Introduction
On the first slide, I wanted to put up this graphic of words related to ACEs or Adverse Childhood Experiences to frame our discussion (Figure 1).
Figure 1. Words related to ACEs.
You may be thinking, how does the topic of ACEs relate to respiratory therapy? I want to give you some background. I started practicing in 1993. One of the very first slang terms I was exposed to was the "frequent flyer." I am sure in your own practice you can think of frequent flyers. These are people that come back into the health system over and over. Sometimes, they only go home for a few days before they are back. For years, I thought that frequent flyers resulted from poor education and issues with finance and access. I blamed that system for dumping them out as the reason they kept coming back.
Over the years, the issues associated with readmissions for COPD have really come to the forefront. Managers, CEOs, CFOs, therapists, and many others have been looking at ways to ensure these patients do not return within 30 days of discharge from a facility.
Around this same time, I decided to complete a master's degree in education. I focused on the instruction curriculum and went back to work in the university setting. I was teaching classes and was away from bedside treatment, but I was still connected through my clinical chair position. I decided to pursue my doctorate to expand my knowledge base. I have also been fortunate throughout my professional career working in various roles like in rehab; I was a director over PT, OT, and speech; and I worked in quality management, social services, and utilization review. I even worked on a pharmacy committee. I have a pretty broad knowledge of what is happening in healthcare, but when I was looking for an advanced degree path, I wanted to expand upon that even further.
I picked a Doctorate of Health Sciences from Nova Southeastern in Fort Lauderdale. The relevance of this story is that I picked the Global Health Track. As part of the Global Health Track, I did not do a dissertation, but instead, I completed a practicum and an internship. For many years, I wanted to work with foster children, especially kids abandoned within the system that did not have representation. Personally, I had adopted a son when he was 16. He had come from a very broken family with both parents and having addiction issues. One of his parents was in prison, and one was gone, so he was raised by grandparents.
I was excited for the opportunity to learn more about these kids left in the shadows (the actual name of my practicum and internship). As part of that, I became a court-appointed special advocate. If you are not familiar with this role, you represent children in the foster care system. As part of that process, you have to continue your education. As I was sitting in this continuing education class, they showed a documentary called "Resilience: The Biology of Stress and the Science of Hope." At that hectic moment in my life (balancing school/work/life), I had a light bulb moment. As a respiratory therapist training to be a court-appointed special advocate and watching this movie, I realized that ACEs might be the key to COPD management.
Adverse Childhood Experiences (ACEs)
What Are ACEs?1
- Adverse childhood experiences, or ACEs, are potentially traumatic events that occur in childhood (0-17 years)
- For example:
- Experiencing violence, abuse, or neglect
- Witnessing violence in the home or community
- Having a family member attempt or die by suicide
ACEs are what the CDC calls Adverse Childhood Experiences. They are traumatic events that happen to a child somewhere between zero and 17 years of age. This can be violence, abuse, or neglect. This can be witnessing abuse or receiving abuse at the hands of a parent or a loved one. It could be seeing the death of a loved one or seeing violence in the community. This could be murder, drive-by shootings, burglary, et cetera. We see these events often in our lower socioeconomic neighborhoods. It can also be a family member's attempt or death by suicide.
- Also included are aspects of the child’s environment that can undermine their sense of safety, stability, and bonding, such as growing up in a household with:
- Substance misuse
- Mental health problems
- Instability due to parental separation or household members being in jail or prison
When you think of trauma and adverse childhood experiences, you think of the big things right away. However, there is more to it. Adverse childhood experiences can be any situation where a child feels unsafe, has not had the ability to bond with caregivers, or have no stability. Foster kids are one example. What is happening in those homes? There can be substance misuse, mental health problems, a parent leaving secondary to divorce, parental separation, or even a household member being in jail or prison. How does all of this impact future wellbeing?
Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study 5
- The CDC-Kaiser ACE Study is one of the largest investigations of childhood abuse and neglect and household challenges, and later-life health and well-being.
- Conducted between 1995 and 1997, over 17,000 HMO members from Southern California receiving physical exams completed surveys regarding their childhood experiences and current health status and behaviors.
- A strong graded relationship between the breadth of exposure to abuse or household dysfunction during childhood and multiple risk factors for several leading causes of death in adults.
In 1998, researchers (two of them Anda and Felitti) partnered with the CDC and Kaiser Permanente in Southern California to assess ACEs. They assessed 17,000 HMO members. The extensive questionnaire (assessment tool) was 21 pages long that asked about home life experiences and challenges during childhood. The idea was to correlate what happens in childhood with adult health issues or current health status and behaviors. They had a 70% return rate (exceptional for a study). They recognized that abuse and household dysfunction during childhood led to several leading causes of death in adults. It showed that these adverse events directly impact a child and affect overall health and wellness as an adult. We knew this intuitively, but we did not know the full picture until this study came out. I feel these are fairly obvious things, but when you put pen to paper and start researching those pieces of the puzzle, it makes sense. What does this mean?
ACEs: An Introduction (Video)
This is a five-minute video that gives an introduction to the topic. It is from that documentary that I was talking about Resilience. It talks about where the study came from, why it was important, and its impact on overall health and wellness. One of the best parts of it is at the very end. It talks about what is predictable and preventable. This is the direction we are going to be going with this talk today. We want to know how ACEs relate to our COPD.
Graphic: Adverse Childhood Experiences8
Here is a graphic about ACEs to take a look at this a little bit closer (Reference to image link provided below).
As we discussed, ACEs are traumatic events, small to large, that impact our overall wellbeing. When you look at this graphic, there is a lot of information on it. I want to point out a couple of things that they also touched on in the video. One of the most important pieces is that people with 6+ ACEs lose 20 years of their lifespan. He talked about that in the video, and we will talk more about this in a minute. How many do I have? How many do you have? How does that impact our longevity and how healthy we are in the long run?
One-eighth of the population has had more than four ACEs between the years of 1 and 17. And, if you have had more than four ACEs, you are three times more likely than the normal average American citizen to smoke and develop lung disease. You are also 14 times more likely to have had a suicide attempt and four and a half more times likely to develop depression. You are 11 times more likely to have had used intravenous drugs and four times as likely to have started having sex before 15. Lastly, this group of people is twice as likely to develop liver disease.
What happened to us a child directly impacts us later in life, including health issues. If we want to create a healthy population and improve the United States' overall wellbeing, we have to consider what is happening during those developmental years. They also mention in the video, and you may or may not have caught it, about actual biological changes. Toxic stress can make changes to the neural pathways and the genetic makeup of your body. This, in turn, is passed down from generation to generation. The impact of this study is absolutely huge.
ACEs Prevalence- BRFSS Study
Let's break it down just a little bit more. Figure 2 shows some more current data. This data was collected between 2011 and 2014, and it is from the Behavioral Risk Functional Surveillance System.
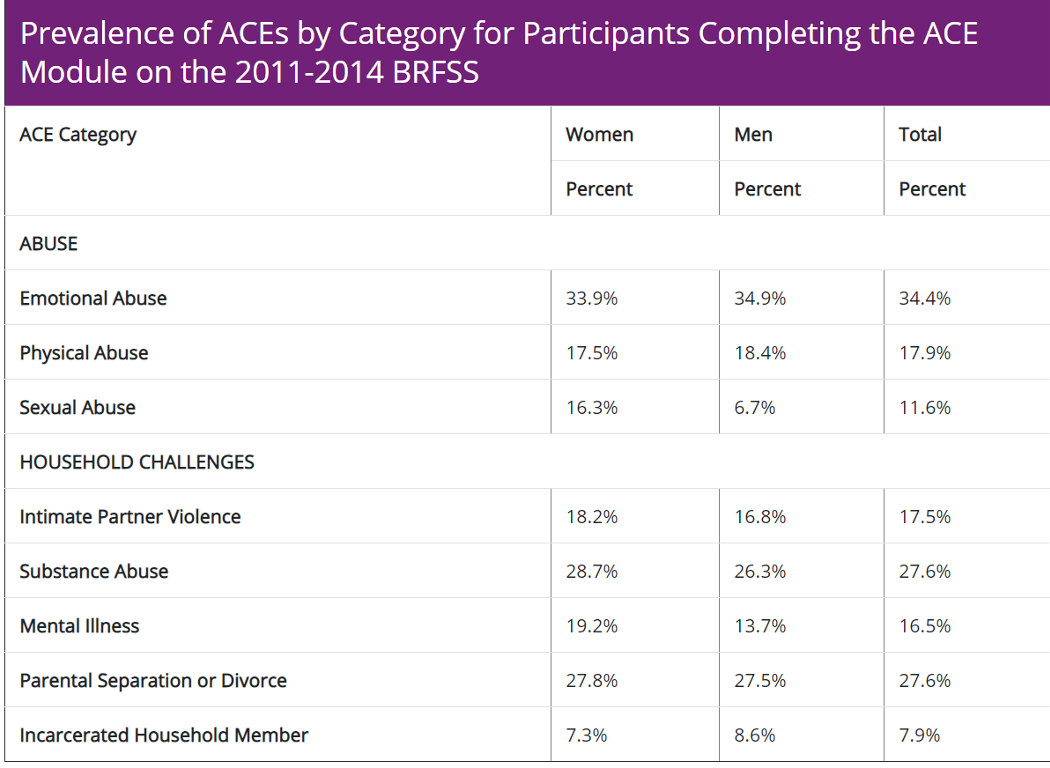
Figure 2. Prevalence of ACEs according to the BRFSS study.
After the study came out from Kaiser Permanente, the CDC recognized the substantial value in collecting data about what was happening to American citizens during childhood. They developed a phone call system where they called random phone numbers and collected data. This spanned 48 States and included the District of Columbia. It went on for several years. All of those states participated for at least one year, and so what came out of that data is a breakdown of what the adult population experienced during childhood.
The graph is broken down by women and men. Abuse includes emotional, physical abuse, and sexual. When you look at the population percentages, 34% had emotional abuse. 17-18% had physical abuse, and 12% had sexual abuse. You will notice that sexual abuse is higher in women than in men, so there is quite a bit of disparity to consider there.
As we look at household challenges, 17.5% of the population had intimate partner violence (IPV) exposure. Almost 28% of the population saw some sort of substance abuse. Mental factors occurred in 16.5% of the population. Remember, this data is from 2011 through 2014. Now, we are in 2021, and so much has happened in the last year. I would estimate that these numbers are probably much higher at this point.
Parental separation or divorce is high at 28% of the population. We even see 8% of the population had an incarcerated household member. If you think about the last slide that talked about the propensity for long-term health issues, you can see how all of these things (depression, suicide attempts, IV drug use, early sexual encounters, et cetera) are tied to these numbers. There is a high percentage of the population has had some sort of childhood experience that was negative. At this point, you may be thinking, "How many ACEs do I have?"
How Many ACEs Do You Have? 1
- ACEs are common, with 61% of adults surveyed across 25 states reporting that they had experienced at least one type of ACE
- Nearly 1 in 6 reported they had experienced four or more type of ACEs
- Take the Survey (Study Questionnaires):
I have given you a lot to think about, I am sure. For me, my parents are divorced, so I have a score of one. At least 67% of adults surveyed across 25 States have at least one type of ACE. If you add in any sort of violence, a family member going to jail, drug abuse, mental health issues, and the like, the number grows. One in six American adults has reported more than four. If you are curious, there is a survey that you can take that is hyperlinked above. You can also take the CDC study, the one that was pulled from Kaiser Permanente, as it is found on the CDC website. Let's compare this data to the rest of the United States. In 2010, through similar information gathering, they looked at the total number of ACEs in the US (Figure 3).
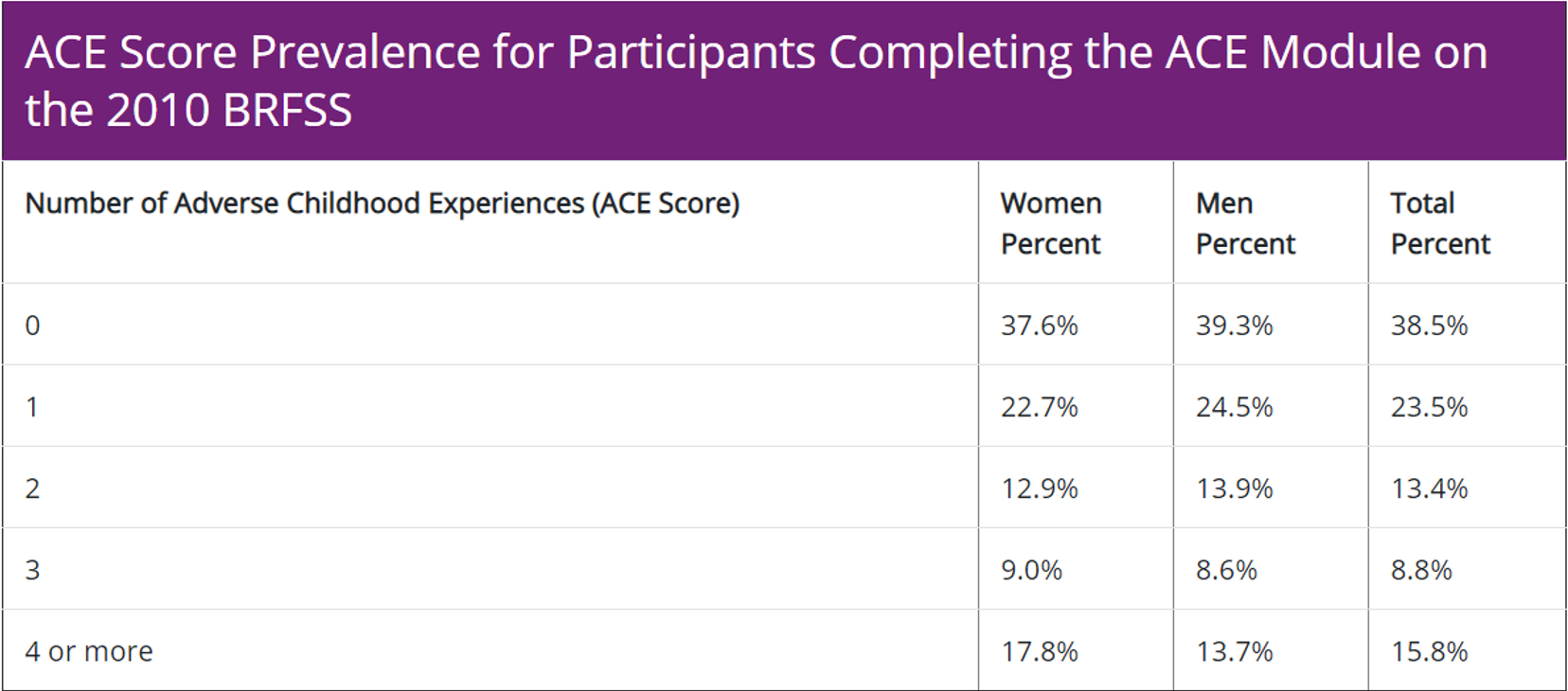
Figure 3. ACE Score Prevalence in the 2010 BRFSS.
Zero to 38.5% do not have any ACEs, but 23.5% have at least one, and 13.4% have two. Three adverse events in the population sit at only 8.8% or 9% of the population but then when you get to four or more; this is 16% of the population. Again, with 4 or more, there are some dire consequences of that.Figure 3. ACE score prevalence for participants based on the number.
Who are we talking about? Looking at Figure 5 ACES based on race and income, the demographic most prone to having ACEs are multiracial households.

(Image source: Baylor University)
When you look at emotional abuse, substance abuse, physical abuse, and mental illness, multi-racial households dominate those categories. Hispanic populations follow that, and then it is a toss-up between White and Black communities. I did notice that there was a higher propensity for separation and divorce in Black households as compared to biracial, Hispanic, and all White households.
Who is Affected by ACEs?7
- Unfortunately, no one is immune to ACEs
- The highest incidence noted in participants who identified as black, Hispanic, or multiracial
- Individuals with less than a high school education and from households with incomes of less than $15,000 annually
When we, as healthcare providers, start thinking about who our patients are and what they have experienced in life and putting this face on our clients with COPD, it helps us identify with some of their struggles and issues that they have had to overcome in life to get to this point.
No one is immune to ACEs, but it is clear that multiracial, Hispanic, and Black communities are the most prone. Individuals with less than a high school education and from households with incomes of less than $15,000 annually are also predisposed to an increased number of ACEs. Think about the stress of caring for a family with earning just over $1,000 every month. I cannot imagine how that impacts what is going on in that household and community.
Consequences1
- Lasting, negative effects on health, well-being, and opportunity
- Experiences are associated with increased risks of:
- Injury
- STD
- Maternal and Child Health Problems
- Teen Pregnancy
- Involvement in Sex Trafficking
- Chronic Disease
What are the consequences? We have established that a good percentage of the population has had ACEs, and there are negative effects on health, wellbeing, and opportunity. There are some listed, but let's look at this next one because this next slide really does a better job of really identifying and kind of giving us some details.
Lasting Impacts
What are the lasting impacts of Adverse Childhood Experiences?
- Injury
- Traumatic brain injury
- Fractures
- Burns
- Mental Health
- Depression
- Anxiety
- Suicide
- PTSD
- Maternal Health
- Unintended pregnancy
- Pregnancy complications
- Fetal death
- Infectious Diseases
- HIV
- STDs
- Chronic Diseases
- Cancer
- Diabetes
- Risky Behaviors
- Alcohol and drug abuse
- Unsafe sex
- Opportunities
- Education
- Occupation
- Income
The first one we will talk about is Injury. You may automatically think that this is secondary to abuse. However, it may or may not be abuse. It may be just a lack of supervision. We are talking about everything from traumatic brain injuries from abuse, fractures, burns to even possible injuries from having no real supervision. We also see mental health issues. We have already talked about depression. There are 21 million cases of depression associated with Adverse Childhood Experiences. As a result of that, we see increased anxiety, suicide, and PTSD. The next one is maternal health. A lot of early sexual activity is associated with what is happening in the home. There can be unintended pregnancy and possible complications due to the mother's age and no good prenatal care. There can be infectious disease issues such as STDs and HIV. For chronic disease, we may see cancer and diabetes. Risky behaviors include addiction, which I am going to go over in more detail in a second. Risky behaviors also include alcohol and drug abuse and unsafe sex secondary to childhood experiences.
The last one is opportunities. Sometimes I feel like it is overlooked, although it is a big piece of the puzzle. These are education, occupation, and income. I teach a global health class, and we actually have an entire section on poverty and the poverty cycle. There is always much discussion with our college freshmen about whether or not poverty perpetuates itself. The reality is that poverty begets more poverty. Oftentimes, these individuals living in households without proper support, great parental roles, or adequate income do not have the same opportunities in education, jobs, and income.
ACEs and Addiction3
- According to the Council on Recovery, approximately 64% of people have at least one ACE, which can double to quadruple the likelihood of using drugs and alcohol, particularly at an early age
- Having an ACE score of 4 increases your likelihood of becoming an alcoholic by 700%
- People with a score of 5 or higher are 7 to 10 times more likely to use illegal drugs and become addicted
I mentioned addiction a few minutes ago. The prevalence differs depending on the source. According to the Council on Recovery, 64% of those with 1 ACE have an addiction issue, but I have also heard 67%. How do ACEs relate to chronic obstructive pulmonary disease? We know that COPD is often caused by tobacco, and the use of cigarettes is an addictive drug. Thus, you can see how this could translate to what is happening with our COPDers and why they have such difficulty with kicking the habit.
This next one really always traumatizes me. That magic number of four ACEs is a big unhappiness indicator. If you have an ACE score of four or greater, this increases your likelihood of becoming an alcoholic by 700%. I have a very good friend that deals with alcoholism with an ACE score of greater than four. He was predisposed long before he had control of his situation. It is heartbreaking, but it is the recognition of that issue that leads to intervention. People who score five or higher are 7 to 10 more likely to use illegal drugs or become addicted. Addiction obviously is a real issue, and that is why I am highlighting it.
Correlation Between ACEs and COPD
Is there a correlation between ACEs and COPD? I pulled this from acesaware.org, notice that COPD is listed second in health conditions (Figure 4).
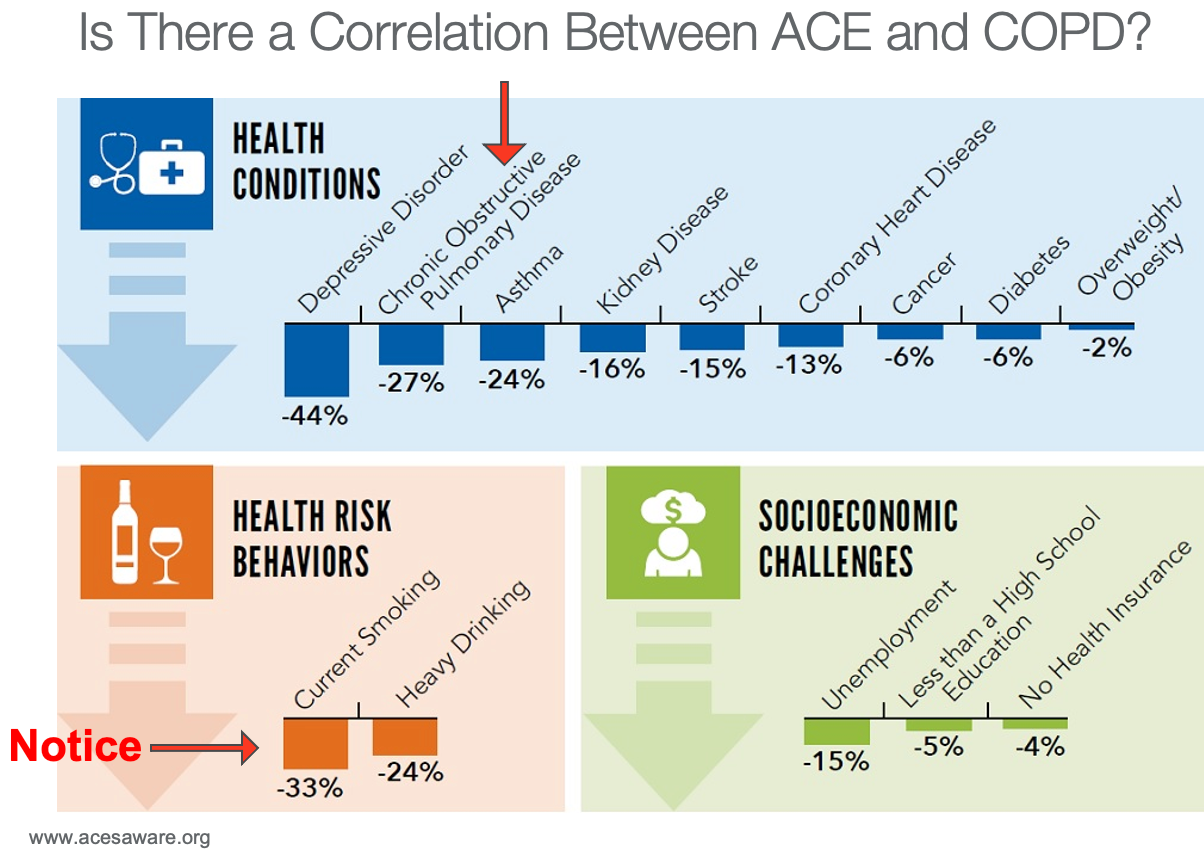
Figure 4. Correlation between ACEs and COPD.
The only thing beating COPD as negatively associated with ACEs is depression. Notice at the bottom in health risk behaviors, current smoking, and heavy drinking are the top two, where 33% of the population is experiencing heavier levels of smoking than the average American citizen. Does that mean that ACEs cause COPD?
Adverse Childhood Experiences and Chronic Obstructive Pulmonary Disease in Adults2
- In study results published in 2008 in the American Journal of Preventive Medicine, researchers examined the data from 15,472 adult members enrolled in the Adverse Childhood Experiences (ACE) Study from 1995 to 1997
- The number of ACEs was used to examine the relationship between childhood stressors to the risk of COPD
- Conclusion:
- Adverse childhood experiences increase the risk of COPD
- Because this risk is only partially mediated by cigarette smoking, other mechanisms by which ACEs may contribute to the occurrence of COPD merit consideration
The first study that I pulled is from 2008. They pulled data from the original ACE study that was done from 1995 to 1997. From that, they pooled specific data out as it related to COPD. They found that ACEs increased the risk of COPD. The most important line on this slide is the very last line. "Because this risk is only partially mediated by cigarette smoking, other mechanisms by which ACEs may contribute to the occurrence of COPD merit consideration." This means that, yes, cigarette smoking causes COPD. However, this study identifies that it is not just cigarette smoking causing COPD in this population. There are other contributing factors. Remember, some COPDers have never smoked a cigarette in their life. Why don't we see alpha-1 antitrypsin disorder? We see other secondhand exposures and all the other things happening. However, we see a direct association between COPD and ACEs without a specific correlation to cigarette smoking.
Sex-specific Relationships Between Adverse Childhood Experiences and Chronic Obstructive Pulmonary Disease in Five States4
- In study results published in the International Journal of Chronic Obstructive Pulmonary Diseases, researchers examined the data of 26,546 women and 19,015 men in MN, MT, VT, WA, and WI
- Occurrences of childhood abuse, household dysfunction, COPD diagnoses were recorded in addition to age, gender, race, marital status, education, and smoking status
- Weighing the prevalence of ACEs and COPD diagnoses among their patients, the authors found women who experienced an ACE were significantly more likely (P<0.05) to have COPD than women who did not
- While the male sample had a higher rate of COPD development (P<0.05), the link between COPD and ACEs was not as strong
The next study was done in 2014. It looked at 26,546 women and 19,015 men, but they looked in five specific states: Minnesota, Montana, Vermont, Washington, and Wisconsin. They looked at the correlation between childhood abuse, household dysfunction, and actual COPD diagnoses. They also looked at marital status, age, and those types of things. By weighing the prevalence of ACEs and COPD diagnoses among their patients, the authors found that women who experienced an ACE, just one, were significantly more likely to have COPD than women who did not. The male correlation was not as strong, but this was a study done in 2014 and looked at a particular population. Overall, they saw a correlation between ACEs and COPD.
Adverse Childhood Experiences and Chronic Lung Diseases in Adulthood: A Systematic Review and Meta-analysis6
- A total of 19 studies were reviewed as part of this meta-analysis
- The relationship between ACEs and the development of lung disease in adulthood was evaluated
- The meta-analysis showed that those who have adverse childhood experiences have approximately a 40% chance of presenting with lung disease
- It is worthy to note, however; when other risk factors such as smoking were taken into consideration, the risk is greatly decreased
This was a meta-analysis that looked at 19 studies. I like this because it was done in 2020. The men's analysis showed that those who have adverse childhood experiences have approximately a 40% chance of presenting with lung disease. They looked at 19 different studies examining lung disease and ACEs and found a 40% greater chance in that population. However, it is worthy to note that when other risk factors such as smoking were considered, the risk was greatly decreased. They weighed more heavily on the smoking piece, but we have to think about ACEs' addiction component again. If we know the individuals who experience high numbers of ACEs are more prone to addiction and are more willing to take risk-taking behavior or start risk-taking behaviors early, the odds of them starting to smoke young will be much greater than those of the normal average citizen.
Addressing ACEs in Our COPD Patients
- So if we know ACEs contribute to addiction and furthermore the development of COPD?
- What do we do with that info?
I am thinking back to when I first started talking about the frequent flyer. We know that ACEs contribute to addiction and the development of COPD. Now, what do we do? The reality is that a COPD diagnosis very well may warrant a psychosocial intervention.
Psychosocial Interventions for Patients with Severe COPD-An Up-to-Date Literature Review9
- Rzadiewicz and Nasilowski (2019) completed a literature review of those studies over the past 10 years that assessed interventions focused on psychosocial support for patients with advanced COPD, including those with chronic respiratory failure
- Strategies noted include:
- Palliative Care
- Telehealth and/or Telemedicine
- Self-management
- Pulmonary Rehab
- Mind-Body Interventions
I pulled up a literature review from 2019 that looked at studies over the past 10 years and what actual interventions worked with our advanced COPD patients. Strategies that were found to be the most beneficial were palliative care, telehealth, self-management, pulmonary rehab, and mind-body interventions. As respiratory therapists, we spend an enormous amount of time and energy in acute care. We put so much of our resources into acutely ill clients, like the clients with COPD exacerbation. We need to start looking at these puzzle pieces that often get overlooked in the healthcare system. For telehealth, we make sure they understand after they get home what, when, and how much medicine they should be taking. We also ask if they are monitoring their blood sugars, oxygen levels, and blood pressures. We ask if they have swelling and what is their input and output. We want to assess all of these self-management tools during pulmonary rehab. I am disheartened when I see decreases in funding for pulmonary rehab and difficulties with reimbursement. The reality is that pulmonary rehab and mind-body interventions probably have the greatest potential to truly impact the COPD population. I am a huge believer in pulmonary rehab. I spent some time working in long-term acute care and working with vent-dependent patients. Again, physical wellbeing, core body strength, muscle strength, and ways to alleviate stress through meditation, positive energy, and mindset were big pieces of the rehab process. Knowing more about who they are and where they came from allows us to address those underlying stressors that we may or may not have seen before to make a bigger impact.
Addressing Adults with Adverse Childhood Experiences Requires a Team Approach10
- Valeras et al. (2019) conducted a small qualitative study in a primary care office utilizing interviews to determine the effect of adverse childhood experiences and their relationship with their healthcare team
- Patients interviewed expressed maladaptive stress responses and a fear of abandonment during heightened stress states
- The direct correlation between ACEs and maladaptive stress responses suggests that incorporating a trauma-informed approach is essential in treating this patient population
- The study further suggests the integration of mental health professionals into primary care settings to better serve patients with trauma histories
I thought this was an excellent study beyond the psychosocial piece. This looked at bringing in mental health professionals. We know that the vast majority of patients dealing with long-term illnesses, like COPD and cardiac issues, diabetes, and high blood pressure, are attributed to ACEs. Thus, it makes sense that we have a mental health intervention immediately. This study found a direct correlation between ACEs and maladaptive stress responses. This means that patients are scared to death that when they find out, they have a diagnosis that also may be related to previous things that happened in their lifetime. Having that mental health person in that initial care setting could go a long way to help with compliance, education, and maintenance of long-term health issues.
Early Intervention/Resilience
Resilience is a great word. It was the title of the documentary I was watching. Resilience is the ability of a substance or object to spring back into shape; elasticity. Or it is the capacity to recover quickly from difficulties or toughness. In the video, if you remember, he said, "If it's predictable, it's preventable." We spend a lot of time and energy on the backside as respiratory therapists dealing with COPD patients. Often, they are at the end of life and dealing with the long-term consequences associated with ACEs. We just talked about some good psychosocial interventions and the importance of incorporating the mental health pieces early on. However, I still feel it is valuable for me to bring up early intervention as I know some pediatric therapists who will be watching this. I think it is super critical to use education to change the world. The better equipped we are to handle what is out there, the better positioned we are in improving upon what is out there.
- “What’s Predictable is Preventable”1
If we know all of these negative things happen due to ACEs, and now we are coming up with ways to improve it after the fact, we now need to look at what we can do in the beginning. This reinforces the need for early support to the family. Figure 8 shows a couple of pieces in this puzzle.
- Strengthen economic supports to families
- Strengthing household financial security
- Family-friendly work policies
- Change social norms to support parents and positive parenting
- Public engagement and enhancement campaigns
- Legislative approaches to reduce corporal punishment
- Provide quality care and education early in life
- Preschool enrichment with family engagement
- Improved quality of child care through licensing and accreditation
- Enhance parenting skills to promote healthy child development
- Early childhood home visitation
- Parenting skill and family relationship approaches
- Intervene to lessen harms and prevent future risk
- Enhance primary care
- Behavioral parent training programs
- Treatment to lessen harms of abuse and neglect exposure
- Treatment to prevent problem behavior and later involvement in violence
First, we can strengthen economic supports in the families. This is strengthening household financial security and having family-friendly work policies. Again, $15,000 yearly brings that minimum wage debate to light. What can we do to strengthen the financial resources that these families have available to them when caring for these children? At $15,000/per household, most likely, you are looking at a situation where both parents are working, and potentially they are working multiple shifts or jobs. There are several different health care facilities around our area and throughout the nation that offer childcare and even instruction and so forth. If we can do these types of programs in needy communities, this could have a huge impact.
We also need to change social norms to support parents and create positive parenting. I was fairly sheltered as a child. When I came into healthcare and met a variety of people, I was shocked. People assume that parents know how to parent. I am not sure why we think that because obviously there is no manual. Individuals are engaging in early sexual activity with early teen pregnancies are perpetuating this cycle. It is critical to support at-risk populations and give them the resources, education, knowledge, et cetera.
Quality care and education need to occur early in life. I touched on this concept with the whole family-friendly work policies. Head start programs are crucial, and we should be spending money in this area. I live in Texas, north of Dallas, and there was a big push to cut funding to our child advocates program. I spoke to several of our city council and board members on behalf of child advocates. I could not see anything that was more backward than this. Why on earth would we cut resources? The best part was that they were looking to cut resources in childhood development because we had a budget shortfall, and they needed money for building a jail. This is the polar opposite thing of what we needed to do. We needed to be reinvesting in those kids to prevent the need for future jails.
Again, we need to enhance parenting skills to promote healthy child development. This includes early child home visitations. This is one of the things I do with Casa (child advocacy). I do not tell them what to do, but I try to help lessen harm and prevent future risk.
Speaking of lessening harm and preventing future risk, enhanced primary care and behavioral parent training programs are intervention areas. We need to make sure they have adequate access to medical treatments. We need to provide treatment to lessen the harms of abuse and exposure, and then treatment to prevent problem behavior and later involvement in violence. All of this takes education and investment. If we can make a change early on, we have a chance to offset some of these experiences to improve their overall well-being later in life. For example, we could prevent COPD by educating and empowering our kids within our high-risk populations.
Additional Resources
- ACEs Aware https://www.acesaware.org/heal/resources/
- Belsky M. (2019). The Deepest Well: Healing the Long-Term Effects of Childhood Adversity: by Nadine Burke Harris, MD. The Permanente Journal, 23, 18-075. https://doi.org/10.7812/TPP/18-075
- National Council on Family Relations https://www.ncfr.org/index.php/cfle-network/summer-2017-ACEs/aces-resources-family-life-educators
- Resilience: The Biology of Stress & The Science of Hope. https://kpjrfilms.co/resilience
I have listed a few additional resources. ACEs Aware is a great website with lots of good information. "The Deepest Well: Healing the Long-term Effects of Childhood Adversity" is by Dr. Nadine Burke Harris. You can also go to YouTube or the CDC for information. Most of the information out there is going to be from Dr. Burke Harris. She has done numerous Ted talks. She wrote this book, "The Deepest Well." It is absolutely fantastic. There is also good information on the National Council of Family Relations website. Lastly, I have mentioned this documentary several times called "Resilience: The Biology of Stress and The Science of Hope."
Summary
In summary, I think the relationship between ACEs and COPD is fairly evident. There are opportunities for us to change things and to intervene. For years as a therapist, I have thought that every patient with COPD should have a psych eval, and now the reality is that this is probably the truth. Data going all the way back to 20 years ago suggests a high prevalence of ACEs in individuals filling out the questionnaires. Now in 2021, we are looking at a 22-year status post the publication of this seminal study. In that time period, what do we see within society? Have we seen improvements? Have we seen dramatic change? Have we seen decreases in poverty, violence, and drug abuse? Absolutely not. The reality is the information that was pulled from the study over 20 years ago is probably more relevant in today's world. It is beneficial for us, as respiratory therapists, to really look into what we can do to intervene and better address those things that have happened early in life associated with our patient population. There is a lot of potential for improvement and for us to change what we are doing for the children of tomorrow.
Questions and Answers
Is it possible that doctors may be overlooking children with ACEs?
Absolutely. Let's use an example of pediatric practice. If we have a child that is coming in, potentially with a grandparent and not the primary care provider, it is completely possible that in the five to 10 minutes of the assessment (although we hope for a 15 to 20-minute assessment) that they are not getting the full picture of what is happening with the child. They must be incorporating some assessment tools when talking to the parent/caregiver to get a better picture, as I do believe that a lot of children are slipping through the cracks. For years, we have downplayed the impact of divorce, the impact of a parent not being in the home, and the impact of a lower socioeconomic status. Often, we do not want to call a parent or a caregiver out for that situation or create a guilt situation. Caregivers may not even share these types of things for fear of being ostracized for not providing the perfect ideal environment. All of these pieces of the puzzle lead to the potential for a child to be missed. Additionally, how often does a pediatrician, a primary care provider, see the child? In the early years, children are seen more often when we are doing immunizations and well-baby checks. There is no guarantee that a child is coming to a pediatric provider for immunization in today's world. We may have more opportunities with CVS, the health department, and so forth. I firmly believe that we are missing opportunities to make a difference to offset a wide variety of health issues.
What can I do as that respiratory therapist to recognize or provide the care needed, especially if, let's say, there are more than three to four ACEs?
Many times as respiratory therapists, we get caught up in our to-do list. I commend any therapist who truly assesses what is happening with their patient and is really engaging and involved. It is easy for us to overlook the signs and symptoms of potential mental illness or associated stressors with ACEs. Our adult COPD population is typically going to tell us that they are fine. They are going to try to camouflage those issues. For the RT to identify that and to see that this person is potentially in need is going to be absolutely huge. However, this will be more than walking into a room, giving a breathing treatment, and doing a quick assessment. It is going to be engaging and talking to that patient. The more time we spend talking and engaging with the patient and family members, this will give us an idea of what is going on. We may be able to identify those at high risk (4+ ACEs) as they start talking about divorce or family members that struggle with addiction. They may also be caring for a loved one that has addiction issues. We may even see signs and symptoms of abuse. Once we identify those, we are going to have to tread lightly. Oftentimes, there is a stigma associated with mental health help. No one wants to concede that they are not strong enough to handle what has gone on in their life. As an RT developing rapport with that patient, especially with the frequent flyer patients, developing those relationships helps open that door to getting them the resources they need. Reaching out to the physician or referring for a psych eval is a very direct approach. It might work, but there is a potential to alienate the patient. I would personally also advocate for the nurse to be involved. One of our most overlooked resources in healthcare is the social services case management department. I have met some fantastic social workers in my years in practice. If we identify an issue, we might have a social worker help them identify resources inside and outside the hospital setting.
Many communities have seen a reduction in mental health resources. This is going to be a tougher sell. Social workers and case managers will be very helpful in navigating this and can access resources via insurance companies like Medicare and Medicaid.
I do not have a lot of pediatric experience. In this area, it is definitively about building relationships with the caregivers to build trust. You can take advantage of the five to seven minutes that you are giving a nebulizer treatment. It is all about interacting with the patient and caregivers to advocate for them on a broader scale.
We see patients all the time, and they'll say, "What do you suggest I take as a herbal supplement?" Or, "What do you suggest to help me stop smoking... reduce the stress levels...help me work through some issues that I experienced many, many years ago." There are many things that we can use to fill in the blank.
I think you summarized this well. It is building that rapport and trust because that is when education comes alive.
Yes, absolutely. I also think that collaborative research has shown that when we engage with what we call a two-generation model, whether it is the parent or the caregiver. We provide education on ACEs. There is always room for repair. Remember, what is predictable is preventable.
References
Available in the handout.
Citation
Kurszewski, T. (2021). Revisiting adverse childhood experiences: Is this the key to managing COPD. continued.com - Respiratory Therapy, Article 38. Available at www.continued.com/respiratory-therapy
