Editor’s note: This text-based course is an edited transcript of the webinar, Brain Injury Effects on the Respiratory System, presented by Sarah Busser, M.A. CCC-SLP.
Learning Outcomes
After this course, participants will be able to:
- Identify 3 neuroanatomical structures implicated in respiratory function
- Define 3 respiratory deficits that impact functional outcomes
- Explain 2 strategies for improving carryover and engagement in patients with brain injury
Neurophysiology
Central Nervous System
Encased in bone
- Brain
- Cortex
- Subcortex
- Brain stem
- Spinal cord
- Brain
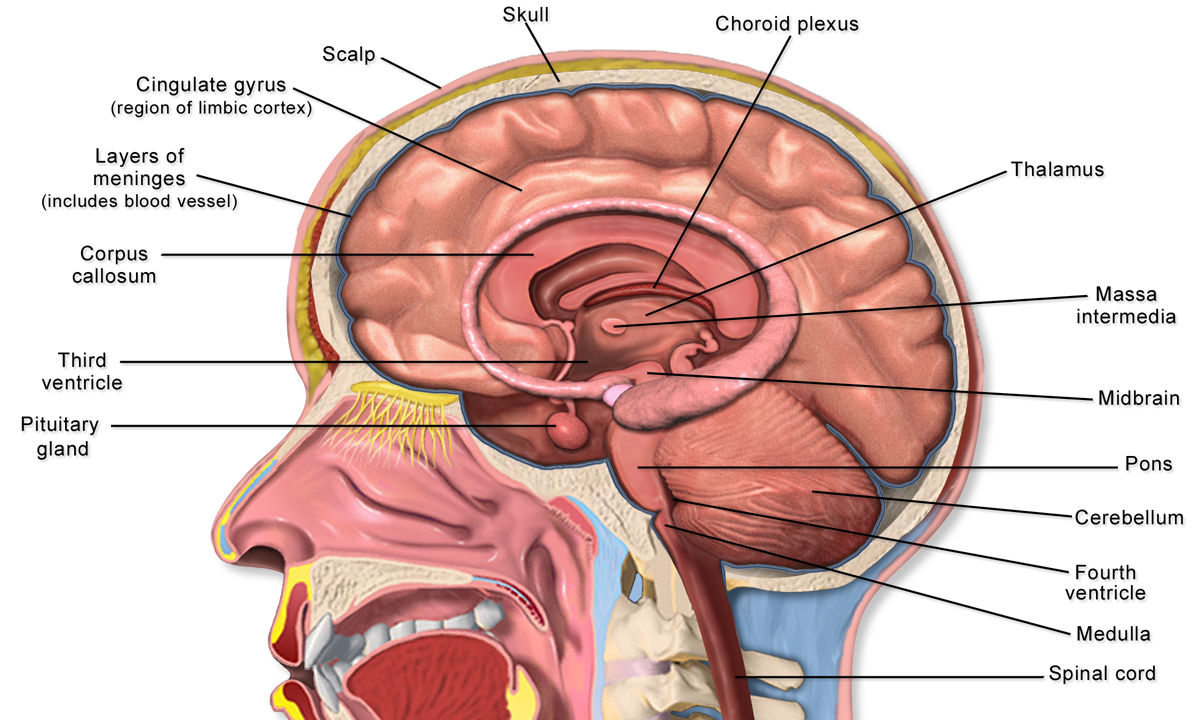
Figure 1. Structures of the brain (Source: Blausen.com CC BY 3.0 via Wikimedia Commons).
Let's talk a bit about neurophysiology as it relates to brain injury. We are going to start from the top with the central nervous system as seen in Figure 1. We have the brain encased inside the skull, and the main structures within the brain are the cortex, the subcortex, and the brain stem. Then within the spine, we have the spinal cord. These make up the central nervous system. Some of the critical features that I want to highlight in the cortex is the primary tissue in the outermost portion of the brain, primarily composed of gray matter and white matter.
- Cortex
- Primary motor strip (posterior frontal lobe)
- Primary sensory strip (anterior parietal lobe)
- Subcortex
- Amygdala
- Basal ganglia
- Thalamus
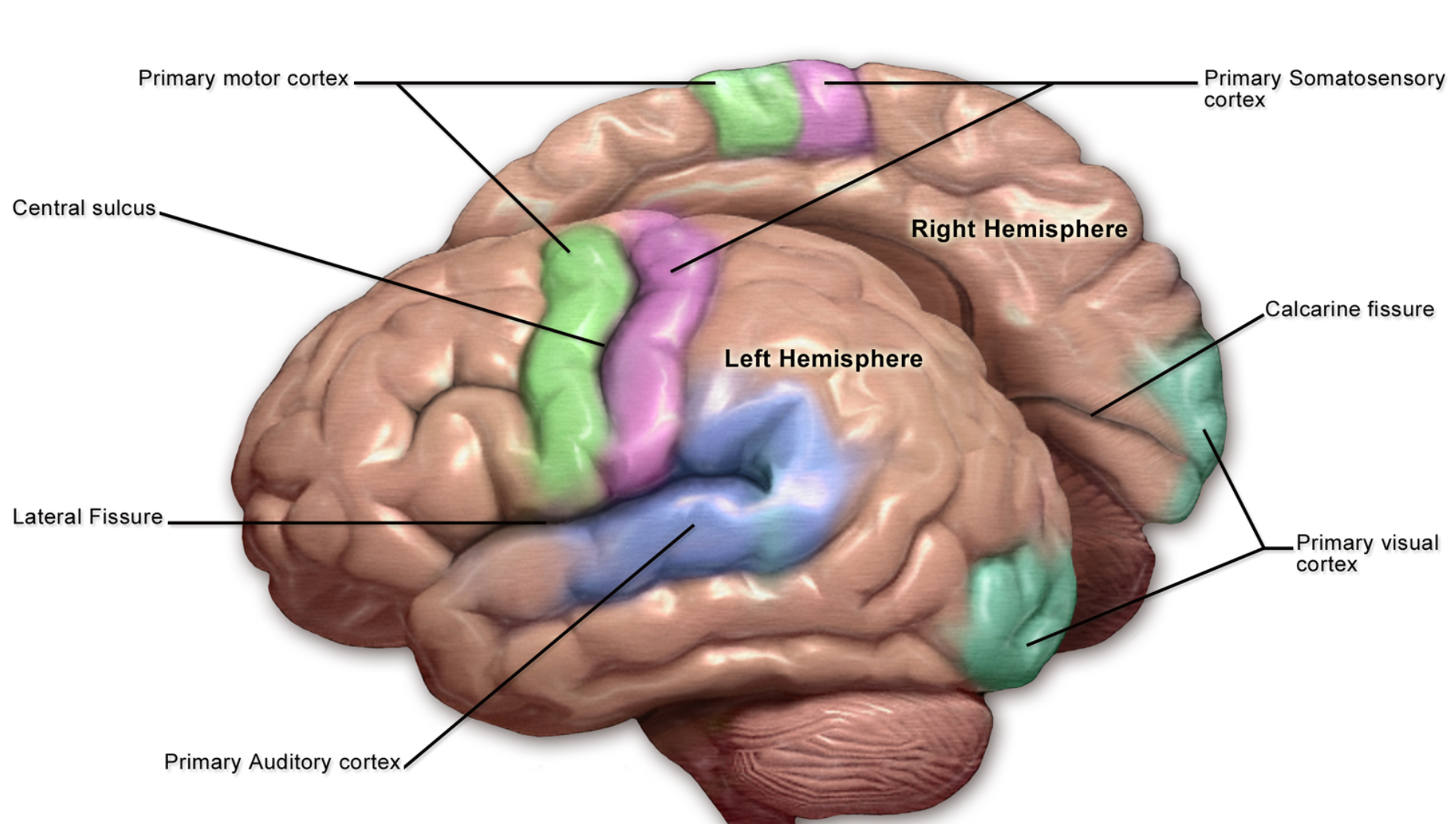
Figure 2. Brain Cortex (Source: Blausen.com CC BY 3.0 via Wikimedia Commons).
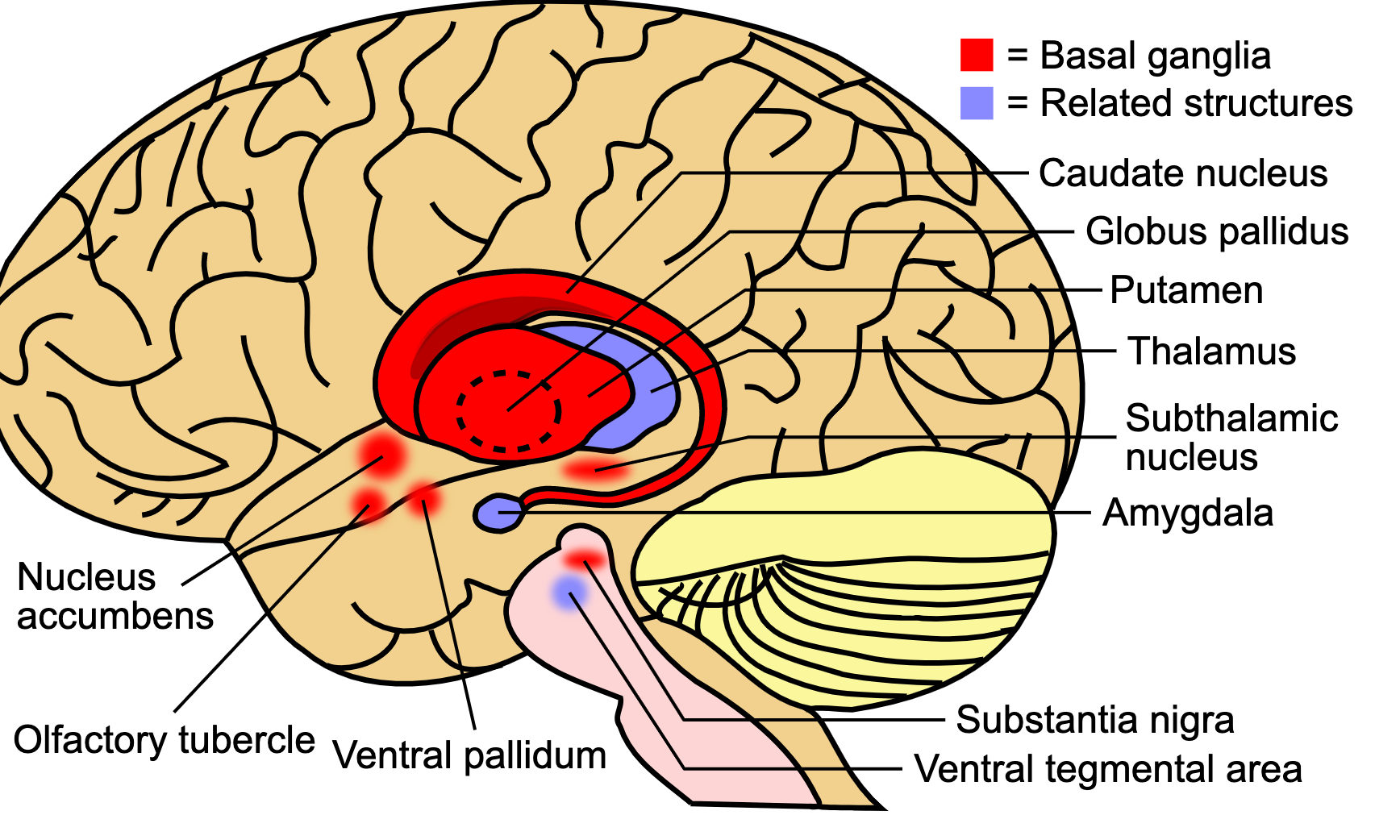
Figure 3. Brain Subcortex (Source: SUMI, CC BY 4.0 via Wikimedia Commons).
Two major players in respiratory function from the cortex are the primary motor strip, located in the posterior part of the frontal lobe, and the primary sensory strip, located in the anterior parietal lobe (Figure 2). I also want to highlight the subcortex in Figure 3, which is located beneath the cortex and is sort of in a structure almost like what I would describe as a peach pit. Think of a peach. You have the outer part. The meaty part that we like to eat is the cortex. And then, the subcortex is the peach pit, the innermost part.
We have three vital structures in both respiratory function and brain injury. The amygdala seen in Figure 3 is implicated in emotion and is often hyperactive or hypoactive with brain injury, we know that emotional lability and various states of arousal can certainly impact respiratory rate and function. We have the basal ganglia (see Figure 3), which is a group of cells that function to work on motor control and speed. If you think about the basal ganglia most often associated with Parkinson's disease, we can see changes in the movement amplitude with those folks. Within a brain injury, if there is damage to the basal ganglia, we may see respiratory deficits associated with that motor control. Then we have the thalamus (see Figure 3), the brain's relay station. It controls a lot of the information processing between the brain stem and the cortex. Moreover, it is super essential in many different aspects of function but connects with conscious control of respiratory function and our ability to control and process motor and sensory inputs from the brain to the rest of the body.
- Brain stem
- pons
- medulla oblongata
- Spinal cord
- Phrenic nerve
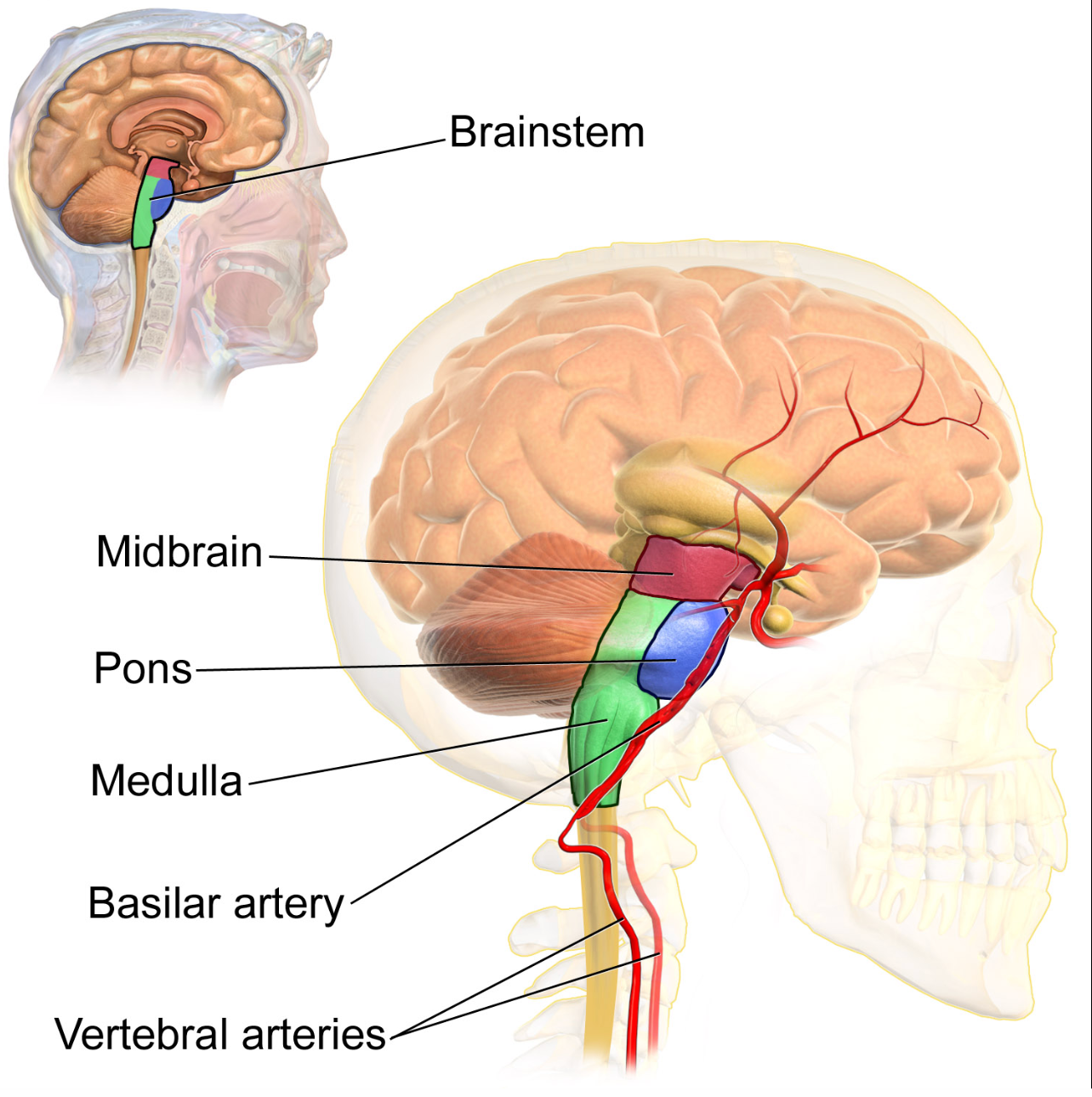
Figure 4. The brain stem (Source: Blausen.com CC BY 3.0 via Wikimedia Commons).
The brain stem in Figure 4 is directly underneath the subcortex. Furthermore, the two aspects of the brain stem that are most important for respiratory function are the pons and the medulla oblongata. We know that brainstem is associated with essential life functions and that the foundational control of respiratory function is derived from here. Direct injuries affecting the brain stem can have profound implications for basic respiration functions and other aspects of the respiratory system, like speech and swallowing. The spinal cord, which is still part of the central nervous system, is encased in bone and within that is the connection to the phrenic nerve. The phrenic nerve is super crucial for the control of the diaphragm. Injuries to the phrenic nerve can undoubtedly have severe implications for respiratory function and the ability to control and maintain the respiratory drive.
- Reticular Activating System
- brain stem ↔ thalamus ↔ cortex
- Disorders of consciousness
- brain stem ↔ thalamus ↔ cortex
Additionally, inside the central nervous system, a structure or group of structures work together to form the reticular activating system. The reticular activating system is a system that is important for fundamental consciousness. We have alterations in consciousness with changes to the reticular activating system. For someone in a coma, their reticular activating system is often not functioning properly. The reticular activating system is a network that courses through the brain stem, through the thalamus, the relay center, and then into the cortex. It is that "conscious control of respiratory function," and when there is dysfunction in the brain, often initially, we see that those functions can be depressed. Our more severe brain-injured patients will require mechanical ventilation. I want to highlight we see more severe impacts on the respiratory system with disorders of consciousness.
Peripheral Nervous System
- Nerve projections & ganglia
- Outside bony enclosures of skull & spine
- 2 major divisions
- Somatic
- Autonomic
The peripheral nervous system is the nerve projections and ganglia outside of the bony enclosures of the skull and spine. The central nervous system is housed within bones. You can consider central inside and then peripheral, meaning outside that area. These nerves and ganglia will be necessary for communicating helpful information from the brain and spinal cord out to the rest of the body. There are two major divisions of the peripheral nervous system, and this is where it can get a little confusing. I will try to keep it as simplified as possible because we have divisions within divisions here. We have the somatic nervous system and the autonomic system within this peripheral.
- Somatic- voluntary
- Autonomic- involuntary
- Sympathetic
- Parasympathetic
The word somatic is rooted in soma or body if we think about somatic. We want to think about the somatic aspect of the peripheral nervous system as our active and voluntary control of movement.
Autonomic Nervous System
“Automatic”
- Regulates
- Heart rate
- Respiratory rate
- Blood glucose
- Pupil dilation/constriction
- Regulates
The respiratory system is our active control of the lungs, whereas I always think about automatic, like auto, the autonomic nervous system. It is involuntary controlling our visceral organs and essential breathing that we are not controlling, not making any adjustments to, is regular breathing. Then, we get into that further division within the autonomic system that encompasses both sympathetic and parasympathetic. It is foundational to understand how the body responds to trauma. There are significant implications for the respiratory system. It regulates heart rate, respiratory rate, blood glucose, pupil dilation, and constriction.
- Sympathetic
- Fight or flight
- Parasympathetic
- Rest & digest
We have the two divisions of the sympathetic nervous system. I am sure you have heard the term "fight or flight," which becomes activated when the sympathetic nervous system (Figure 5) is engaged. We can see that may cause us to be in a state of hyperarousal, particularly with brain injury patients, as they are moving through levels of consciousness and changing their overall level of function. On the other hand, the complement to the sympathetic nervous system will be our parasympathetic nervous system (Figure 6), the "rest and digest" aspect.
- Sympathetic
- “Fight or flight”
- ↑ respiratory rate
- ↑ heart rate
- ↑ blood glucose
- pupils dilate
- inactive gut
- “Fight or flight”
- Parasympathetic
- “Rest & Digest”
- ↓ respiratory rate
- ↓ heart rate
- ↓ blood glucose
- pupils constrict
- active gut
- “Rest & Digest”
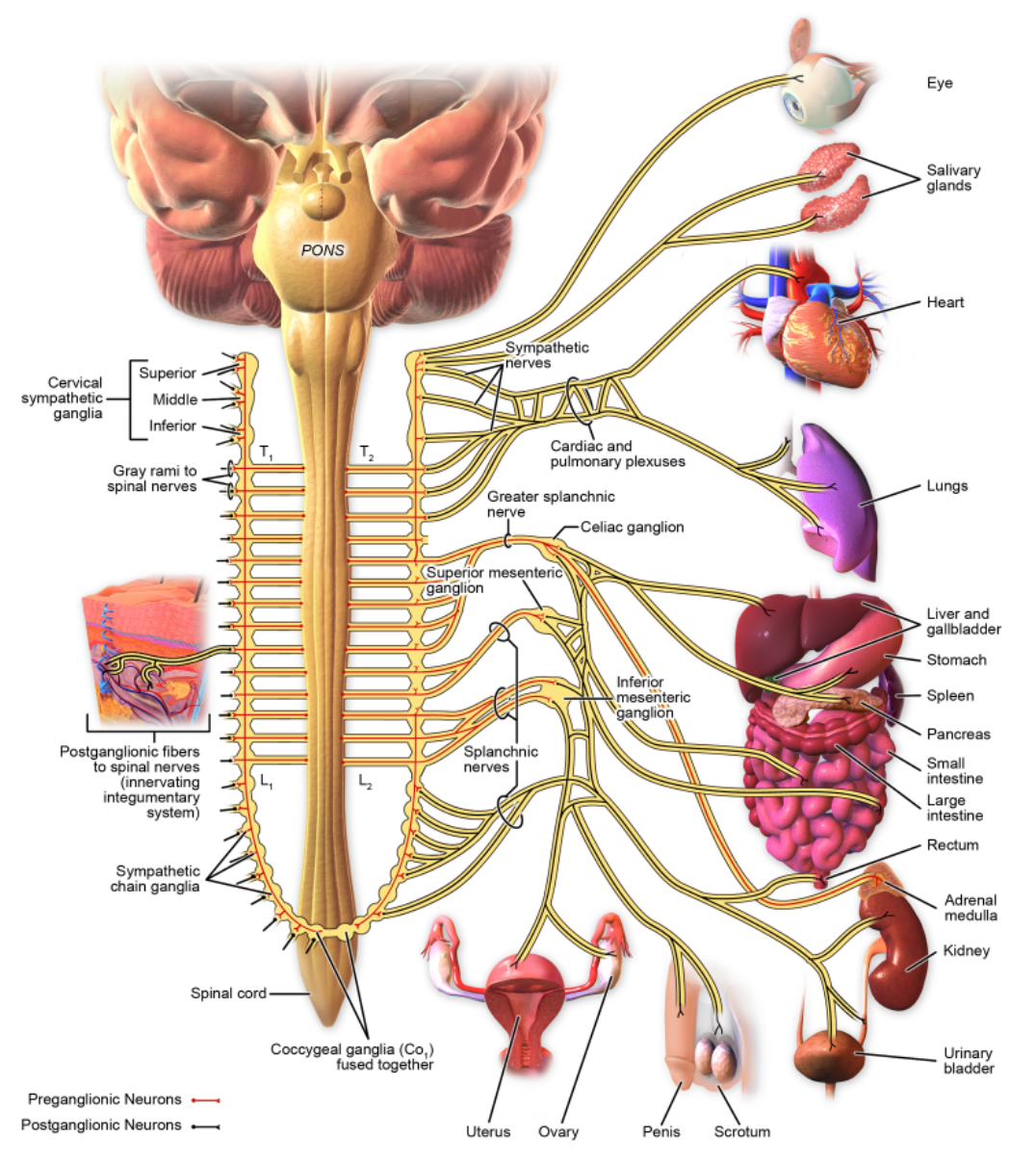
Figure 5. Sympathetic System (Source: Blausen.com CC BY 3.0 via Wikimedia Commons).
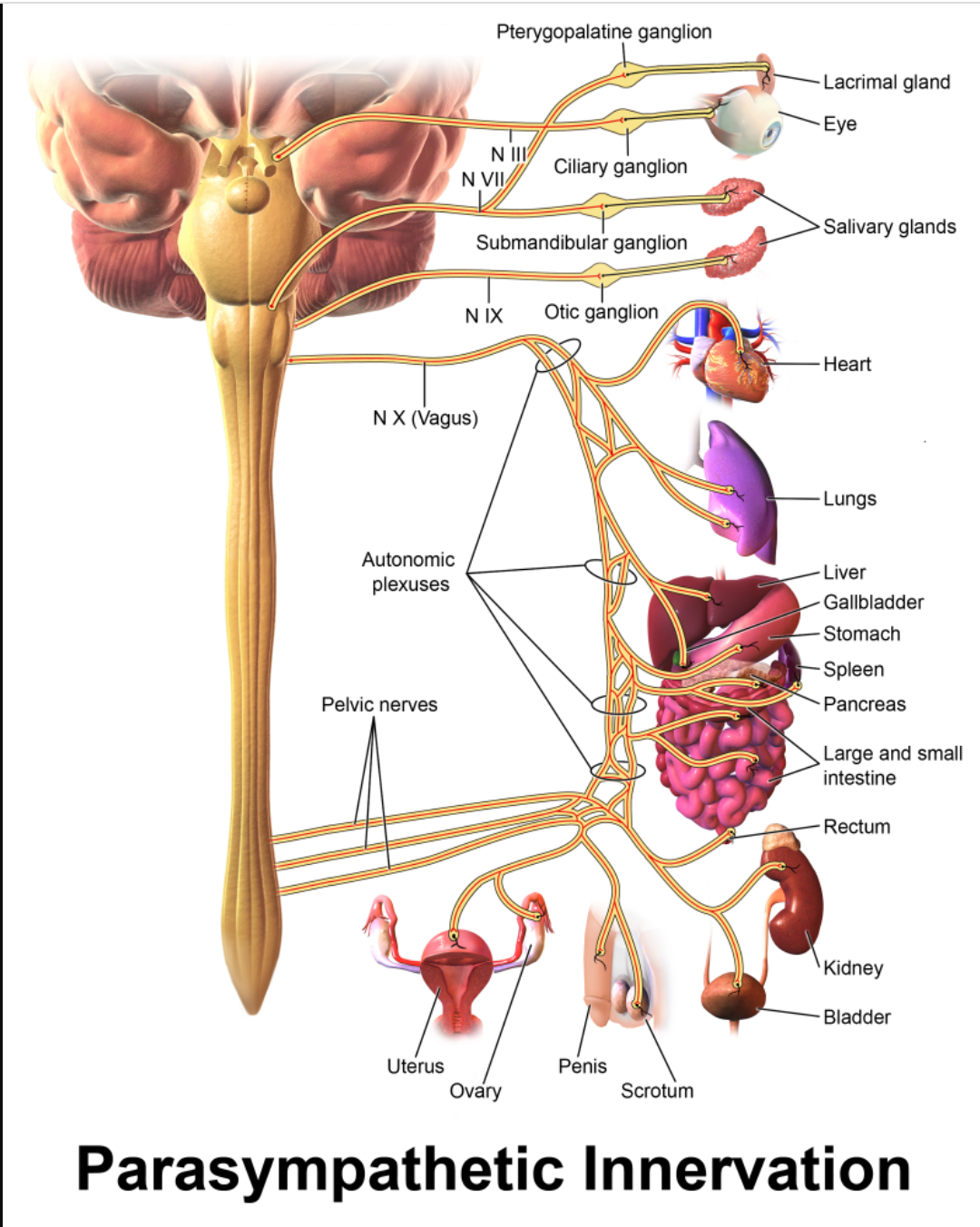
Figure 6. Parasympathetic System (Source: Blausen.com CC BY 3.0 via Wikimedia Commons).
On the other hand, we have the parasympathetic nervous system, the "rest and digest." It is complementary because everything is pretty much the reverse of what we see with the sympathetic nervous system. We see a decreased respiratory rate. Our respiratory rate decreases with sleep, heart rate, and blood glucose production. The pupils constrict, keeping the light out so that we can sleep. A more active or busy gut allows for digestion to occur and absorb nutrients. When that sympathetic nervous system is hyper-aroused, it will be more difficult for our body to absorb what we need to have long-term nutrition and storage of what is important because those spikes in blood glucose can give us a burst of energy. However, building up muscles and responding in a rehab situation is not that beneficial in the long term.
Brain Injury
Types of Brain Injury
- Disorders of Consciousness
- Coma
- No sleep/wake cycles on EEG
- Coma
- Vegetative State
- Spontaneous eye-opening
- recovery of the Reticular Activating System
- Spontaneous eye-opening
Let's talk more about different types of brain injury because we certainly know there are many levels and ways these folks may present to us. The most severe disorder of consciousness is also known as "DOC." Frequently, there will be these types of patients in a level one trauma center, potentially level two. Specific facilities tend to work with these patients in the rehab process. Depending on what types of facilities you worked in, you may or may not have had much interaction with this type of patient. Let's talk about what these levels of consciousness are and what differentiates these people. Coma, they are not responsive, but also, on a deeper level, we know that we can determine someone is still in a state of coma when there are no sleep or awake cycles on an electroencephalogram (EEG). An EEG measures the electrical activity of the brain. It does not require us to interact with the patient to know where we are in the process of recovery. In the later stages, a vegetative state, also referred to as a persistent vegetative state (PVS), is differentiated from a spontaneous coma by spontaneous eye-opening, indicative of recovery of that reticular activating system. We receive connections from the brain stem through the thalamus and into the cortex that allows the eyes to open. We have some degree of consciousness developing.
- Disorders of Consciousness
- Minimally Conscious State
- Clearly discernible AND reproducible evidence of :
- Simple command following
- Intelligible verbalization
- Recognizable verbal or gestural “yes/no” responses (without regard to accuracy)
- Clearly discernible AND reproducible evidence of :
- Minimally Conscious State
We will talk about a minimally conscious state, known as MCS. A minimally conscious state is coming more and more into public awareness. For many years, we had people either classify it as coma or vegetative state and then we would go right into Rancho levels, which are different levels of participation with brain injury. However, there was no in-between to talk about these folks who are considered lower-level functions but are conscious and able to show some consistent level of participation. I found this important, being able to differentiate a vegetative state versus a minimally conscious state because it can be helpful for us in the rehabilitation process to know what the prognosis for recovery is.
Certainly, someone minimally conscious shows us that recovery is occurring and that we are proceeding towards higher levels of brain function that the cortex is connecting with the rest of the brain stem and the body. That is a critical differentiation. What does minimally conscious mean by definition? The most important things we see are discernible and reproducible evidence to see them done more than once, not spontaneously. Discernible AND reproducible evidence of simple command following, intelligible verbalization, and recognizable verbal or gestural yes/no responses. This is without regard to accuracy. If you ask the individual with brain injury, "Are you a man," and the correct answer is yes, but they say no, they are still verbalizing a "yes or no." It is not correct, but they are responding appropriately. We often describe this as an appropriate response to that question, just not the correct one. Often, rehab professionals working with these patients will use something like the coma recovery scale to monitor the patient's response. We have to make sure they are not sedated when we give this type of testing. It allows us to assess for various functions and monitor if the person progresses from a vegetative state to a minimally conscious state and beyond. Ensure that we are providing accurate prompting to get the responses. We know there can be those times when something will occur that is spontaneous. The person might smile or move their foot. It can happen, but we want to be tracking it as much as possible and show that it can happen with some interaction with the environment, not just reflexively. Very important for us to know and help participate in evaluating these patients for both the team and when we are communicating with families.
- Diffuse Axonal Injury
- Focal injuries:
- Epidural hematoma
- Subdural hematoma (SDH)
- Subarachnoid hemorrhage (SAH)
Another type of brain injury is diffuse axonal injury (DAI). DAI is a severe brain injury primarily affecting the white matter. The white matter is in the cortex, that outermost part, remember the peach analogy, is the meat of the peach, the part that we eat. The white matter is the axons, which are nerve conducting pathways. I think of those as the "superhighway for information." To get higher-level consciousness and higher-level activities, we need to have those superhighways functioning as well as possible. When damaged, I often refer to them as things being "under construction." There are speed bumps, detours, potholes, and things are not going smoothly on that path, and that is how we have disruptions in our ability to understand information and process higher-level information.
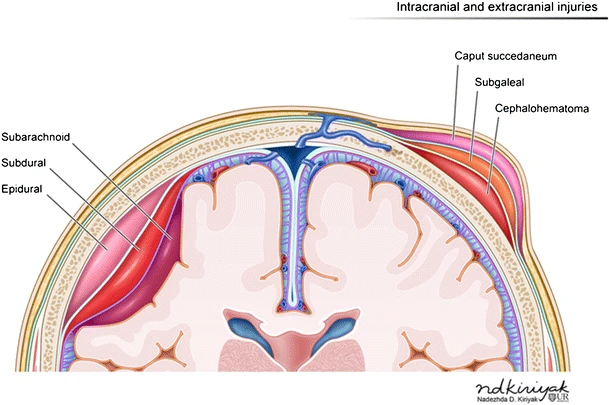
Figure 7. Illustration of intracranial and extracranial injuries (Source: Nadezdha D. Kiriyak, CC BY 4.0 via Wikimedia Commons).
We often see diffuse axonal injury when it is more severe in people with severe consciousness disorders. Focal injuries can vary. If there is only one focal injury, that is relatively small. We may not see a severe impact on the overall level of function. However, when these are seen in combination with one another or multiple, we can see more severe damage. The location and size, as with any brain injury, will be important in how the level of function is affected in Figure 7. An epidural hematoma is a collection of blood outside the dural, like a protective layer that helps with shock absorption. It is usually lens-shaped and often does not have significant implications for the overall level of function because it is several layers outside. If it grows too large, we can see issues with function.
Subdural hematomas (SDH) are relatively common as far as brain injuries go, especially among the elderly. We also see these with motor vehicle accidents, and these are collections of blood that happen between the layers. It is below that dural lining underneath the skull and above the brain. These frequently can expand and cause significant pressure on the brain. When these become very large, we will frequently have a craniotomy situation. Again, these are pretty common with elderly falls. Sometimes, brain atrophy that occurs with normal aging can go undetected. Because of that atrophy over time, there is extra space between the dura and the skull, which allows for blood collection without significant pushing onto the actual cortex. Every once in a while, we will see someone that had a fall or was in a car accident, did not have any signs or major issues at the time, but maybe months or even years later, they may have something happen where they get a CT of their brain and come to find out, there is a chronic injury there. There is an old collection of blood. Subarachnoid hemorrhage (SAH) will affect the brain tissue even more. When a SAH becomes large, it certainly can cause significant disruption in brain function.
Brain Injury & Respiratory System
- Direct trauma
- Disrupts neural control of the respiratory system
- Peripheral trauma
- Directly affecting trachea, lungs, diaphragm, accessory muscles
- Neurochemical cascade response
- Secondary reactions cause further dysfunction
Brain injury can have various implications for the respiratory system. It can disrupt the neural control of the respiratory system. We said, not only the cortex, but the brain stem can cause significant issues with the overall ability to function respiratory-wise. We can have peripheral trauma affecting the trachea, lungs, diaphragm, and accessory muscles for breathing. Any disruptions or damage, whether it is a penetrating injury, can cause further respiratory function issues, especially when dealing with multi-trauma patients. We have the neurochemical cascade response that occurs in response to a brain injury. The body is trying to respond to this trauma, and in doing so, there is a chain reaction of various chemicals in the brain and neurotransmitters that, unfortunately, if they continue to kind of spiral, can cause secondary damage. That secondary damage to the brain can cause further disruptions to the respiratory system and the potential for respiratory failure.
Early Intervention
- Tracheostomized & mechanically ventilated patients
- Establish communication
- Determine the level of cognitive function
- Initiate swallowing treatment
- Decrease time on vent
Let's talk about some early interventions with our brain injury patients. Many of these patients have respiratory failure, especially more severe, and prolonged mechanical ventilation. We may need to do a tracheostomy and then attach mechanical ventilation through the tracheostomy. What are some things that we can do to help these patients? We want to establish communication, whether through gestures, writing, or the use of a speaking valve, and determine their level of cognitive function. We are all working together to assess what this patient can do. Is it reproducible, or is it just spontaneous involuntary reflexive movements? We can initiate some swallowing treatments. That may just start with some basic exercises and then move towards the initiation of pill intake. In early intervention, we want to do everything we can to help decrease these patients' time on the ventilator, which is a team effort. We will talk more about what we can do to facilitate that.
Speaking Valve
- Can be used inline with tracheostomized mechanically ventilated patients
- Early communication
- Improve secretion management
- Improve cough strength
Speaking valves are a wonderful tool that can be used in-line with tracheostomized patients on a mechanical ventilator. The valve can be attached to the ventilator tubing and allow the patient to communicate, improve their secretion management and improve their cough strength. Using the valve is something that can be done with an interdisciplinary team. We love our respiratory therapists working with these patients and helping them improve these essential functions, decrease their time on the ventilator, and help the individual with their cognitive function. Respiratory therapists using the speaking valve help orient and better assess how their cognitive functions are working. We can reduce that ICU delirium and help them in many ways. A great tool that we have as an interdisciplinary team.
Respiratory Muscle Strength Training
- Spring-loaded pressure threshold devices
- Inspiratory & expiratory
- Speech & swallowing implications
Respiratory muscle strength training (RMST) is another great tool. RMST can be used with patients early on, who are having failure to liberate off the ventilator and who are tracheostomized. There are contraindications, but many, especially younger patients who are not severely cognitively impaired can be great candidates for RMST. There are inspiratory pressure threshold devices as well as expiratory ones. Inspiratory is more training the muscles associated with the diaphragm and working for those who have voice disorders, which can be helpful. Then the expiratory muscle strength training is working to bring the vocal cords together, adduction. If you think about it, if a patient is bearing down, then they have to adduct their vocal cords together in order to create pressure within the body. This same effect is needed for coughing. We see with weakness and disuse atrophy the cough certainly becomes disrupted. We have issues with creating a good forceful cough. These pressure threshold devices can be beneficial for these patients to get their function back. Certainly for swallowing we know that the vocal cords coming together is important to prevent aspiration and to make swallowing as safe as possible.
Dysphagia Assessment
- Alertness
- Cognitive-communication function
- Cranial nerve function
- Dentition & oral health
- Respiratory status
- Overall medical/physical condition
I wanted to share with you more about what happens with swallowing dysphagia assessments because I get many questions about what exactly you guys are looking for when you are doing this? How can respiratory therapists help because we know they are so intertwined, the respiratory function and the swallow function? I have had so many wonderful respiratory therapy colleagues who have helped me with monitoring how well the patient is doing, alerting us to patients that may not have been flagged for an assessment that would benefit.
Alertness
- Sedated/obtunded
- Arousable with stim but difficulty maintaining
- Awake but confused/delayed processing
- Awake & alert
Foundationally, we are looking at alertness. That is important, but I do not want the patient obtunded, as varying levels of alertness can impact safety, cognitive-communication function, cranial nerve function, and oral health. Respiratory status is vital, then their overall medical and physical condition. We may be seeing different levels of alertness with these brain-injured patients, sedated or obtunded when we are at that low level of arousal.
We do not want to have them necessarily swallowing anything if not arousable with stimulation, and having difficulty maintaining that level of arousal is common, especially as we are weaning off sedating medications. Awake but confused or delayed processing is common, transitioning to the most optimal state, awake and alert.
Cognitive-Communication
- Impulsivity
- Poor insight
- Agitation
- Disorientation
Some aspects of cognitive-communication skills that we are looking at that impact our swallowing evaluations, such as impulsivity. If the person is constantly grabbing for things and does not have good insight into their deficits, then we can have concerns that they will be the ones shoveling food into their mouth or chugging their drinks when they are not quite ready to be doing that. Those with agitation and behavior issues, which are often associated with confusion, can make it challenging to maintain nutritional needs when that high level of arousal prevents us from engaging that digestive system, as we discussed earlier, with the sympathetic versus the parasympathetic nervous system.
If the person is confused about where they are, disorientation can lead to further agitation—not knowing what time. The meal is here, it is time to eat, and they think it is time to go to bed. They are not interested in participating in mealtime because of disorientation which can have implications for us.
- Aphasia
- Expressive
- Receptive
- Communication strategies
Another aspect of cognitive-communication that we will look at is aphasia. Aphasia is a whole another topic, but just considering its basics, expressive aphasia is when we have difficulty getting any words out or the words we can get out are incorrect. They may say "bog" instead of "dog," "tan" for "man," or say "woman" instead of "man." Receptive aphasia is when they are having difficulty comprehending things.
Like Wernicke's aphasia, some of them may talk fluently and can frequently conceal their deficits by doing this. What they are saying may not make much sense, but they often have good social awareness and can say, "uh huh," "yeah," "okay," "I got it," but do not have a good understanding. They think that everybody else is not making sense, and they do not understand why we are telling them what you are saying does not make sense, which can further increase agitation. Something to be on the lookout for as some of them can be very good at saying, "yeah, okay." They have that good cognitive function and social skills to get by but poor overall comprehension. When working with a patient with aphasia, which is typically associated with brain damage to the left hemisphere, communication strategies like writing things down, gesturing, and identifying keywords can benefit these folks. Certainly, talk with your speech pathologist if you have one available to find out more about what works best for your patient.
- Communication boards
- Yes/no systems
- Writing
I know that communication boards are often requested. There are all different levels of complexity with communication boards, and it can be a little bit tricky. When the person has severe deficits, they may not understand the association between pictures and words. So that can be tough for both the patient and providers. Establishing a consistent yes/no system is important. Making sure that across providers, if we are doing yes/no through thumbs-up, or whether it is "blink once, blink twice," we want to make sure we are consistent so that we keep things the same across providers as much as possible and not confuse the patient. Writing can also be another modality that can be useful to supplement both our communication and the patient to engage in.
Cranial Nerve Function
- CN V- Trigeminal
- CN VII- Facial
- CN IX- Glossopharyngeal
- CN X- Vagus
- CN XII- Hypoglossal
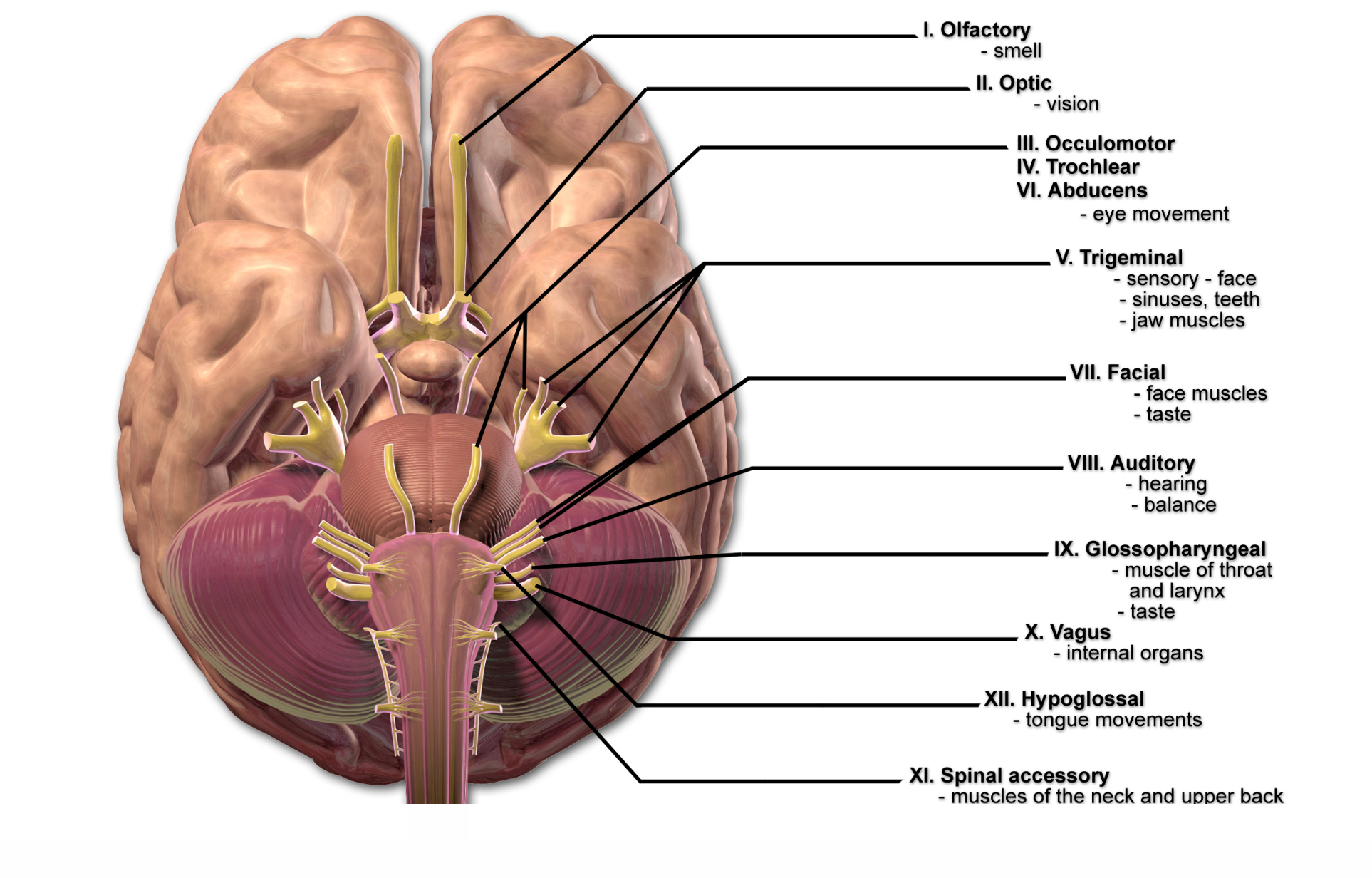
Figure 8. Cranial nerves (Source: Blausen.com CC BY 3.0 via Wikimedia Commons).
Let's look at cranial nerve function in Figure 8. There are five in particular that we are looking at that are essential for swallowing and speech function. Assessment of how well these are operating and any potential injuries to the nerve itself or the structures associated with them are things that we want to be aware of. Cranial nerve V is the trigeminal nerve. That is responsible primarily for sensory function in the face. The trigeminal nerve involves facial injuries, and head trauma can affect this.
Cranial nerve VII, the facial nerve, is primarily going to be the motor function of the face. Cranial nerve IX, the glossopharyngeal nerve, is associated with the tongue and the pharynx. Cranial nerve X, the vagus nerve, is crucial across many levels. Vagus refers to the root word "vagabond" or "wanderer" because the vagus nerve travels down from the throat muscles, through the trachea, around the heart, and into the gut. When there is damage to the vagus nerve, that can have significant implications for many function areas, including the respiratory system, because it is located in the medulla. Cranial nerve XII, the hypoglossal nerve, is responsible for most of the tongue's functions, a significant player in swallowing and speech function.
Dentition & Oral Health
- Window into overall health status
- Link to aspiration pneumonia
- Dry mouth= more bacteria
We will be looking at dentition and oral health. Something many of my respiratory therapists are great about assessing. We know that the oral cavity can be a window into our overall health status. We know that when we see much decay and poor condition of the teeth and mucosa, that can give us some clues as to how well this person was functioning and how well they are functioning now. When we have a parched mouth and many secretions, we know that there is the possibility that this person is at a much higher risk for developing aspiration pneumonia.
Oral Care
- Toothette vs toothbrush
- Lemon glycerine swabs
Oral care can be an important factor in reducing aspiration risk. I work with many great respiratory therapists who help me out with oral care, keeping the mouth clean, and helping our nurses out. I wanted to highlight a couple of things that we have learned throughout the years with oral care that are important. We have found that the toothette, those little sponges, are great for moistening things and helping to do the foundational work for oral care, but ultimately, to remove that bacterial film, we need a toothbrush. If you have access to a soft toothbrush or those oral care kits, which are great, having the swabs and toothbrushes can be attached to suction. Those are wonderful tools that can help reduce that bacterial load to lower the risk for pathogens entering the respiratory tract. The toothbrush is far superior to the toothettes.
I wanted to touch on lemon glycerin swabs because I know these were popular and still are in some facilities. However, we have found that the acidity of the lemon is potentially damaging to the actual dental enamel and that this can cause further dryness. Lemon glycerin swabs are not ideal. I have seen many hospitals start to get away from having them in stock because they were popular for a while, but now we have research to show that they can be damaging. Sometimes they can be used to help stimulate swallow function, but it is overall important if these are going to be used that we then go ahead and do oral care with a toothbrush afterward to remove the acid and any drying properties from these.
- Denture removal
- Sleeping in dentures doubles the risk of pneumonia (PNA)
- Lower partials can be swallowed
- Check mouth prior to intubating or applying non-invasive ventilation masks
Dentures are another essential piece of oral care. When assisting with that, be aware of the different respiratory devices. A study included in the references talks about how sleeping with dentures doubles the risk of pneumonia. You can also imagine that when we have a sedated patient or a patient with a low level of function, keeping those dentures in can cause further issues. Unfortunately, I have seen several cases where the lower partials have been swallowed. I had a patient within the past year who was a very low level of arousal and low level of function, whose voice was very muffled. She was having throat pain. I had seen this happen before. I said to her, "Do you wear dentures? Yeah, they're in my mouth." Well, it turns out that she had significant respiratory issues. She had been on Bipap. We do not know for sure what happened, but we suspect that potentially the pressure of the Bipap had blown them back into her pharynx. Her gag reflex was not sensitive enough to respond. We know that with the pressures of Bipap, it would be difficult for anyone. They ended up stuck in her throat, and the patient went in to remove them in the operating room. We do not want that to happen. Lower partials look like little retainers, and the upper is typically more difficult, but I cannot say I have not seen it happen. If you just Google "swallowed dentures," there are many disturbing photos. Keep that in mind. Whenever you are going into someone's mouth, take the dentures out.
Respiratory Status & Dysphagia
- Respiratory rate
- Cough effectiveness
- Voice link- CN X Vagus
- Oxygen delivery modes & dysphagia
Another thing to keep in mind is respiratory status and dysphagia. We know that respiratory rate and swallowing function are closely linked because to swallow, we have to be able to hold our breaths. When we have a respiratory rate over 30, we have to hold our breath for 1 to 2 seconds to swallow. That means a respiratory rate of 30 requires us to breathe every 2 seconds within that minute. If we have to hold our breath and breathe that quickly, then it increases the likelihood that that person, rather than exhaling, which is the normal pattern after swallowing, is going to gasp for a breath. It is going to be more challenging for them to manage. Now, a respiratory rate of 30 is the benchmark where we start to look for potential trouble. It does not mean, "No, they cannot swallow." There is a high risk for aspiration when we get above 30, into the 40s, and beyond.
We also look at cough effectiveness, which is linked to their voice. Should the person is unable to voice. They either have a mechanical injury to the vocal cords or potential Cranial Nerve X injury, the Vagus nerve responsible for the vocal cords being able to "adduct" or come together to voice. Potentially, airway protection may be impaired, primarily mediated by the vocal cords coming together. Keep that in mind.
- Bipap
- Small-bore dobhoff
- Switch delivery mode for feeding
People requiring noninvasive ventilation, BiPap, struggle with their breathing. I have seen some success with small-bore dobhoff tubes with the mask on top and maintaining enough seal. If the person is not tolerating or completely backs down on BiPap, potentially switching the mode of delivery of oxygen for the person to eat, if they can tolerate it, is optimal. Sometimes we will try to remove the mask quickly, get something in, have them swallow, and turn it back on, but that is not ideal because then we are forcing that pressure, and any residue could potentially be aspirated. Ideally, we would like to have them on either a high flow, a nasal cannula of some kind in order to, again, maintain enough oxygen while they are eating because we know that can become an aerobic activity pretty quickly, or they may need to consider an alternate means again.
Oxygen Delivery Modes & Dysphagia
- High Flow Nasal Cannula
- Risk for feeding/swallowing with higher pressures?
Some literature suggests that there is potential for increased risk of aspiration when we get into those high pressures with high flow nasal canulas. If the person is on 70, or 80 liters per minute, they are probably not a great candidate for swallowing. Individual results may vary, but they will be more critically ill if in that situation, so swallowing may not be the priority.
Overall Medical Status
- Underlying comorbidities
- Acute conditions
- Mobility
- Immune system function
We also look at the medical status serving multiple functions. Assessment of underlying comorbidities and acute conditions. What are we treating? What is their mobility status, and is their immune function compromised?
Strategies for Treatment
Principles of Neuroplasticity
- Use it or lose it
- Repetition
- Intensity
- Salience
Let's talk about some strategies for treatment that can be beneficial for respiratory therapists. I wanted to highlight the principles of neuroplasticity. There is more than this, but these are some of the ones that I find are most important, especially when we are dealing with more severe brain-injured patients. "Use it or lose it." For someone to maintain their highest level of function, they have to continue to use it.
We talk about this a lot with swallowing if you are not swallowing at all, you start to develop disuse atrophy, including those respiratory muscles. When we have that acute decline in function, if they are on the ventilator and the machine is working for them, we do not have the same level of function as we are transitioning off. We need to engage in activities that will promote the continued use of these muscles. Repetition and intensity are super important. We do not want to have them do that simply one time. We want to have them do it multiple times, keeping in mind their tolerance, but to best map out better brain function, we want to do things more than once to help engage those pattern generators in the brain.
Salience is making something meaningful to the patient, giving them the "why." Why are we doing this? Why does this matter, and how does helping them connect it to something that they want to be able to do? When we are talking about breathing treatments, as an example, you need to be able to improve your breathing to swallow, walk, and do the things you want to do to be independent—making that link to understand better why participation is necessary and can be beneficial. Often, disorientation, memory issues, and cognitive impairments can occur in brain injury patients in which hyperarousal of the sympathetic nervous system is often present.
Establish Trust
- Introduce yourself
- Orient
- Explain step-by-step what is going to happen next
There can be a lot of difficulty engaging with people unfamiliar to them, all of us as medical professionals. There are so many of us. We have physicians and different therapists. Establishing trust from the minute you walk in the door is essential. You are introducing yourself, even if you have been there multiple times. Also, some of these patients are kind of "fake it till you make it" mode. They may act as if they know you but not remember your name and not tell you that because they will want to seem as appropriate as possible. Help orient them. We usually try to keep the date current on the boards, letting them know what time it is and what is going on as much as possible for those who are very confused and disoriented, trying to walk them through what we are going to be doing step by step. We are going to be putting this mask on you. I need you to take some deep breaths for me. It does not necessarily need to be complex, but just letting them know as things are happening, especially with suction or things that can feel a little more invasive. Trying to talk them through it can be beneficial. Participating in treatment promotes independence.
Promote Independence
- Hand-over-hand guidance
Using hand-over-hand guidance can be helpful. I talked about suctioning. Rather than having the patient sit back and you are placing the suction in their mouth, instead try to engage them by taking their hand and putting your hand over it to help them do it. Same with brushing their teeth. Whenever something is coming at their face, that hypervigilance can be engaged. We know how often we get swinging and pushing with those more confused patients. I have found that helping them engage again by putting it in their hand and helping guide their hand up to their mouth can help reduce that. If they cannot do it at all, let me help you. At least they see what you are trying to do, which can help ease those fears and let them participate better. I honestly have found that an effective tool to get those tasks done. Ultimately, that is what we are here for. We do not have all day, but if they are combative with us and we cannot do it at all, we know that we are potentially going to have more problems down the road and need more treatments. The benefit is for both us as professionals and for the patient.
Model and Give Feedback
- Gestures and demonstration
Modeling and giving feedback by using gestures, especially for patients with aphasia or difficulty understanding what is going on or who have hearing impairments, whether at baseline or from the injury, to show them what we want to do often can be helpful.
Maintain Safety
- Subtle signs of agitation
Maintaining safety is our number one priority. As professionals, we deal with many patients who are confused and can be agitated. Being aware of those subtle signs of agitation- the person becomes withdrawn or closes their eyes. We want to be aware of those to keep the patient safe and keep ourselves safe. Knowing when to step away and give the person a break is essential.
Repetition, Repetition, Repetition
- Orientation
- Review of how to use devices
- Education on the “why”
Repetition, repetition, repetition is critical. Frequently, these patients will be able to "kind of" socially engage in a way that may make you think they are more oriented than they are. Review orientation information, and review how to use devices as much as our time allows. Perhaps, going over how to use the incentive spirometer—educating them as we are able on the "why." Why this is important, why does this matter to you, and how this is going to help you? These are all things that we can do as therapists. We are helping both our patients and ourselves to maintain our productivity.
Questions and Answers
Do the "flight and fight" signs occur at certain stages of a brain injury?
If we are familiar with the Rancho levels, frequently that transmission from that coma, vegetative, minimally conscious state, we start to see more and more of that fight or flight coming into play. When we get into levels three and four, those patients become agitated. This is partly due to the confusion and disorientation and because those systems are starting to come back into play, and we can see more sympathetic nervous system hyperactivity occurring. That can fluctuate during the time of day and the stages of recovery.
What are disturbances in sleep-wake cycles?
We get those patients who are up all night and then sleeping all day and trying to figure out what is happening. That can also be related to disruptions in the nervous system. Communicate with the team as to what you see. Respiratory is in there so frequently on those scheduled times that they can help us tease those things out. In contrast, speech may only be in there once a day, optimally in the acute phase, maybe for more extended periods in a rehab setting, but still having that information about "They were agitated this morning, worked themselves up and then fell asleep," we can optimize our treatment, get the most out of it for them. That is beneficial information.
References
Bender, A., Jox, R. J., Grill, E., Straube, A., & Lulé, D. (2015). Persistent vegetative state and minimally conscious state: a systematic review and meta-analysis of diagnostic procedures. Deutsches Arzteblatt International, 112(14), 235–242.
Gupta, A., Gupta, A., Singh, T. K., & Saxsena, A. (2016). Role of oral care to prevent VAP in mechanically ventilated Intensive Care Unit patients. Saudi Journal of Anaesthesia, 10(1), 95–97.
Iinuma, T., Arai, Y., Abe, Y., Takayama, M., Fukumoto, M., Fukui, Y., Iwase, T., Takebayashi, T., Hirose, N., Gionhaku, N., & Komiyama, K. (2015). Denture wearing during sleep doubles the risk of pneumonia in the very elderly. Journal of Dental Research, 94(3 Suppl), 28S– 36S.
Meurman, J. H., Odont, D., Sorvari, R., Odont, D., Pelttari, A., Rytömaa, I., ... & Kroon, L. (1996). Hospital mouth‐cleaning aids may cause dental erosion. Special Care in Dentistry, 16(6), 247-250.
O'Reilly M. Oral care of the critically ill: a review of the literature and guidelines for practice. Australian Critical Care: Official Journal of the Confederation of Australian Critical Care Nurses. 2003 Aug; 16(3): 101-110.
Pear, S., Stoessel, C. K., & Shoemake, S. (2007). The role of oral care in the prevention of hospital-acquired pneumonia. Infection Control Today, 11(10), 1-3.
Rowshani, B., Timmerman, M. F., & Velden, U. V. (2004). Plaque development in relation to the periodontal condition and bacterial load of the saliva. Journal of Clinical Periodontology,31(3), 214-218.
Wang, Z., Wang, Z., Fang, Q., Li, H., Zhang, L., & Liu, X. (2019). Effect of expiratory muscle strength training on swallowing and cough functions in patients with neurological diseases: A meta-analysis. American Journal of Physical Medicine & Rehabilitation, 98(12), 1060–1066.
Zasler, N. D., Katz, D. I., & Zafonte, R. D. (Eds.). (2012). Brain injury medicine: Principles and practice. Demos Medical Publishing.
Citation
Busser, S. (2022). Brain injury effects on the respiratory system. Continued.com - Respiratory Therapy, Article 140. Available at www.continued.com/respiratory-therapy