. Research has shown that excess media exposure to coverage of stressful events can actually result in negative mental health outcomes. Use trusted media outlets and also look for those positive stories about recovery.
Maintain a Routine
- Create and maintain a routine and schedule
- Structure will help you to cope
Another important thing that we need to do is maintain a routine. Whether you are working from home or going out every day to work in a hospital or a clinic, keep to the best of your abilities a regular schedule. If you are home, set up a designated space for you and your family members to work or learn. Make sure that you have periodic breaks for recharging. Everybody is going to be different. I know I am working from home right now and have my whole family under one roof. We get up at a certain time and are trying to stay on task. We have breakfast. We start doing some of our work. We break for lunch and have an activity in the afternoon. Having that structure helps you to cope and stay sane. If you are working from home, there is a tendency to work a lot. You have to, at some point, shut it down and make time for you to do something that is all about you. If you are working at a center, it is also important to establish those routines and stick to them while allowing for self-care.
Dealing With Stress
How do you deal with stress? Think about what we do as OTs. We have a strong service orientation. As such, we often have difficulties acknowledging our own needs due to a lack of time or fear of being removed from our duties at work. All of those things may prevent each of us from speaking up and saying that we have stress. In addition, during this time, employers are trying to be proactive and encouraging. In order for all of this to work, the environment needs to be free from stigma, coercion, negative consequences, and negative reprisal if we do speak up about being stressed.
Looking from our side, as nurturers, we tend to prioritize everybody else over ourselves. A self-care strategy can give us a sense of control and give us a sense of contribution without making us feel unrealistically responsible for everyone around us.
During work shifts:
- Self-monitoring and pacing
- Check-ins with colleagues, family, and friends
- Working in partnerships or in teams
- Brief relaxation/stress management breaks
- Time-outs
- Keep anxieties conscribed to actual threats
- Helpful self-talk
- Focus efforts on what is within your power
Accept what you cannot change
We will talk more about this as we go along, but self-monitoring and pacing are really critical. Check-in with your colleagues, your friends, and your family. If you can, even though you are working physically apart, work in partnerships or teams. Share the workload. Relaxation, stress management breaks, and timeouts need to built into the day. Keep your anxieties to actual threats, not perceived threats. Focus on what is within your power and accept what you cannot change. I firmly believe that you cannot necessarily choose what is happening to you, but you can certainly choose your attitude and how you are going to address and respond to it. We need to foster amongst ourselves a spirit of fortitude, of patience, of tolerance, and we will talk a little bit later of hope.
- Avoid
- Working too long by themselves without checking in with colleagues
- Working “round the clock” with few breaks
- Feeling that they are not doing enough
- Excessive intake of sweets and caffeine
- Engaging in self-talk and attitudinal obstacles to self-care
At the same time, avoid working too long by yourself without checking in with someone. You may be working around the clock and feeling like you are not doing enough. "My colleagues are doing all of this, and I am not nearly doing that." It is not a contest. Avoid excessive intake of sweets and caffeine. They may be great at the onset, but that crash later is never so good. Engage in helpful self-talk, but avoid attitudinal obstacles like "It'd be selfish of me to take a rest. Others are working round-the-clock so I should be doing the same." Or, "The survivor's needs are way more important than mine." Now is the time to call upon your colleagues, give up the total power and control, and share the workload.
Stress Management
General
- Be prepared
- Take everyday preventive measures
- Maintain a healthy diet and exercise regimen
- Talk to loved ones about worries and concerns
- Engage in hobbies and activities you enjoy
It is not too late to look at a personal or a family preparedness plan. Take every day preventative measures. This includes hand sanitizer, PPE, frequent hand-washing, and the like. Maintain a healthy diet and exercise regimen, and we will discuss this more shortly. Talk to your loved ones because they probably are sharing your worries and concerns. And again, find things that you enjoy. I saw somebody post to social media, "Seems my only hobbies are eating out, shopping, and spending money." While I got a chuckle out of that, you should try to find something that you enjoy and make time for it. There is a saying, "The other 23." You have 23 other hours in the day to do whatever else you need to do. Set aside one hour for you and your own health and wellness.
Basic Stress Management Techniques
Let's now look at some very basic stress management techniques.
- Relax your body often by doing things that work for you
- Pace yourself between stressful activities
- Talk about your experiences and feelings to loved ones and friends
- Maintain a sense of hope and positive thinking
Relax your body. Take deep breaths, stretch, meditate, pray, and engage in activities that you enjoy. A lot of this takes mere minutes. It only takes one or two minutes to do some deep breathing exercises or five minutes to do some decent stretches. Pace yourself between stressful activities. After you have done a really hard task, maybe do something fun or take a little break. Again, talk about your experiences with other people. Maintain that sense of hope and positive thinking. Journaling can be nice as well. Right now we have reduced access to food, gyms, sporting activities, and bars, and restaurants, but we have more control over our stressors than you think. Again, it is easy to use meditation and deep breathing. We can practice gratitude. I am a firm believer in the FISH! Philosophy in management. One of the principles is, "Make their day." There is a way that we can give to each other during this time, and that makes it so much easier for all of us.
Stress Relievers That You Can Do At Work
- Progressive muscle relaxation
- Visualization
- Deep breathing
- Engage your senses
- Laugh
- Practice makes perfect
There are some simple things you can do at work. Progressive muscle relaxation can help you to relieve tension in your muscles. Over time you just become so accustomed to your tension, you stop noticing that you are tight. Sore muscles, particularly in your neck and your shoulders, come from chronic tension. With progressive muscle relaxation, it lets go of that tension. Slowly tense and relax your muscles, one group, at a time. Start with your toes, and work all the way up to your neck and then back down again. With some practice, you start to increase your awareness of when you are actually tensing up and you start to let go of that tension.
Visualization is another one. Go to your happy place like a mental vacation whether it is a beach or a mountain. It could also be your favorite chair in your living room. Any place other than work will fit the bill. Close your eyes and spend a couple of minutes there. Do not just visualize it, but you should also engage your senses. In this place, what would do you hear, smell, touch, and taste? Tap into those memories.
Deep breathing is becoming more aware of your breath. This increases the supply of oxygen to your brain and provides a state of calmness. You can really focus your body and quiet your mind. There are one million ways to do this. Some have visualization, and some do not. Some hold it for a count and let it go. I really do not think it matters.
We have already talked a little bit about engaging your senses. The key is to find out what sense is most helpful for you. For some, it is listening to music. For others, it is visual like looking at family photos. Scented hand lotion or sucking on a favorite candy might calm your senses. Figure out something that is easy and simple. Finally, laughter is the best medicine. You have to try to find that silver lining and humor right now. It could be a funny meme, funny photo, or a cartoon. Sometimes this serves as a really good reminder not to take life so seriously. And then, of course, practice makes perfect. The more we practice some of these things, the better we will be at actually doing them, and quickly learning how to reduce our stress.
Simple Stress Relievers
- Start your day off right
- Be clear on requirements
- Stay away from conflict
- Stay organized
- Be comfortable
- Forget multitasking
- Walk at lunch
- Keep perfectionism in check
- Listen to music on the drive home
Start your day off right. There is a reason they say that breakfast is the most important meal of the day. Start the day off with good nutrition, proper planning, and a really good attitude. You might find that the stress just rolls off your back if you do. Be clear on requirements. Try to stop from falling into a trap of thinking that you are not doing enough. Talk to your supervisor and make sure that you are clear on your requirements. Stay away from conflict. It is harder now than ever, but try to avoid those conflicts. Do not gossip or share too many personal opinions. Steer clear of the things that you know are going to cause conflict. Try to stay organized. This can get a little tough when we are all under one roof all day long. The more organized you can be, the less stress you will have in other places. Along with this, stick to a routine as well. If you are set up for success, small things that can be distracting or cause frustration like noise or lighting might not be an issue. Forget multitasking. I think we learned this a long time ago. Try chunking or doing dual-tasking because that will certainly relieve stress as well. Walking at lunch and getting some fresh air can be a game-changer. If you cannot get outside, the simple exercises I am going to share with you can help. Keep your perfectionism in check. Again, you might feel good about yourself, but being a perfectionist can drive you crazy. This can also drive the people around you crazy as well. Try to give up that control.
Simple Yoga Poses
Some things that you can do include yoga poses. Figure 1 shows the seated crescent moon pose.

Figure 1. Example of seated crescent moon pose (Image ©2020 continued, LLC).
Lift your arms overhead. Stretch your fingers wide and lean to the right, taking two or three deep breaths. Switch sides and do the same thing. Figure 2 shows a seated backbend.

Figure 2. Example of a seated backbend (Image ©2020 continued, LLC).
You are going to reach all the way up to the ceiling with your arms open wide. As you exhale, start to look behind you and bend slightly from your upper back and your chest, putting your arms behind you. Hold it for a few seconds and then let it go. Wrist and finger stretches are shown in Figure 3.

Figure 3. Example of finger stretches (Image ©2020 continued, LLC).
This is particularly helpful if you are working at a desk quite a bit. Do some wrist circles, spread your fingers, and open and close your fists five or 10 times to reduce some stress. The next position is called a seated twist in Figure 4.

Figure 4. Example of a seated twist (Image ©2020 continued, LLC).
For this, you sit tall in your chair and inhale and then twist to one side from the bottom of your spine. This is moving more from your abdomen versus your back. Then, grab your armrest or the side of your chair, breathe in, and then go to the other side. Figure 5 shows the chair pigeon pose.

Figure 5. Example of the chair pigeon pose (Image ©2020 continued, LLC).
You start with your feet on the floor. Cross one leg over the other at a 90-degree angle, and then stay in an upright seated position. Twist a little if you can. You should feel a gentle to moderate stretch on the thigh, and you hold that again five or 10 breaths and move to the other side. The sit-to-stand pose can be seen in Figure 6.

Figure 6. Example of the sit-to-stand pose (Image ©2020 continued, LLC).
In this one, you start at a seated position, and you try to stand up just by pushing down through your heels and not using the arms and not leaning really far forward. Then, as you sit down, you are doing the same. Completing this exercise 5-10 times will really help to awaken those leg muscles. Figure 7 shows a desk upward dog pose.
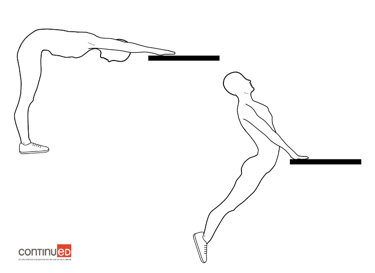
Figure 7. Example of a desk upward dog pose (Image ©2020 continued, LLC).
With arms straight, you lower your hips toward the desk refraining from sinking in the lower back. Then, stretch your chest between your shoulders. Gently lift up your chin and hold it for five or 10 breaths. Finally, Figure 8 shows a forward fold.

Figure 8. Example of a forward fold (Image ©2020 continued, LLC).
Let gravity take over and hold it for about 20 seconds. You are not trying to touch the floor but just going as far forward as you can. You might be thinking that you do not have time for this. However, these only take a few minutes. This is something you can do on a quick break on your way back from the restroom or whatever, and it makes a huge difference in relieving some of the stress that you can hold in your muscles.
Stress Well-Eat Well
- Purchase shelf-stable and frozen foods
- Take inventory of the items in your kitchen and get creative with cooking
- Pay attention to portion sizes
- Stay hydrated
While it is important to minimize your excursions to the grocery store to limit the spread of COVID-19, this may also limit our ability to purchase fresh, healthier food. We can purchase shelf-stable and frozen items to incorporate into recipes. Take inventory of what is already in your kitchen and get creative. Pull out your cookbooks or look online for some fun things to do. We also need to pay attention to portion sizes. As we are cooped up inside, it is easy to overindulge. Try to maintain regular eating habits as much as possible. Minimize your reliance on take-out and drive-through options. It is also important to stay hydrated and drink more water. Always have the water at your desk or water at the ready.
Move Well
- Exercise is critical for both mental and physical health
- Go for a brisk walk or run
- Hop on your bicycle for a tour of your neighborhood
- Try a new activity
- Create an obstacle course at your home
- Invite your kids to get moving
Moving well goes hand-in-hand with eating well. Exercise is critical. Take advantage of what is out there right now. This could be virtual workouts or you could take a walk or a run. Get on your bicycle. I have been out in my neighborhood practically every day. It is amazing how social it has been. Everyone is out and about, and it has been kind of fun. Try new activities. One fun thing with kids is an obstacle course at your house. If you are homeschooling, they need to get PE and you can do that right along with them. Play with your kids. Again, there are a lot of really cool things online. In fact, I have seen runs that you can do through Disney parks while you are on your treadmill. I also saw something where you can virtually hike the Appalachian Trail. It is really up to us to get creative and figure out what is out there.
Resistance Band Exercises
Here are some resistance band exercises. The first one is a lunge with a biceps curl shown in Figure 9.
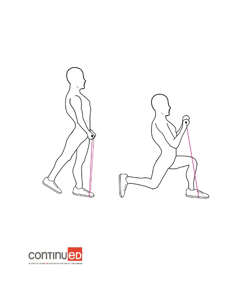
Figure 9. Example of a lunge with a biceps curl (Image ©2020 continued, LLC).
You start in a standing position. As you lunge down into a knee bend, you pull the band up and you are doing a biceps curl. You can do 10-20 repetitions and then switch sides. Figure 10 shows a move called hug-the-world plie.
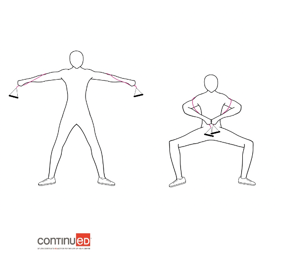
Figure 10. Example of a hug-the-world plie (Image ©2020 continued, LLC).
You stand with your feet shoulder-width apart, and as you complete a "plie" or bend down, you pull the ends of the band together. Your arms are extended and then you bring them in toward your chest. You can do this one 10-20 times. The next one is a squat with an overhead press in Figure 11.
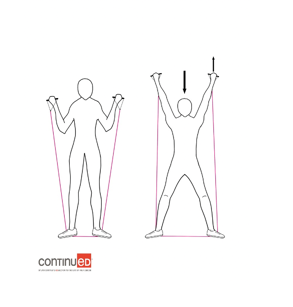
Figure 11. Example of a squat with an overhead press (Image ©2020 continued, LLC).
So you stand in the middle of the band with your feet parallel and you hold the handles at shoulder height. And then as you squat down, you push up. So you're working your arms. You're working your legs. Or you could maybe not work your legs and just work your arms here, and again, 10 or 20 times. Next is a crunch with a lat pull-down in Figure 12.
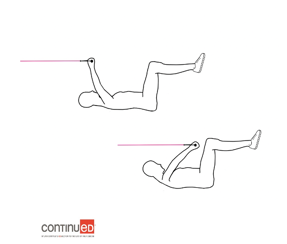
Figure 12. Example of a crunch with a lat pull-down (Image ©2020 continued, LLC).
I would not necessarily advise doing this at work, but you can certainly do this at home. Loop the band around something, and then lie on your back, raise your legs, and perform crunches with your TheraBand or your resistance band while you are moving. Figure 13 shows side lunges with side raises.
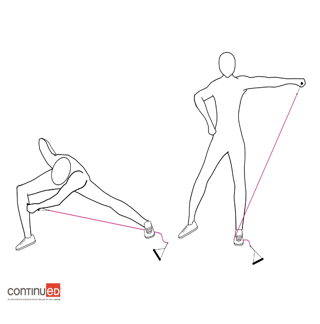
Figure 13. Example of side lunges with side raises (Image ©2020 continued, LLC).
You can see that the resistance band is under one foot. You start in a lunge position, and you are going across the body and coming to a standing position. This works both the arms and the legs. Then finally, we have side bends in Figure 14.
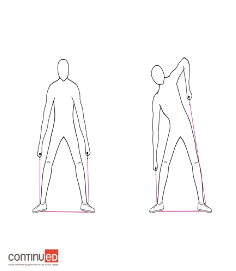
Figure 14. Example of side bends (Image ©2020 continued, LLC).
You stand on the resistance band with it in both hands and you are just bending side-to-side. It is really good for working out your trunk. These resistance bands will get your heart rate up a little bit, and it only takes just a few minutes. Remember the saying, "The other 23." Let's take 60 minutes to get moving for our own benefit.
Upper Body Stretches
Here are some stretches you can do:
- Shoulder Rolls
- Neck Side Stretch
- Neck Rotation
- Shoulder Circles
- Overhead Reach
- Reach Back
- Hand Stretch
- Arm Raises
Exercise releases endorphins to give you positive energy. If you cannot do a full-blown workout, a nice long stretch might be helpful. We all know that sitting for a lot of hours can be really harmful to you. Other ideas for stretching include making a loop around the house or your facility to stretch your arms and legs. This also helps you to stay limber to reduce injuries.
Lower Body Stretches
- Seated Lifts
- Back Stretch
- Inner Thigh Stretch
- Calf Stretch
- Hip Side Stretch
- Hip Rotation Stretch
- Ankle Circles
- Ankle Stretch
Lower body stretches are good as well. Do some chair push-ups or stretches to your inner and your outer thigh. Figure 15 is a great stretch. You can reach side-to-side, stretching out your trunk and legs.

Figure 15. Example of a whole-body stretch (Image ©2020 continued, LLC).
Keep Your Immune System Strong
Keep your immune system strong.
- Washing your hands
- Get enough sleep
- Eat well and stay hydrated
- Take vitamins and any prescriptions
- Prioritize personal hygiene and limit contact with others
- Cover your cough or sneeze
- Disinfect with anti-bacterial wipes
- Avoid touching your face, eyes, nose, and mouth
- Stay home when you are sick
- Exercise and stay active
- Get fresh air
We have talked about some of this already. We need to make sure we are getting our vitamins and any needed prescriptions. We know the importance of washing your hands thoroughly using either the happy birthday song, the alphabet, or whatever works for you. We will talk more about sleep here in just a second. Again, it is important to eat well and stay hydrated. Obviously, cover your sneeze or cough and then go wash your hands. Antibacterial wipes, when you can find them, are important to use to disinfect commonly touched areas. This is pretty obvious, but you should avoid contact with those who are sick and do not go out if you are sick. If you do go out, do not touch your eyes, your nose, or your mouth. Stay active if you are able. Walking, doing planks, and jumping jacks can be done in the home, even if you are watching television. For example, every time there is a commercial everybody can get up and do calisthenics. Your gym or fitness center may be closed, but there are many live streams or app-based workouts available. Take breaks and fresh air whenever possible maintaining the 6-feet social distance.
Sleep
- Upon waking, get at least 15–60 minutes of bright light
- Exercise close to wake-time
- Take naps and consider “banking” your sleep
- Use caffeine judiciously
- Limit alcohol before bed
- Keep a regular sleep and wake-time schedule as much as possible
- Create a regular bedtime routine of quiet activities
- Limit alerting activities close to bedtime
- Optimize your sleep environment
Sleep is really important especially now. In the face of any sort of global pandemic, the health and safety of all of us as healthcare workers is critically important. Research shows that most are not getting the recommended seven to nine hours of sleep per night. If we do not get enough sleep, it is going to impact immune function. A lack of sleep can lead to increased infections and accidents. Make sleep a priority. When you wake up, get at least 15 to 60 minutes of bright light. Natural sunlight, bright indoor light, or blue-enriched light signals to your body it is time to start the day. Exercise closer to your wake up time. Both of these can increase sleep quality. Avoid intense exercises closer to bedtime and particularly when you're sick. Take naps and consider maybe banking your sleep. What do we mean by that? Even short naps, less than 20 minutes, can improve alertness and memory.
Use caffeine judiciously. It can certainly help you when you are tired, but those effects remain for a couple of hours and can ultimately impact your ability to fall asleep later on in the evening. Try not to consume caffeine within about six hours of bedtime. And if we use caffeine too often, it becomes less effective when we really need it. Limit alcohol, particularly before bed. It might be sedating, but it disrupts your sleep.
Keep a regular sleep and wake-up time schedule as much as possible, particularly if you are working from home and even on your days off. That helps you keep your sleep and your circadian rhythms in sync, and it minimizes those feelings of psychological or physiological jet lag. Also, create a regular bedtime routine of quiet activities. Maybe it is a warm shower or reading a book. Maybe you brush and floss your teeth. Maybe it is relaxation exercises, deep breathing, or aromatherapy. Whatever it is that you need to get your mind and body ready for sleep. Limit those alerting activities especially light, a TV screen, phone, computer, exercise, work, caffeine, etc.
Finally, optimize your sleep environment. Keep it dark, cool, quiet, and comfortable. You can even wear an eye mask if that helps.
Connect With Others
- Stay connected using technology
- Talk “face to face” using Skype or FaceTime
- Disaster Distress Helpline at 1-800-985-5990
- Local Alcoholics Anonymous or Narcotics Anonymous offices
- Get creative to stay connected
- “Physical distancing” NOT “social distancing”
Connect with others. Reaching out to people you trust is one of the best ways to reduce anxiety, depression, and loneliness. Stay connected. Use your technology, whether it is FaceTime, Skype, Google Hangout, or Zoom. There is a distress helpline that comes from SAMHSA, the Mental Health Services Administration from the federal government. This might be helpful if you are feeling lonely or need support. Other supportive resources include Alcoholics Anonymous and Narcotics Anonymous. Their local offices are doing a lot to help people at this time. Get creative as we said. Come up with new ideas like a Google Hangout while exercising or doing a happy hour. The sky is the limit.
We need to describe it as physical distancing, not social distancing so that we never lose sight of the importance of social relationships during this time of high stress. Your social relationships are going to help you through this difficult time.
Social Wellness Checklist
- Make connections
- Look for creative ways to get involved with others
- Join an online group focused on a favorite hobby
- Take a class to try something new
- Online virtual tours of museums, theme parks, nature trails, etc.
- Look for creative ways to get involved with others
Make a social wellness checklist. Find an online group, engage in a favorite hobby, or try something new. There are so many neat virtual classes going on right now, and many are free. Others are only a small investment to learn new and different things like a new language or art technique. There are online virtual tours. There are a lot of things to keep us engaged. You just got to go find them.
- Take care of yourself
- Ask for help. Make a list of ways others can help
- Make to-do lists and set a daily routine
- Try to take breaks each day
- Keep up with your hobbies and interests
- Eat healthy foods, and exercise as often as you can
We have already hit on some of these, but we are not immune to emotional distress. We are equally as vulnerable as the patients and the individuals that we are serving. The stress and the strain of caregiving and working during this time period can take a serious toll on your health. Make sure that you are asking for help. Make a list of ways that people can help you. Make to-do lists and set up a daily routine. Try not to sit at your desk or work 24/7.
- Build health relationships
- Share your feelings honestly
- Listen to others without judgment or blame. Be caring and empathetic.
- Disagree with others respectfully
- Avoid being overly critical, angry outbursts, and violent behavior
- Compromise
Share your feelings with supervisors, family, staff, peers, colleagues, and friends. Listen to others without judgment or blame. Be caring and empathic, and disagree respectfully. Conflict should not turn into a personal attack. Compromise and avoid being overly critical. Everyone is going to be experiencing this differently, and we have to recognize that.
Hope
- Connect with someone in their family or community to ask another person they respect how they stayed hopeful in troubled times
- Download and view YouTube videos from church or inspirational speakers
- Take time to learn about other historical times of crisis, including how these ended and communities rebounded
- Share some of the many stories of hope and help that have come out of this current crisis
I think one of the big things is you have to have is hope. Hope is the expectation that ultimately everything is going to work out. Many people probably do not have that feeling right now. They feel discouraged, hopeless, or angry. We are all feeling a great loss for many things. It could be people, activities, or routine. Again, it is so important to connect with family, friends, and others in the community. Ask them, "How did you stay hopeful in troubled times?" You can download inspirational videos on YouTube or perhaps from a church. Take time to learn about historical times of crisis. How did those crises end? And, how did the communities rebound from them? You could also share some stories of hope with others. In my own community, we had a woman that was 78 or 79 that recovered. As she was coming home from the hospital, everybody came out on their porches and waved as she drove by. Look for those inspirational kinds of stories.
What Else?
- Meet basic needs
- Take breaks
- Connect with colleagues
- Communicate constructively
- Contact family
- Respect differences
We have talked about meeting basic needs. We will not go back over that. Taking breaks is a big thing. These do not have to be long breaks. It might include an activity unrelated to work that you find comforting, fun, and relaxing. Many of us feel guilty if we are not constantly working. However, you have to remember your own health and well-being. Connect with your colleagues, tell your stories, and listen to others, but again communicate constructively. I think this is important. Complement each other and build each other up. Compliments can be so powerful for motivation and for reducing stress. Share your frustrations, solutions, and problem-solving. That gives you another feeling of accomplishment. It is important to recognize and respect differences. Some people are going to want to talk, while others want to be left alone.
- Self check-ins
- Honor your service
- Set boundaries on work schedule
- Distract and redirect
- Be mindful
Self check-ins are important as I do not think that we always do this. Monitor yourself and look for depression, sadness, difficulty sleeping, and hopelessness, and make sure to address it. Do not let it fester or go on too long. Certainly, honor your service. Remind yourself that despite obstacles, frustrations, or whatever you are doing, as a caregiver, you are fulfilling a very noble calling. Also, recognize your colleagues, whether formally or informally. Honor the fact that you are doing amazing things for your peers, colleagues, patients, and your families.
We have already talked about setting boundaries. Again, make sure that you set those. Your health and wellness are paramount. Distract and redirect when you can. Again, engage in activities that you enjoy. Activities can include journaling, reading, art, cooking, or whatever. Find something and make it stick.
Lastly, be mindful. Again, during these times, it might be tempting to stay up late. "Oh, I don't have to get up in the morning." Or, you might find yourself mindlessly scrolling through TV. Establish good sleeping practices. Keep a worry journal. Try to maintain your regular schedule. As we navigate this new normal, consider really how you can use your time mindfully. It could be developing a new hobby, working on a home improvement project, or getting in the kitchen. Again, whatever you decide, focus on the things that you can do to contribute to your health and well-being versus lamenting what you cannot do. Instead of complaining and mourning losses, find that silver lining.
What Can Managers Do?
- Show empathy and be available
- Stay connected with communication and meeting tools
- Recognize the impact of isolation and loneliness
- Have a plan to monitor the course of the outbreak and take rapid and appropriate action if needed
- Create a culture of calm
What can managers do? Many organizations have employees out of the office. Right now it is more important than ever to get in regular communication to show empathy and touch base. How are you doing today? What went well yesterday? What are your frustrations? How might I be able to help? Working remotely, particularly, can cause people to feel very, very isolated. These routine check-ins are super important. Be aware of any changes that you are sensing. If you are not a manager, you can use these same principles to check in on colleagues.
Impact on Work
- Increased absenteeism from health problems or lost productivity
- Impaired judgment
- Unwillingness to accept extra work or responsibility
- Low motivation
- Low productivity; poor work quality (leading to poor client outcomes)
- Decreased compliance with organizational requirements
- Staff conflict
- High staff turnover (leading to ongoing training costs)
Is there a viable plan to monitor the course of the outbreak and to take action. While planning, we still need to create a culture of calm. I talk about modeling the behavior that you want to see. We want to have consistency, transparency, and support for each other. What we are going through right now is traumatic, and it has a big impact on work. There can be low motivation, high turnover, and absenteeism.
Signs of Traumatization
- Psychological distress
- Cognitive shifts
- Relational disturbances
- Frame of reference
There are also many signs of trauma like anxiety, nightmares, sleep disturbances, and complaints of headaches. You may be missing or canceling appointments and not engaging in self-care as you should. There can be suspicion and helplessness. You may find yourself judging, labeling, or feeling disconnected from your own identity. You can have a distortion of your values and lose your faith. This list can go on and on and on, but we are looking for these types of signs that someone is being traumatized. I strongly urge everybody, whether you are a supervisor or an employee, to do a self-check.
Use Psychometric Measures
- If you use the ProQOL in clinical supervision, present it as a self-assessment tool
- Work collaboratively and respectfully to explore their own understanding of and meanings attached to their scores
- Scores are one way for you and your supervisees to get a sense of whether they might be at risk for secondary traumatization, what they can do to prevent it, how to address it, and how you can support them
Use a psychometric measure to just check yourself where you are right now. The one that I am personally a fan of is the ProQOL, The Professional Quality of Life Measurement tool. It looks at where you are right now on the topics of compassion, fatigue, burnout, and the like related to your work and what it is that you are doing in your caregiving role.
Addressing Secondary Trauma
- Engage in regular screening/self-assessment
- Address signs of STS within clinical supervision
- Work collaboratively to develop a comprehensive self-care plan and evaluate its effectiveness on a regular basis
- Provide a safe and nonjudgmental environment
- Provide a place to debrief critical stress incidents at work
- Support and encourage individual counseling or psychotherapy, when needed
These tools can help you to understand not just where you are, but it also helps you to develop a comprehensive self-care plan. Just like we develop a care plan for our clients, we need to do the same for ourselves. This comes from an awareness of where you are right now and where you are struggling. You could share this information with your supervisor, but you certainly do not have to. I think that having the self-awareness to explore personal issues and be able to do that in a very safe, nonjudgmental environment is only going to help us.
Again, everybody responds differently. Some people are going to be very stoic and detached, and that is a great defense mechanism for them. Others are going to be very emotionally charged. We hope that our leaders (or we, as managers) are modeling the behavior that we want to see. We need to recognize the emotions that people are struggling with right now. Having empathy and compassion are so important during this time.
Trauma-Informed Leadership
- A way of understating or appreciating there is an emotional world of experiences in our colleagues
- Recognizes and honors the emotional scars that people may struggle with
- Helps leaders have empathy and compassion for their employees
All of this we call trauma-informed supervision. This is not only our leaders and managers but each of us, as peers, leading with empathy.
Why Trauma-Informed Supervision?
- Promotes staff retention and reduces turnover (Barak et al., 2001; Knudsen et al., 2013)
- Reduces levels of vicarious trauma experienced by staff (WCSAP, 2004)
- Influences supervisee ability to more effectively cope and have resilience (Sommer & Cox, 2005; Turner, 2009)
- Enhances worker well-being
- Facilitates best practices (Schwalbe et al., 2014)
It promotes staff retention, enhances worker well-being, and facilitates best practice. Overall, it is just a better way to be.
What is Trauma-Informed Supervision?
- Supporting staff
- Relationship-based supervision
- Best practices for reflective supervision
- Regularly scheduled meetings without interruption
- Discussions about change management
- Inviting colleagues to share experiences and explore experiences
What is trauma-informed supervision? It is supporting staff and offering relationship-based supervision. It is very different from clinical supervision. It is genuine sharing.
Leading With Empathy
- When employees experience empathy, understanding, and compassion from the leadership team they will feel safe, respected and recognized
I am a former manager and used to be a VP for a healthcare company. When we talk about clinical supervision, the last thing that we were ever taught was to get very relationship-oriented and get very involved. It de-emphasizes hierarchy and power differentials, and I think that is important. Our clients, if we are managers, are the people that we supervise. They can benefit from this supervision model as it incorporates all of the same elements that we are asking them to do with their patients. We want to see mentoring and coaching as a way to support professional development. Again, you do not have to be a manager to do this stuff.
It is important to have regularly scheduled meetings without interruption. I got into a conversation with somebody just the other day about this. Things are changing so rapidly in our organizations right now that it is hard to keep up and with reimbursement and what the government is doing. We need to talk with each other about these changes and the "why" behind the policies. We may not all like the changes, but if you can get the why behind it, it is a little more palatable sometimes. And again, inviting everybody to share experiences. It is very touchy-feely, isn't it? We, again, need to recognize that some people are going to thrive from that, and others will not, and that is okay. We need to be open to discussing that.
I am a firm believer that when employees experience true empathy, and true understanding and compassion, whether it is from leadership or their peers, they are going to feel safe, respected, and recognized. It is just a much better environment. When I say, "real," I mean real empathy and understanding and not something that feels fake or contrived.
Staff Responses
- Stress will transfer to our residents
- Give yourself some space to cope
- Share resources and education about abuse
- Be watchful and vigilant for risk factors for suicide
- Practice self-kindness
- Take care of yourself
- Gain insight into where you are struggling
In general, we have to consider that the stress that we have as caregivers might be transferred to those we serve. We are dealing with high amounts of stress and this is going to be ongoing for an extensive amount of time. This is not going to just resolve itself immediately. I was reading an article today about depression. With what we are going through right now, we are probably going to see an increase in clinical depression for some time to come. In light of this, consider the following. Share messages about how we need to give space when emotions run high and then model that behavior. When your emotions are high, step back and say, "You know what? I need to decompress for a minute. Let me go over here."
I think it is important to help others to schedule and develop routines. The more control they have, the better off we are. Also, share resources and education about abuse. This is outside the scope of what we are talking about today, but we are starting to see some of the data from other countries that the rates of domestic violence and child abuse have increased significantly during the COVID-19 crisis. Stress and increased isolation are risk factors for abuse. Be vigilant and be watchful for risk factors for suicide. These include hopelessness, isolation, and barriers to accessing help. Now is the time to be present and active in your family's and patients' lives, and in your own life. Be watchful for those things. In addition, practice self-kindness and gain insight into where you may be struggling. You cannot take care of others if you are not caring for yourself.
Considerations
- Support regulation
- Prioritize relationships
- Explain the why behind decisions
- Help staff know what to expect to the extent possible
- Reframe behaviors – we may not show up a sour best selves
When people are stressed, they have a harder time managing emotions and staying regulated. Try to build in time for regulation practice like breathing, exercises, movement, and model calm behavior. If we want everybody else to do it, we need to model it. Prioritize relationships, social support, and connection. You will figure out what works best for you, but this can buffer a stress response. We have to find those ways to connect with and support each other. In uncertain times, having any amount of certainty or predictability is helpful. I am not suggesting that you provide answers if you do not have any, but share information when it is available will help to decrease stress. And, as you are sharing that information, keep in mind cultural competency, health literacy, and the like. Keep it on a level that people can understand, recognizing that not everybody has the same understanding of what is going on right now. Finally, we need to reframe behaviors. Remember that emotional regulation and impulse control are going to be a lot more difficult during times of stress. Everyone may not be showing up as their best self during this period. You need to give everyone some grace and understanding and realize that the challenging behaviors really are a reflection of the stress that we're all under, not that this person has changed. So to the extent possible, exercise patience and understanding and give everyone the benefit of the doubt. I say to my family all the time, "I pray for patience, but I don't tend to get it. I just get more and more opportunities to exercise it." I think that is where we are right now. We are getting more and more opportunities with each other, with our families, and with our coworkers to exercise that patience.
- Remember that we as caregivers are the best predictors of how our residents are doing; they are watching and listening to us. When we take care of ourselves, we’re showing them how they can take care of themselves, too.
We can find that meaningful, purposeful behavior that we as OTs are famous for. When we exercise, eat well, and focus on our own mental health, we are showing them that we are taking care of ourselves while we are taking care of them. By doing so, we are modeling good behavior that is so imperative right now.
References
Abd-Alrazaq, A., Alhuwail, D., Househ, M., Hamdi, M., & Shah, Z. (2020). Top concerns of tweeters during the COVID-19 pandemic: A surveillance study. Journal of Medical Internet Research. DOI: 10.2196/19016.
Bloom, S. (2012). The Workplace and trauma-informed systems of care. Presentation at the National Network to Eliminate Disparities in Behavioral Health.
Bloom, S. L., & Farragher, B. (2011). Destroying sanctuary: the crisis in human services delivery systems. New York: Oxford University Press.
Calvo, R., Deterding, S., & Ryan, R. (2020). Health surveillance during covid-19 pandemic. BMJ, 369, m1373.
Dozier, M., Cue, K.L., & Barnett, L. (1994). Clinicians as caregivers: Role of attachment organization in treatment. Journal of Consulting and Clinical Psychology, 62(4), 793-800.
Fallot, R. & Harris, M. (2006). Trauma-Informed Services: A Self-Assessment and Planning Protocol. Community Connections.
Herman, J. (1992). Trauma and recovery: The aftermath of violence – from domestic abuse to political terror. New York: Basic Books.
Hummer, V. & Dollard, N. (2010). Creating Trauma-Informed Care Environments: An Organizational Self- Assessment. (part of Creating Trauma-Informed Care Environments curriculum) Tampa FL: University of South Florida. The Department of Child and Family Studies within the College of Behavioral and Community Sciences.
Shaw S. (2020). Hopelessness, helplessness and resilience: The importance of safeguarding our trainees' mental wellbeing during the COVID-19 pandemic. Nurse education in practice, 44, 102780. Advance online publication. https://doi.org/10.1016/j.nepr.2020.102780
Sultana, A., Sharma, R., Hossain, M., Bhattacharya, S., & Purohit, N. (2020). Burnout among healthcare providers during COVID-19 pandemic: Challenges and evidence-based interventions. SocArXiv. https://doi.org/10.31235/osf.io/4hxga
Unadkat, S., & Farquhar, M. (2020). Doctors’ wellbeing: self-care during the covid-19 pandemic. BMJ, 368, m1150.
Vieira, C., Franco, O., Restrepo, C., & Abel, T. (2020). COVID-19: The forgotten priorities of the pandemic. Maturitas, 136, 38-41.
Citation
Weissberg, K. (2021). Sustaining the well-being of healthcare workers during coronavirus.
